[1]
Lawrence DA, Branson B, Oliva I, Rubinowitz A. The wonderful world of the windpipe: a review of central airway anatomy and pathology. Canadian Association of Radiologists journal = Journal l'Association canadienne des radiologistes. 2015 Feb:66(1):30-43. doi: 10.1016/j.carj.2014.08.003. Epub
[PubMed PMID: 25623009]
[2]
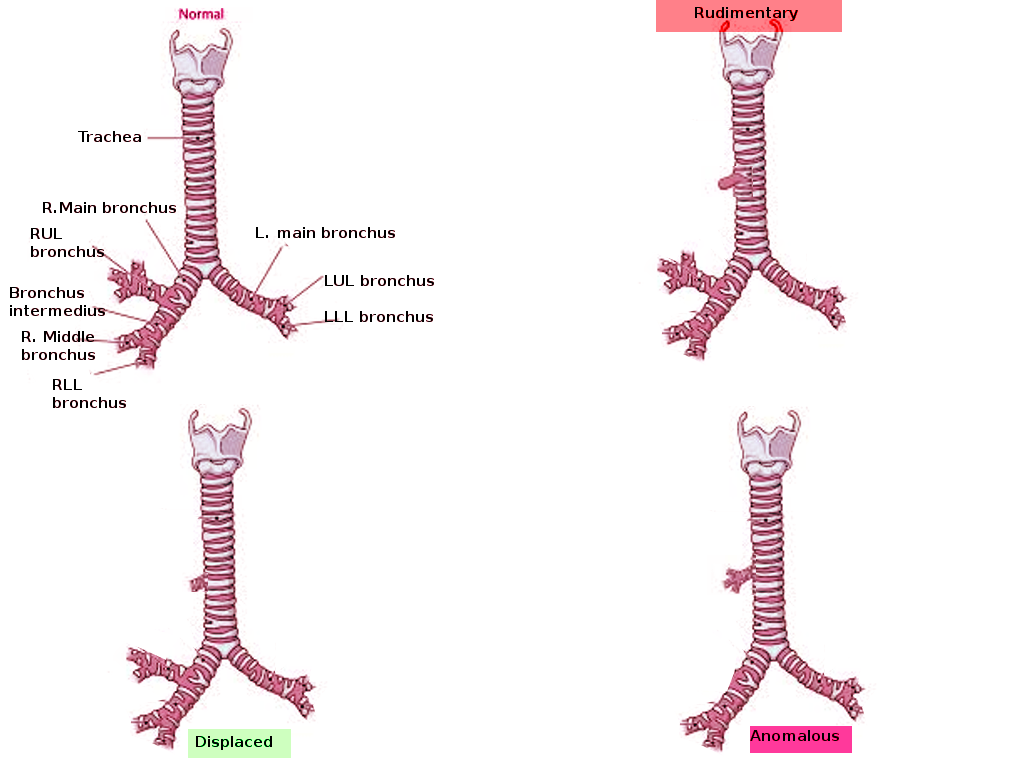
Chassagnon G, Morel B, Carpentier E, Ducou Le Pointe H, Sirinelli D. Tracheobronchial Branching Abnormalities: Lobe-based Classification Scheme. Radiographics : a review publication of the Radiological Society of North America, Inc. 2016 Mar-Apr:36(2):358-73. doi: 10.1148/rg.2016150115. Epub 2016 Feb 1
[PubMed PMID: 26824513]
[4]
Setty SP, Michaels AJ. Tracheal bronchus: case presentation, literature review, and discussion. The Journal of trauma. 2000 Nov:49(5):943-5
[PubMed PMID: 11086789]
Level 3 (low-level) evidence
[5]
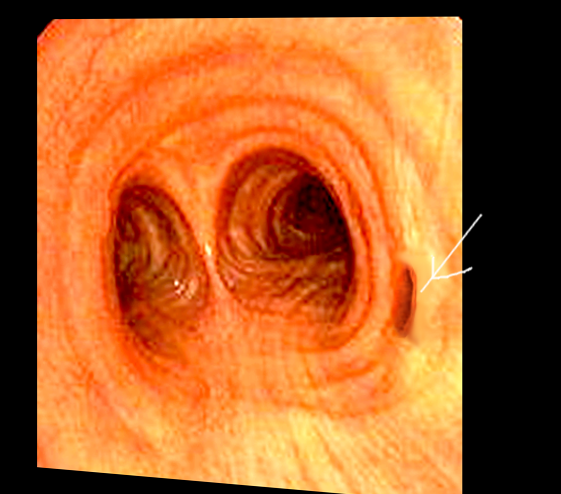
Pérez Ruiz E, Caro Aguilera P, Valdivielso AI, Sanchís Cárdenas S, Martínez García Y, Pérez Frías J. Tracheal bronchus diagnosed in children undergoing flexible bronchoscopy. Paediatric respiratory reviews. 2018 Sep:28():26-30. doi: 10.1016/j.prrv.2018.03.009. Epub 2018 May 19
[PubMed PMID: 29914745]
[6]
Ghaye B, Szapiro D, Fanchamps JM, Dondelinger RF. Congenital bronchial abnormalities revisited. Radiographics : a review publication of the Radiological Society of North America, Inc. 2001 Jan-Feb:21(1):105-19
[PubMed PMID: 11158647]
[6]
Qi S, Zhang B, Yue Y, Shen J, Teng Y, Qian W, Wu J. Airflow in Tracheobronchial Tree of Subjects with Tracheal Bronchus Simulated Using CT Image Based Models and CFD Method. Journal of medical systems. 2018 Mar 1:42(4):65. doi: 10.1007/s10916-017-0879-0. Epub 2018 Mar 1
[PubMed PMID: 29497841]
Level 2 (mid-level) evidence
[7]
Tuon FF, Siqueira AM, Litvoc MN, Lopes MH. Tuberculosis and tracheal bronchus. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2007 Sep:11(5):467-8
[PubMed PMID: 17331782]
[8]
Tamura M, Murata T, Kurumaya H, Ohta Y. Leiomyoma of an accessory tracheal bronchus. The Annals of thoracic surgery. 2004 Dec:78(6):2163-5
[PubMed PMID: 15561062]
[9]
Nicolaou N, Du Plessis A. Squamous carcinoma arising from a true tracheal bronchus: Management and case report. International journal of surgery case reports. 2015:6C():256-8. doi: 10.1016/j.ijscr.2014.12.005. Epub 2014 Dec 19
