Continuing Education Activity
Peripheral nerve blocks inhibit the propagation of impulses in nerve terminals to inhibit the perception of pain by the cerebral cortex. Local anesthetics will temporarily block the transmission of pain. The onset, duration, density, and spread of the nerve block may be influenced by the type of local anesthetic given, concentration, and volume. The femoral nerve block anesthetizes the femoral nerve distribution and is utilized for anterior thigh and knee procedures. It can provide effective analgesia with less opioid intake, which consequently reduces the adverse effects from opioid consumption, and promote earlier hospital discharge. This activity describes the technique of a femoral nerve block and highlights the role of the interprofessional team in the management of these patients.
Objectives:
Describe the technique of a femoral nerve block.
Review the complications of a femoral nerve block.
Summarize the indications of a femoral nerve block.
Outline factors affecting the performance and improvement for outcomes of peripheral nerve blocks that require collaboration from all members of the medical team.
Introduction
Peripheral nerve blocks inhibit the propagation of impulses in nerve terminals to inhibit the perception of pain by the cerebral cortex. Local anesthetics will temporarily block the transmission of pain.[1] The type of local anesthetic given, concentration, and volume may affect the onset, duration, density, and spread of the nerve block. The femoral nerve block anesthetizes the femoral nerve distribution, and surgeons use it for anterior thigh and knee procedures. It can provide effective analgesia with less opioid intake, which consequently reduces the adverse effects from opioid consumption, and promote earlier hospital discharge.[2]
Anatomy and Physiology
The femoral nerve is among the largest branches of the lumbar plexus. The femoral nerve arises from the ventral rami of the L2, L3, and L4 spinal nerves, and enters the femoral triangle inferior to the inguinal ligament. The femoral nerve is the most lateral of the structures within the triangle, which also contains the femoral artery and femoral vein at its medial end.
The femoral nerve splits into anterior and posterior divisions that originate near the level of the circumflex artery. The anterior division gives rise to the medial femoral cutaneous nerve and innervates the sartorius muscle. The posterior division gives rise to the saphenous nerve and provides innervation to quadriceps femoris muscle.[3]
In addition to motor innervation, the femoral nerve provides sensation to the anterior thigh and knee and the medial lower extremity below the knee. The saphenous nerve is a femoral nerve branch that is directly responsible for sensation to the medial lower leg and foot. The saphenous nerve can be blocked separately at the level of the adductor canal, and several more distal sites. The adductor canal is a musculoaponeurotic tunnel found in the mid-thigh and extends from the femoral triangle to the adductor magnus.[4] Due to the anatomical connection, the femoral nerve within the femoral triage may potentially be affected by proximal or high-volume adductor canal blocks.[5]
Indications
The femoral nerve block (FNB) is indicated for surgery on the anterior aspect of the thigh. It may also be combined with a sciatic nerve block to provide complete lower extremity coverage below the knee, and additionally with an obturator block to provide complete lower extremity anesthesia. Both single injection and continuous infusions provide pain relief following total knee replacement.[6] Femoral nerve block is also useful for analgesia in femoral neck fractures, femur fractures, and patellar injuries. Femoral nerve block may be utilized alone or as part of a multi-modal pain management plan.[7]
Contraindications
Absolute contraindications include patient refusal, inability to cooperate, and severe allergy to local anesthetic agents. Relative contraindications include current infection at the site of local injection, patients on anticoagulation and antithrombotic medications, and patients with bleeding disorders. The physician should discuss the possibility of further nerve damage in patients with pre-existing nerve damage or those who may be susceptible to nerve injury (such as severe diabetes, trauma to nerves, etc.).[1]
Equipment
Proper equipment is necessary for the femoral nerve block procedure. Sterile protocol with antiseptic solution (such as chlorhexidine scrub), sterile gloves, face mask, and hospital cap, should be maintained. A 20- or 22-gauge, 50- to 100-mm, short-bevel, insulated needle (that may be stimulating and/or echogenic), lidocaine 1% with a 25 gauge needle to anesthetize at the insertion site, and 20 mL syringe for local anesthetic would be part of a standard nerve block kit. For an ultrasound-guided technique, an ultrasound machine with a linear transducer, sterile ultrasound probe cover, insulated needle, and ultrasound gel are all requirements. Local anesthetic options may include long-acting amide agents, such as bupivacaine 0.5%, levobupivacaine 0.5%, or ropivacaine 0.5%, or intermediate-acting amide agents, such as mepivacaine 0.5% or lidocaine 0.5%.[8] Preservative-free formulations for peripheral nerve block should be utilized.
