Continuing Education Activity
The transabdominal plane (TAP) block is a regional anesthesia technique used for postoperative pain management in abdominal wall procedures, providing somatic analgesia to the anterior and lateral abdominal walls. This activity describes the anatomy, techniques, approaches, and complications of the TAP block and highlights the role of the interprofessional team in evaluating and managing patients who undergo this procedure. It emphasizes the importance of teamwork in ensuring optimal care and improved outcomes for patients undergoing abdominal surgeries.
Objectives:
Identify the indications for a transabdominal plane block.
Differentiate between various transabdominal plane block techniques to choose the most appropriate approach for specific patient needs.
Assess and promptly manage any complications or side effects associated with transabdominal plane blocks, such as infection, bleeding, or nerve injury, to ensure patient safety.
Collaborate with the interprofessional team, including surgeons, anesthesiologists, advanced care practitioners, nurses, and pharmacists, to ensure seamless integration of transabdominal plane blocks into the patient's overall care plan.
Introduction
Regional anesthesia for abdominal wall procedures can be performed using a variety of peripheral nerve blocks. These blocks are typically ultrasound (US) guided and involve injecting a local anesthetic (LA) solution into interfascial planes. US-guided transversus abdominis plane (TAP) block involves the injection of LA in between the transversus abdominis (TA) and internal oblique (IO) muscles. The TAP block can also be targeted using anatomical landmarks at the level of the Petit triangle. This interfascial plane contains the intercostal, subcostal, iliohypogastric, and ilioinguinal nerves. These nerves give sensation to the anterior and lateral abdominal wall and the parietal peritoneum, providing only somatic and not visceral analgesia.
The TAP block can be used for postoperative analgesia management in open and laparoscopic abdominal surgeries and inpatient and outpatient surgical procedures.[1] Unilateral left- or right-sided blocks are used for unilateral surgical procedures, such as cholecystectomy, appendectomy, nephrectomy, or renal transplants. In contrast, bilateral TAP blocks are used for midline and transverse abdominal incisions, such as umbilical or ventral hernia repair, cesarean deliveries, hysterectomy, and prostatectomy. TAP blocks are part of multimodal pain management for abdominal surgeries, which adds analgesic benefit to patients, reducing postoperative opioid requirements. TAP blocks are typically placed intraoperatively, either before the surgical incision or at the end of the procedure before emergence from anesthesia. The TAP block's efficacy depends on the spread of LA across the interfacial plane. Newer tissue plane blocks, like the quadratus lumborum block, provide somatic and visceral analgesia.
The TAP block has become one of the most common truncal blocks performed for postoperative analgesia after abdominal surgeries. This activity reviews the anatomy of the abdominal wall, the history of the TAP block, classification, approaches, techniques, and complications for this block. It also highlights the indications, contraindications, clinical significance, and materials to perform this block safely.
Anatomy and Physiology
Reviewing the anatomy of the anterior abdominal wall will result in a greater understanding of the neurovascular anatomy within the TAP block. The anterolateral abdominal wall has 4 muscles: the rectus abdominis, external oblique, internal oblique, and transversus abdominis muscles. The TAP anatomical compartment is a plane that is located between the internal oblique and transversus abdominis muscles and contains the T6 to L1 thoracolumbar nerves.
The sensitive innervation of the anterolateral abdominal wall results from the spinal nerves, anterior rami. Immediately after exiting their respective intervertebral foramina, spinal nerves divide into anterior and posterior rami. The anterior rami are split into 2 branches, the anterior and lateral cutaneous nerves. The anterior cutaneous nerve from the T6 to T11 segments gives rise to intercostal (IC) nerves, which supply sensitivity to the skin and muscles of the anterior abdominal wall. The T9 to T11 IC and T12 subcostal (SC) nerves penetrate the transversus abdominis plane compartment posterior to the midaxillary line.
The lower thoracic IC and SC nerves innervate the skin of the infraumbilical area between the midline and midclavicular lines.[2] The L1 lumbar plexus gives rise to ilioinguinal (II) and iliohypogastric (IH) nerves. These nerves provide sensory innervation to the upper hip, groin, and thigh. All these nerve branches travel between the transversus abdominis (TA) and internal oblique (IO) muscles in the TAP compartment.