[PubMed PMID: 25549955]
Level 3 (low-level) evidence
[10]
Ismail M, Vukasinov P, Liao HI, Mir P. Hemoptysis in a previously healthy elderly patient with an unrecognized tracheal bronchus: A case report. Respiratory medicine case reports. 2017:22():34-35. doi: 10.1016/j.rmcr.2017.06.002. Epub 2017 Jun 2
[PubMed PMID: 28649488]
Level 3 (low-level) evidence
[11]
Berrocal T, Madrid C, Novo S, Gutiérrez J, Arjonilla A, Gómez-León N. Congenital anomalies of the tracheobronchial tree, lung, and mediastinum: embryology, radiology, and pathology. Radiographics : a review publication of the Radiological Society of North America, Inc. 2004 Jan-Feb:24(1):e17
[PubMed PMID: 14610245]
[12]
Lai KM, Hsieh MH, Lam F, Chen CY, Chen TL, Chang CC. Anesthesia for patients with tracheal bronchus. Asian journal of anesthesiology. 2017 Dec:55(4):87-88. doi: 10.1016/j.aja.2017.09.002. Epub 2017 Oct 26
[PubMed PMID: 29122588]
[13]
Lee HL, Ho AC, Cheng RK, Shyr MH. Successful one-lung ventilation in a patient with aberrant tracheal bronchus. Anesthesia and analgesia. 2002 Aug:95(2):492-3, table of contents
[PubMed PMID: 12145079]
[14]
Lee DK, Kim YM, Kim HZ, Lim SH. Right upper lobe tracheal bronchus: anesthetic challenge in one-lung ventilated patients -A report of three cases-. Korean journal of anesthesiology. 2013 May:64(5):448-50. doi: 10.4097/kjae.2013.64.5.448. Epub 2013 May 24
[PubMed PMID: 23741569]
Level 3 (low-level) evidence
[15]
Baden W, Schaefer J, Kumpf M, Tzaribachev N, Pantalitschka T, Koitschev A, Ziemer G, Fuchs J, Hofbeck M. Comparison of imaging techniques in the diagnosis of bridging bronchus. The European respiratory journal. 2008 May:31(5):1125-31. doi: 10.1183/09031936.00045907. Epub
[PubMed PMID: 18448507]
[16]
Suzuki M, Matsui O, Kawashima H, Takemura A, Matsubara K, Hayashi N, Koda W, Shibata Y. Radioanatomical study of a true tracheal bronchus using multidetector computed tomography. Japanese journal of radiology. 2010 Apr:28(3):188-92. doi: 10.1007/s11604-009-0405-5. Epub 2010 May 1
[PubMed PMID: 20437128]
[17]
Jugpal TS, Garg A, Sethi GR, Daga MK, Kumar J. Multi-detector computed tomography imaging of large airway pathology: A pictorial review. World journal of radiology. 2015 Dec 28:7(12):459-74. doi: 10.4329/wjr.v7.i12.459. Epub
[PubMed PMID: 26753061]