Personnel
A medical professional with training in regional anesthesia should perform the nerve block. An additional person may be needed to assist with the local anesthetic injection. A nurse with background or familiarity in regional anesthesia is a definite asset.
Preparation
The provider obtains informed consent in accordance with hospital policy. Importantly, a motor and sensory exam should take place, and any pre-existing neurological damage documented.
Before the start of the procedure, the following American Society of Anesthesiology (ASA) standard monitors should be placed on the patient: pulse oximetry, continuous electrocardiography, and blood pressure (intermittent every 3 to 5 minutes or continuous monitoring). Reliable intravenous access and intravenous fluids should be confirmed. There should be immediate availability of oxygen, resuscitation equipment, and medications. A 20% lipid emulsion should be readily accessible in case of local anesthetic toxicity.[9]
The patient should be in the proper position before femoral nerve placement. The patient should be supine. The correct lower limb should be straightened, slightly abducted, and externally rotated.[1]
The pannus may require additional retraction to better expose the groin area.
Lastly, a Time Out is strongly recommended prior to the start of the procedure for final confirmation. Light sedation may be administered at the direction of the proceduralist based on institutional policy.
Technique or Treatment
Ultrasound-Guided Technique
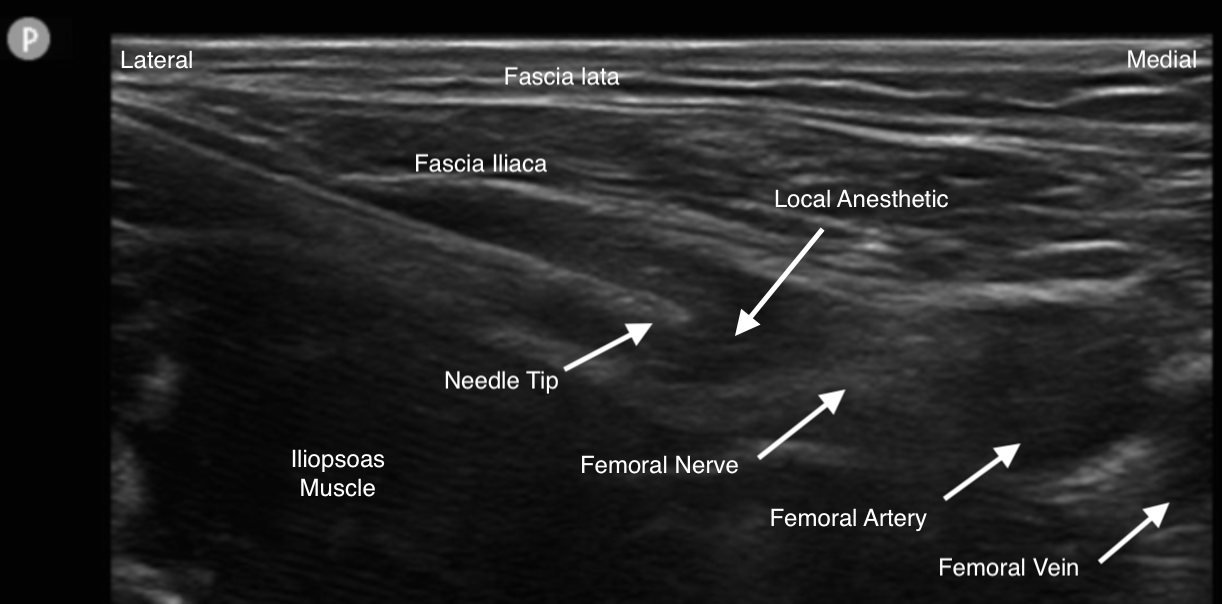
The femoral artery and vein are medial to the femoral nerve at the level of the inguinal ligament. When using ultrasound, the transducer is placed transversely at the inguinal crease, and the femoral vessels are located. If multiple arteries are present (i.e., superficial and deep femoral arteries), then slide the probe proximally until only the common femoral artery is visualized along with its associated femoral vein. Immediately lateral to the femoral vessels, the femoral nerve classically appears as a hyperechoic wedge or ovoid structure. The femoral nerve is superficial to the iliopsoas muscle group; and it is deep to the fascia lata and fascia iliaca, respectively (refer to Figure).