The first description of the TAP block was accredited to Rafi in 2001, who advocated for the performance of this block by anatomical landmarks at the level of the lumbar triangle of Petit.[3] The Petit triangle edges are conformed by the iliac crest as the inferior edge, the latissimus dorsi as the posterior edge, and the external oblique as the anterior edge. The tip of the triangle is the rib cage.
Traditionally, these landmark blocks have blind endpoints (pops), making their success unpredictable. In 2006, O'Donnell introduced the term TAP block and modified Rafi's original description by advocating for a double pop technique. In 2007, Hebbard et al. proposed using US guidance to identify the intermuscular planes and using the midaxillary line (lateral approach) instead of the triangle of Petit. In 2010, Lee et al. demonstrated that the subcostal approach covered an increased number of dermatomes (4 vs 3 by the lateral approach) and yielded a higher sensory blockade (T8 vs T10).[4][5][6]
Indications
Providing analgesia after an abdominal wall procedure in various abdominal surgeries is an indication of the TAP block. The TAP block can be performed for open abdominal surgeries and laparoscopic procedures. The block is an easier and less risky substitute for epidural anesthesia in postoperative pain control for abdominal surgeries.
- A unilateral block is used for a one-sided procedure, such as appendectomy, cholecystectomy, nephrectomy, and renal transplant.
- Bilateral blocks are used for midline and transverse abdominal incisions, such as ventral hernia repair, umbilical hernia repair, exploratory laparotomy, colostomy closure, cesarean delivery, hysterectomy, radical retropubic prostatectomy, bariatric surgery, inguinal hernia repair, and laparoscopic surgery.
TAP blocks can also play a role in chronic pain management.[7][8][9]
Contraindications
This procedure is contraindicated in the following circumstances:
- Patient refusal
- Infection over the site of injection
- Allergy to LA
Caution should be maintained in patients on therapeutic anticoagulation, pregnant patients, and others where anatomical landmarks are difficult to distinguish (such as very thin or deconditioned patients or older individuals).
Equipment
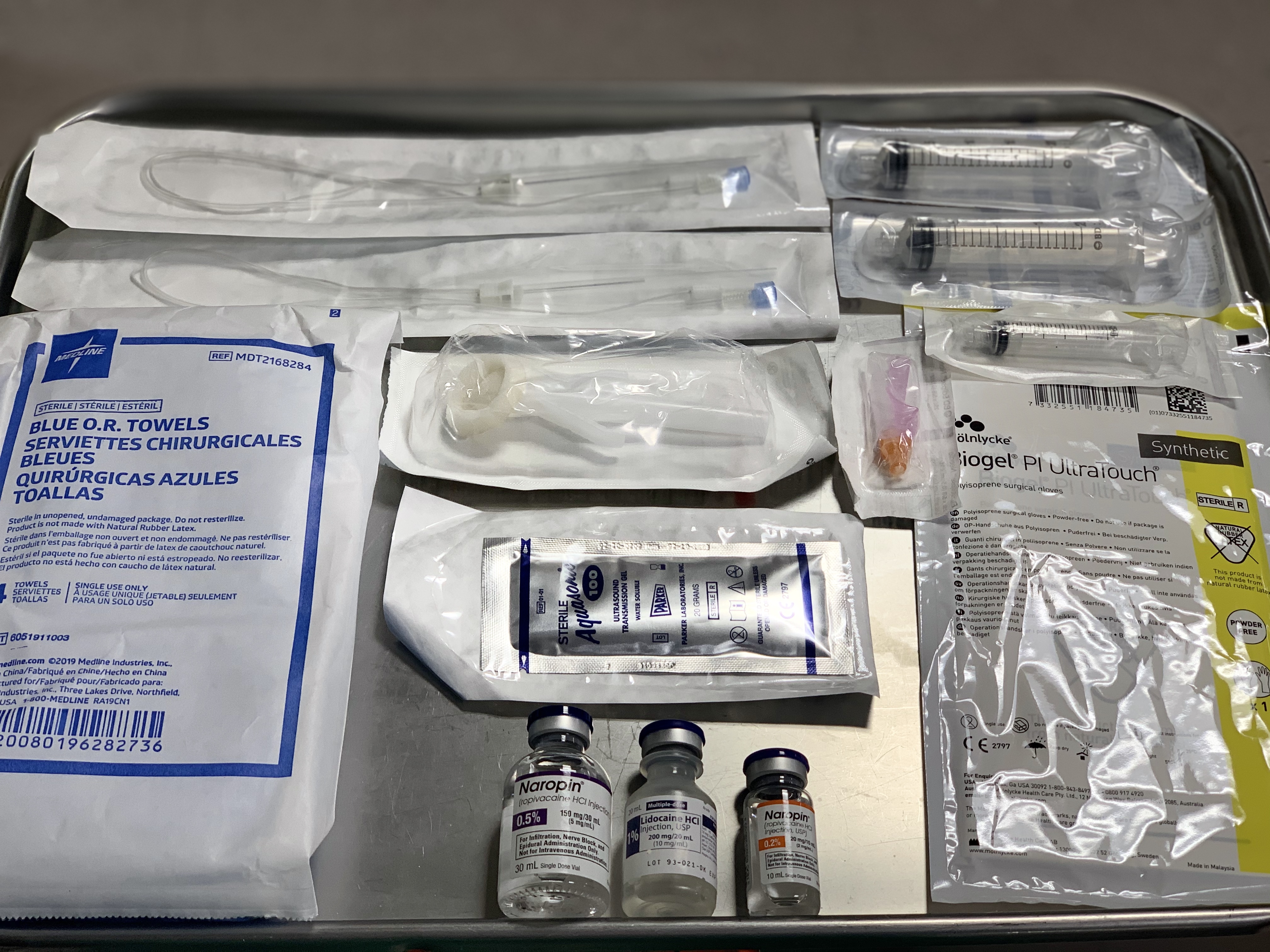
The following are the necessary materials to perform a TAP block (see Image. Regional Anesthesia Tray for TAP Block):
- Ultrasound machine with a linear transducer. (Sometimes, a curvilinear transducer might be needed if the patient is obese or if performing a posterior approach.)