[18]
Laroia AT, Thompson BH, Laroia ST, van Beek E Jr. Modern imaging of the tracheo-bronchial tree. World journal of radiology. 2010 Jul 28:2(7):237-48. doi: 10.4329/wjr.v2.i7.237. Epub
[PubMed PMID: 21160663]
[19]
Schweigert M, Dubecz A, Ofner D, Stein HJ. Tracheal bronchus associated with recurrent pneumonia. The Ulster medical journal. 2013 May:82(2):94-6
[PubMed PMID: 24082287]
[20]
Moon YJ, Kim SH, Park SW, Lee YM. The implications of a tracheal bronchus on one-lung ventilation and fibreoptic bronchoscopy in a patient undergoing thoracic surgery: a case report. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2015 Apr:62(4):399-402. doi: 10.1007/s12630-014-0293-8. Epub 2014 Dec 16
[PubMed PMID: 25510236]
Level 3 (low-level) evidence
[21]
Conacher ID. Implications of a tracheal bronchus for adult anaesthetic practice. British journal of anaesthesia. 2000 Aug:85(2):317-20
[PubMed PMID: 10992847]
[22]
Rahmanian R, Zheng J, Chadha NK, Kozak FK, Campbell AI, Ludemann JP. False carina: a distinct variant of tracheal bronchus. International journal of pediatric otorhinolaryngology. 2015 Apr:79(4):623-8. doi: 10.1016/j.ijporl.2015.01.023. Epub 2015 Jan 25
[PubMed PMID: 25683591]
[23]
Xu XF, Chen L, Wu WB, Zhu Q. Thoracoscopic right posterior segmentectomy of a patient with anomalous bronchus and pulmonary vein. The Annals of thoracic surgery. 2014 Dec:98(6):e127-9. doi: 10.1016/j.athoracsur.2014.09.059. Epub 2014 Dec 1
[PubMed PMID: 25468123]
[24]
Yurugi Y, Nakamura H, Taniguchi Y, Miwa K, Fujioka S, Haruki T, Takagi Y, Matsuoka Y, Kubouchi Y. Case of thoracoscopic right upper lobectomy for lung cancer with tracheal bronchus and a pulmonary vein variation. Asian journal of endoscopic surgery. 2012 May:5(2):93-5. doi: 10.1111/j.1758-5910.2011.00115.x. Epub
[PubMed PMID: 22776372]
Level 3 (low-level) evidence
[25]
Shih FC, Lee WJ, Lin HJ. Tracheal bronchus. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2009 Mar 31:180(7):783. doi: 10.1503/cmaj.080280. Epub
[PubMed PMID: 19332762]
[26]
Rasooly AJ, Noor S, Ullah S, Baryali AT, Haidary AM. Forty days old infant with Pig Bronchus, presenting with recurrent pneumonia: A Case Report. Pediatric health, medicine and therapeutics. 2023:14():379-383. doi: 10.2147/PHMT.S429852. Epub 2023 Oct 30
[PubMed PMID: 37927398]
Level 3 (low-level) evidence