Once the femoral nerve and relevant neighboring structures have been identified, a lidocaine wheal is administered before the block needle insertion into the tissue, and the needle tip is advanced below the fascia iliaca towards the femoral nerve. Either an in-plane or out-of-plane approach may be used, depending on the proceduralist’s preference. Confirming negative aspiration for heme is recommended before injection to avoid intravascular injection. The ultrasound monitor will show the spreading of local injection around the nerve.[10] Caution is necessary with unusually high injection pressure or nerve expansion with injection, which may indicate intraneural injection.[11]
Landmark and Nerve-Stimulation Technique
The inguinal ligament is identified between the anterior superior iliac spine and pubic tubercle. The femoral artery can be palpated just below the femoral crease. The needle is inserted approximately 1 cm lateral to the femoral artery pulse in a cephalad direction. The expected depth of the femoral nerve is 2 to 4 cm (though may be variable depending on body habitus), and can be combined with a nerve-stimulation technique for a more precise location.
A nerve stimulator may be connected to a stimulating block needle to help identify the femoral nerve. The stimulator is set to a current density of 0.8 to 1 mA with a frequency of 2 Hz and a pulse duration of 0.1 milliseconds. The needle enters at an angle of 30 to 45 degrees to the skin in a cephalad direction. Once the expected patellar twitch is confirmed, the current is slowly decreased. If the motor response is obliterated between 0.3 to 0.5 mA, then the needle tip is likely sufficiently near the nerve without being intraneural, and the provider may inject local anesthetic after confirming negative aspiration.[12] Nerve stimulator technique is an option in combination with ultrasound guidance.
Complications
There are always risks involved when performing a peripheral nerve bock. The following are complications that can result: nerve injury, allergic reaction, hematoma, infection, and local anesthetic systemic toxicity.[7] Also, patients should understand the risk of the nerve block not working successfully, and other forms of analgesia should be available. There is a small risk of temporary or permanent nerve injury, which can be caused by direct needle injury or intraneural injection. Given the possibility of complications, resuscitation equipment must be nearby in the event of local anesthetic systemic toxicity.[13]
A 20% lipid emulsion administration is effective for local anesthetic toxicity. A bolus dose of 1.5 mL/kg based on the lean body mass of lipid emulsion should be given over 1 minute and followed by an infusion of 0.25 mL/kg/min. This continuous infusion should continue until reaching hemodynamic stability. If hemodynamic stability is not obtained, then another bolus of 1.5 mL/kg (for a maximum of two total doses of 20% lipid emulsion), followed by a continuous infusion at the increased dose of 0.5 mL/kg/min should be considered.[14] The 10% lipid emulsion in propofol should never be used as an alternative source for lipid emulsion therapy.
Clinical Significance
The femoral nerve block includes motor and sensory nerves. Patients will exhibit difficulty with mobility due to the weakness of the quadriceps muscle. Mitigation of this motor weakness is achievable by using a reduced concentration of local anesthetics. Importantly, patients should not be ambulating without assistance following femoral nerve block as they may be at risk for falling.
Enhancing Healthcare Team Outcomes
The performance of peripheral nerve blocks requires collaboration from all members of the interprofessional medical team. The regionalist and nursing staff should work together to provide the highest level of care and benefit to the patient.
Although a relatively safe procedure, preparation, proper monitoring, and immediate accessibility of emergency equipment and medications should be ready in the event of any adverse events;, if anesthesia is in use in any form, a nurse dedicated to the monitoring of the patient should be on the case. Also, resuscitative equipment should always be in the room, even before starting the procedure. The pharmacist should verify agent selection and dose for the procedure, as well as ensuring no drug-drug interactions by performing medication reconciliation, and reporting to the surgical team any concerns.
Open interprofessional communication and collaboration between the staff is the optimal way to avoid morbidity and improve outcomes when performing femoral nerve block. [Level 5]