- Sterile ultrasound probe cover sleeve
- Sterile ultrasound gel
- Sterile towels
- Sterile gloves
- Antiseptics for skin disinfection, such as chlorhexidine 2%
- Nerve block needle (50 mm to 100 mm, 20-gauge to 21-gauge needle) with tubing
- Two 20 mL syringes containing the LA solution
- LA agent: ropivacaine, bupivacaine, or liposomal bupivacaine
- One 5 mL syringe containing lidocaine for skin LA (if the patient is awake)
- Basic physiological monitors: EKG, pulse oximeter, and blood pressure monitor
- If performing the block in an awake patient: A 5 mL syringe with needle for skin infiltration with lidocaine 1% LA
Personnel
A skilled medical provider with regional anesthesia training, such as an anesthesiologist, should perform the TAP block. A second health care provider or nurse is required to perform a preprocedure time out and to assist during the procedure with the US and the injection of LA while the anesthesiologist positions the needle and directs when and how much to inject.
Preparation
Before performing a TAP block, the healthcare professional must:
- Obtain informed consent for the procedure, discussing the possible risks, benefits, and alternatives for pain management.
- Verify that the patient has IV access before the procedure.
- Verify the patient is being monitored using continuous EKG and pulse oximetry, and blood pressure cuff cycling every 5 minutes.
- Position the patient supine and uncover the abdomen.
- Prepare the area with an antiseptic solution to clean the skin of the anterolateral area of the abdomen (from the costal margin to the iliac crest).
- After prepping the area and letting the antiseptic dry, place sterile towels surrounding the border of the procedural field.
- Before starting the procedure, a preprocedural time-out should occur, including patient name, medical record number, date of birth, allergies, the procedure that will be performed, and laterality.[10]
Technique or Treatment
There are several TAP block techniques based on how the TAP block compartment is identified:
- The original landmark-guided TAP block at the level of the Petit triangle
- The US-guided TAP block that can be found anatomically in the subcostal, lateral, and posterior approach
- The laparoscopic-guided TAP block involves visualizing from inside the abdominal cavity and sensing 2 "pops" or loss of resistance with the needle from outside the abdomen during surgery.
