Definition/Introduction
Vital signs are an objective measurement of the essential physiological functions of a living organism. They have the name "vital" as their measurement and assessment is the critical first step for any clinical evaluation. The first set of clinical examinations is an evaluation of the vital signs of the patient. Triage of patients in an urgent/prompt care or an emergency department is based on their vital signs as it tells the physician the degree of derangement that is happening from the baseline. Healthcare providers must understand the various physiologic and pathologic processes affecting these sets of measurements and their proper interpretation. If we use a triage method where we select patients without determining their vital signs, it may not give us a reflection of the urgency of the patient's presentation.[1] The degree of vital sign abnormalities may also predict the long-term patient health outcomes, return emergency department visits, and frequency of readmission to hospitals, and utilization of healthcare resources.
Traditionally, the vital signs consist of temperature, pulse rate, blood pressure, and respiratory rate. Even though there are a variety of parameters that may be useful along with the traditional four vital sign parameters, studies have only found pulse oximetry and smoking status to have significance in patient outcomes.[2] Pulse oximetry sometimes helps to clarify the patient's physiological functions, which would sometimes be unclear by checking just the traditional vital signs. The inclusion of smoking status has the premise that the patient will be provided counseling by the provider on quitting smoking. In the past, some health care systems in the United States had used "pain as the fifth vital sign'. This approach is being abandoned due to the unintended opioid crisis that the country is currently facing.[3]
Issues of Concern
Patient safety is a fundamental concern in any health care organization, and early detection of any clinical deterioration is of paramount importance whether the patient is in the emergency department or on the hospital floor. The early detection of changes in vital signs typically correlates with faster detection of changes in the cardiopulmonary status of the patient as well as up-gradation of the level of service if needed. Vital signs assessment currently uses electronic equipment, but there is evidence that, outside of the intensive care units, respiratory rate assessment through observation, leading to insufficient, subjective, and unreliable results.[4]
In a case-control study conducted by Rothschild and colleagues, early warning criterion among patients on the medical floor, the presence of respiratory rate over 35/min (OR=31.1) was most strongly associated with a life-threatening adverse event.[5] Early warning score (EWS) tools, mostly using vital sign abnormalities, are critical in predicting cardiac arrest and death within 48 hours of measurement, even though the effect on in-hospital health outcomes and utilization of resources remains unknown.[5]
It seems intuitive that the higher the frequency of vital sign measurement, the faster the chances of clinical deterioration are detected. There is variability between institutes within and across nations depending on the acuity of clinical condition, any active intervention carried out, the amount of staff availability, cost issues, organizational practices, and leadership styles. The weighted average score deduced from the vital sign measurements (i.e., an early warning score) is used to determine the timing of the next observation sets.[4][5]
Clinical Significance
Temperature
Body temperature is a variable, which is complex as well as nonlinear and is affected by many sources of internal and external variables. The normal body temperature for a healthy adult is approximately 98.6 degrees Fahrenheit/37.0 degrees centigrade. The human body temperature typically ranges from 36.5 to 37.5 degrees centigrade (97.7 to 99.5 degrees Fahrenheit.[6] Body temperature is regulated in the hypothalamus in a narrow thermodynamic range and maintained to optimize the synaptic transmission of biochemical reactions.[7]
Clinical decisions, especially in the pediatric population regarding the investigation and management, are based on the results of temperature measurement alone. Whereas at one end, missing that the patient's fever is severe or detecting a falsely positive fever reading can cause the patient to receive wrongful management. Galileo was the first scientist to uncover the concept of thermometers that began in the 16th century. In the year, 1709 Daniel Fahrenheit developed an alcohol-filled thermometer as well as a mercury-filled thermometer.[8]
Health care providers use the axillary, rectal, oral, and tympanic membrane most commonly to record body temperature, and the devices most commonly used are the electronic and infrared thermometers. They can monitor temperature at different sites, and each site has its range as well as advantages and disadvantages. As clinicians, the understanding of these site-specific differences is crucial. For example, the oral temperature, which is the most commonly used method, is considered very convenient and reliable. Here we place the thermometer under the tongue and close the lips around it. The posterior sublingual pocket is the area that gives the highest reliability. The other commonly used methods are tympanic temperature, where the thermometer where we insert the thermometer into the ear canal, and the axillary temperature where we place the thermometer in the axilla while adducting the arm of the patient. Both these sites are convenient but generally considered less accurate and hence not recommended.[8]