The US-guided technique is considered the gold standard in TAP blocks because it is easy for the operator to acquire US images and safe for the patient to have the procedure performed under direct visualization of the needle prior to the injection of LA. For these techniques, the patient should be positioned supine, except for slight lateralization for the posterior approach in some cases. A high-frequency linear or curvilinear US transducer should be placed in the abdomen with gel for adequate contact and transmission of the US waves.[5]
The skin and subcutaneous fat are the most superficial layers in the visualized US image. There are 3 muscular layers, from superficial to deep: the external oblique, followed by the internal oblique (IO), and lastly, the transversus abdominis (TA) muscle. The IO muscle is usually the thickest muscle layer in most patients, while the TA muscle is the thinnest. If the layer borders are uncertain, increase the ultrasound's depth to confirm the bowel beneath the TA muscle. Scanning posteriorly, the IO and TA muscles show the 2 layers come together to form the thoracolumbar fascia. Scanning medially, the aponeurosis of the 3 muscle layers comes together to form the rectus sheath. Upon identifying the TAP compartment with the US probe, infiltrate the patient's skin using lidocaine (if the patient is awake) and penetrate the skin with the block needle using an in-plane technique, making sure to visualize the needle tip on US throughout its entire trajectory. Upon entering the plane between the IO and the TA muscles, the LA is slowly injected after negative aspiration of blood. The TAP compartment will begin to separate, hydrodissect, or "unzip" as the LA is injected, pushing the TA muscle down (see Image. Hydrodissection of TAP Compartment). Usually, an injection of 15 mL to 20 mL of LA is recommended for each side of an adult patient. The dose and volume depend on the patient's weight as well as the concentration of the LA. The spread of LA along the TAP compartment is responsible for the success of the block. Studies have shown that the efficacy of the block is improved when injecting 15 mL or more.[11]
There are 3 approaches for US-guided TAP block to target the compartment anatomically:
- Subcostal approach: Targets the TAP compartment in the anterior abdominal wall beneath the costal margin. The high-frequency probe should be located in the lower margin of the rib cage between the xiphoid process and the anterosuperior iliac spine at the level of the anterior axillary line. The objective is to deposit the LA in the plane between the TA muscle and the posterior rectus sheath. The needle should be inserted above the rectus abdominis muscle and advanced until it is positioned between the anterior edge of the TA muscle and the posterior rectus sheath[2]. This area is covered by T6 to T9 dermatomes, blocking the anterior cutaneous nerves. The anterior approach provides analgesia for open or laparoscopic cholecystectomy surgeries (see Image. Subcostal TAP Block Approach).
- Lateral approach: Targets the TAP compartment in the lateral abdominal wall. The high-frequency probe should be located in the midaxillary line between the bony prominences of the subcostal margin and the iliac crest. The 3 muscular layers in the abdominal wall should be visualized. The objective is to deposit the LA in the plane between the TA and IO muscles. The needle should be inserted and advanced until it reaches the TAP plane. This area is covered by T10 to T12 dermatomes, blocking the anterior cutaneous nerves. The lateral approach provides analgesia for most abdominal surgeries, including laparoscopic surgery, open appendectomy, ventral hernia repair, umbilical hernia repair, exploratory laparotomy, colostomy closure, cesarean delivery, hysterectomy, bariatric surgery, radical retropubic prostatectomy among others (see Image. Lateral TAP Block Approach).
- Posterior approach: Targets the TAP compartment at the level of the lumbar triangle of Petit or the anterolateral aspect of the quadratus lumborum muscle. The high-frequency probe should be located in the midaxillary line and then displaced lateral and posteriorly to the end limit of the 3 muscular layers. The objective is to deposit the LA in the plane among the TA muscle and the IO muscle but in the posterior end limit of the TAP plane.[1] The needle should be inserted in the midaxillary line and advanced posteriorly until it reaches the TAP plane. This area is covered by T9 to T12 dermatomes, blocking the anterior and lateral cutaneous nerves. The posterior approach provides analgesia for nephrectomies, renal transplants, and others (see Image. Posterior TAP Block Approach).
Other Blocks
TAP block vs Rectus Sheath Block: The rectus sheath block targets the compartment between the rectus abdominis muscle and the posterior rectus muscle sheath. The high-frequency probe should be placed in a transverse orientation below the costal margin on the lateral edge of the rectus abdominis muscle at the upper one-third of the rectus muscle, where the TA muscle extends medially and provides a layer of safety between the compartment and the peritoneum to prevent peritoneal injection of LA. The US image should visualize the rectus muscle, the posterior rectus sheath, and the TA muscle below the rectus sheath. The LA should separate the sheath from the muscle body, the rectus muscle should be displaced upward, and the TA muscle should be displaced downward. The LA should extend in both directions, cephalad and caudal, within the sheath. The rectus sheath block provides analgesia for midline vertical or paramedian abdominal incisions such as exploratory laparotomy incisions, umbilical surgeries, and umbilical port incisions for laparoscopic surgery.
TAP block vs Ilioinguinal and Iliohypogastric block: The ilioinguinal and iliohypogastric block targets these 2 nerves within the TAP compartment above the inguinal ligament. The high-frequency probe should be placed cephalad and medial to the anterior superior iliac spine (ASIS) in the direction of a line between the umbilicus and the ASIS. US images will depict the 3 layers of abdominal muscles. In the TAP compartment, the ilioinguinal and iliohypogastric nerves may or may not be visible as echogenic structures along with the deep circumflex iliac artery. This is a block that requires less volume of LA, approximately 5 mL to 10 mL. The ilioinguinal and iliohypogastric block provides analgesia for inguinal hernia surgeries.
TAP block vs Quadratus Lumborum block: The quadratus lumborum (QL) block targets the fascial plane in the posterior surface of the QL muscle. There are 3 types of QL blocks, each targeting a fascial plane defined by different muscles. The QL block covers more dermatomes with better cephalad and posterior spread than the TAP block. QL blocks provide visceral and somatic analgesia, probably due to paravertebral and epidural spread. For this block, a curvilinear probe should be located in an axial position at the level of the umbilicus and the anterior axillary line. Visualize the 3 layers of abdominal muscles and trace laterally until the IO and TA muscles merge, becoming the transversalis fascia (TF). The QL muscle is deep to the transversalis fascia. The fascia extends posteriorly as the thoracolumbar fascia (TLF). The needle should be inserted in-plane with the curvilinear probe at the level of the posterior axillary line in between the costal margin and the iliac crest bony prominences.
- The QL1 block targets the superficial anterolateral corner of the QL muscle, where the TF meets the QL muscle; after injection of LA, the QL muscle should be displaced downwards. This block only covers T12 to L1 dermatomes, blocking the subcostal, iliohypogastric, and ilioinguinal nerves. The QL1 block provides analgesia for abdominal surgeries below the umbilicus.
- The QL2 block targets the superficial posterolateral corner of the QL muscle, posterior to the QL muscle but outside the middle layer of the TLF; after injection of LA, the QL muscle should be displaced downwards. This block covers T4 to T12-L1 dermatomes, blocking the anterior and lateral cutaneous nerves. The QL2 block provides analgesia for abdominal surgeries either above or below the umbilicus.
- The QL3 block targets the compartment between the QL and the psoas major muscles. The needle should go through the QL muscle, also called transmuscular QL block; after injection of LA, the QL muscle and psoas muscle should hydrodissect and separate. This block covers T4 to T12-L1 dermatomes, blocking the anterior and lateral cutaneous nerves. The QL3 block provides analgesia for abdominal surgeries either above or below the umbilicus.
Finally, and alternatively, surgeon-administered TAP blocks within the surgical field have also been described.[12][13]
1. The anterior approach provides analgesia for open or laparoscopic cholecystectomy surgeries (see Image. Subcostal TAP Block Approach).
2. Note the angle of the needle in the image demonstrating the posterior block approach (see Image. Posterior TAP Block Approach).
3. Characteristic vertically oriented, thickened collagen bundles are seen in the superficial dermis at point A in the slide (see Image. Lichen Simplex Chronicus).
Complications
Complications related to TAP blocks are rare. Some complications reported in the literature include:
- Bowel perforation
- Hematoma
- Liver/Spleen laceration
- Intrahepatic injection
- Intraperitoneal injection of LA
- Retroperitoneal hematoma due to vascular injury
- Transient femoral nerve blockage
- Local infection
- Intravascular injection
- Systemic toxicity from LA
Utilizing US guidance rather than anatomical landmarks is recommended to increase the success rate and minimize these complications. There have been minimal reported complications after the universal implementation of the US-guided technique for the TAP block.[14]
Neurological injury is rare in TAP blocks because these are field blocks, relying on the high volume of the LA injected to facilitate adequate blockade of the nerves in the compartment rather than targeting a specific nerve. If a neurologic injury occurs, it might be from direct nerve trauma from the needle, hematoma, or local infection. Excessive needle insertion, especially in thin, older, or deconditioned patients, may also lead to complications such as visceral trauma, vascular injury, intraperitoneal injection, or intrahepatic injection.[15]
Case reports have also described transient femoral nerve palsy when some LA injected for the TAP block could trail on the fascia iliaca below the inguinal ligament, producing an inadvertent blockage of the femoral nerve. If this incident happens, the surgical team should be made aware, and the patient has to be advised regarding the potential risk of falls.[16] LA injection within the TAP block is within an interfascial plane that is well vascularized; the reason why the operator should perform careful aspiration before injecting a LA is to avoid an accidental vascular puncture and intravascular injection that might lead to LA systemic toxicity (LAST) which is a rare but known complication of the TAP block.
Clinical Significance
With the advent of US guidance, there has been a surge in popularity for the TAP block, now highly used for postoperative analgesia management following abdominal surgery. The TAP block is part of the multimodal analgesia management for abdominal surgeries that includes using at least 2 non-opioid analgesic agents (eg, acetaminophen, a nonsteroidal anti-inflammatory drug, gabapentinoids, IV lidocaine, ketamine or LA wound infiltration in addition to oral or parental opioids.[17]
The benefits of the TAP block include a reduction in opioid requirements in the postoperative period and a decrease in postoperative nausea and vomiting, but no difference in visual analog pain scale scores.[18] The TAP block has become essential because of its safety profile, ease of performance, and effectiveness for pain control in a multimodal pain management approach with increased patient satisfaction and reduced contribution to the world opioid crisis.[19]
Enhancing Healthcare Team Outcomes
A multidisciplinary team approach is essential to perform regional anesthesia blocks, including the TAP block.
- The informed consent should be ethically obtained by the health care provider, who should explain to the patient the risks, benefits, alternatives, possible side effects, and complications of the TAP block.
- An appropriate time out must be performed before the start of the procedure. The nurse should do this in the presence of the anesthesiologist, surgeon, if possible, OR personnel, and patient listening if awake. The time out should consist of confirming out loud the patient's name, medical record number, date of birth, allergies, block to be performed, laterality, and dose/amount of LA to be injected (especially for pediatric patients).
- The team-based procedure must include the surgeon, anesthesiologist, nurses, pharmacist, surgical assistant, and the rest of the OR personnel.
- It is essential to maintain interpersonal communication with all team members, especially with the surgeon, to evaluate the suitability of the block being performed, the location and size of the incision, and to continue discussions when performing the block before induction of anesthesia (with an awake patient) after induction or before emergence. After the block is performed, it is imperative to notify the surgeon and all the team members how much LA was injected to avoid extra local infiltration of LA by the surgeon to prevent an episode of LAST and enhance patient safety.
- The pharmacist will prepare the LA concentration and dose the clinician ordered, provide a safe dose below the maximum dose per weight, have an intralipid emulsion available in case of a LAST episode, and be available if there are any medication-related questions by the team.
- Nurses will perform the preprocedure time out and assist during the procedure.
- In the event of the block being performed on an awake patient, the patient should be aware of the possible sensations he/she might feel, and the operator should maintain verbal contact with the patient at all times throughout the procedure to monitor for any complications such as potential nerve injury, visceral perforation, or LAST. The patient's vital signs should be monitored in real-time during the procedure.
- The operator and assistant should take extreme caution when handling sharps between one another, as accidental needle sticks may occur. Needles should be disposed of in designated sharp bins in the procedure area.
- Documentation of the procedure should include informed consent, date, time, procedure location, block technique, LA used, volume and concentration of injectate, equipment used, ultrasound images, and documentation of any complications.
Adhering to these standards will elevate patient care, enhance procedural outcomes and patient safety, and boost overall team performance.
Nursing, Allied Health, and Interprofessional Team Interventions
Nurses are very important for the successful performance of the TAP block. Their roles include:
- Verify that the patient signed the informed consent for the procedure
- Verify the correct side of the procedure (if unilateral)
- Set up the US, syringes, needles, medications, and all materials necessary to perform the block
- Place all the monitors preprocedure (EKG, pulse oximetry, and blood pressure monitors)
- Position and prepare the patient for the procedure
- Perform the preprocedure time out
- Assist the operator if necessary during the procedure
Nursing, Allied Health, and Interprofessional Team Monitoring
The nurse should be available before, during, and after the TAP block to monitor the patient, including:
- Verify preprocedure that a crash cart is close and available with resuscitative equipment.
- Monitor the patient's vital signs and clinical status during and after the procedure.
- After the procedure, when in the recovery room, the nurse should assess the patient's block site for bleeding, hematoma, or abdominal distension.