For measuring the rectal temperature, the thermometer is inserted through the anus into the rectum after applying a lubricant. This method is very inconvenient, but since it measures the internal measurement, it is very reliable. It is usually considered the "gold standard" method of recording temperature. Gut temperature, measured with an ingested pill, also gives readings close to the rectal temperature. Besides the site, the time of day is an essential factor leading to variability in the temperature record, secondary to the circadian rhythm. The inability to consider this physiological diurnal variation of temperature can lead to the wrong conclusion that an individual's temperature suggests a disease state when it is a normal temperature at that time of day. There is also a variation of the body temperature in a regularly cycling female, referred to as the "circamensal" rhythm. Understanding of this rhythm is paramount in teaching patients, trying to conceive about the fertile period of the cycle. Besides the change with diurnal variation and menstrual variation, a person's relative physical fitness and age can affect the degree of temperature change during a day. Studies show that younger patients and fitter record larger temperature amplitudes, while older and less fit people record lesser amplitude changes.[9] Some studies have demonstrated a seasonal variation in body temperature; we need more research in this regard to reach a definitive conclusion.[9]
Pulse Rate
The most common sites of measuring the peripheral pulses are the radial pulse, ulnar pulse, brachial pulse in the upper extremity, and the posterior tibialis or the dorsalis pedis pulse as well as the femoral pulse in the lower extremity. Clinicians measure the carotid pulse in the neck. In day-to-day practice, the radial pulse is the most frequently used site for checking the peripheral pulse, where the pulse is palpated on the radial aspect of the forearm, just proximal to the wrist joint. Parameters for assessment of pulse include its rate, rhythm, volume, amplitude, and rate of increase, besides its symmetry The rate of the pulse is significant to measure for assessing the physiological and pathological processes affecting the body. The normal range used in an adult is between 60 to 100 beats/minute with rates above 100 beats/minute and rates below 60 beats per minute, referred to as tachycardia and bradycardia, respectively. The age-specific heart rate given for the pediatric age range appears in table -2.
Assessing whether the rhythm of the pulse is regular or irregular is essential. The pulse could be regular, irregular, or irregularly irregular. Changes in the rate of the pulse, along with changes in respiration are called sinus arrhythmia. In sinus arrhythmia, the pulse rate becomes faster during inspiration and slows down during expiration. Irregularly irregular pattern is more commonly indicative of processes like atrial flutter or atrial fibrillation. We should also be checking for the radial and the femoral pulse simultaneously. If there is any delay between the pulses, it could indicate conditions like the coarctation of the aorta. Assessing the volume of the pulse is equally essential. A low volume pulse could be indicative of inadequate tissue perfusion; this can be a crucial indicator of indirect prediction of the systolic blood pressure of the patient. If we can palpate the radial pulse, the systolic blood pressure is generally more than 80 mmHg. If we can palpate the femoral pulse, the systolic blood pressure is more than 70 mmHg, and if we can palpate the carotid pulse, the systolic blood pressure is more than 60 mmHg.[10] Checking for symmetry of the pulses is important as asymmetrical pulses could be seen in conditions like aortic dissection, aortic coarctation, Takayasu arteritis, and subclavian steal syndrome. Besides the above-stated parameters, amplitude and rate of increase is also an important consideration. Low amplitude and low rate of increase could be seen in conditions like aortic stenosis, besides weak perfusion states. High amplitude and rapid rise can be indicative of conditions like aortic regurgitation, mitral regurgitation, and hypertrophic cardiomyopathy.
Respiratory Rate
The respiratory rate is the number of breaths per minute. The normal breathing rate is about 12 to 20 breaths per minute in an average adult. In the pediatric age group, it is defined by the particular age group. Parameters important here again include rate, depth of breathing, and pattern of breathing. Rates higher or lower than expected are termed as tachypnea and bradypnea, respectively. Tachypnea is described as a respiratory rate of more than 20 breaths per minute that could occur in physiological conditions like exercise, emotional changes, or pregnancy. Pathological conditions like pain, pneumonia, pulmonary embolism, asthma, foreign body aspiration, anxiety conditions, sepsis, carbon monoxide poisoning, and diabetic ketoacidosis can also present with tachypnea. Bradypnea described as ventilation less than 12 breaths per minute can be seen due to worsening of any underlying respiratory condition leading to respiratory failure or due to usage of central nervous system depressants like alcohol, narcotics, benzodiazepines, or metabolic derangements. Apnea is the complete cessation of airflow to the lungs for a total of 15 seconds. It appears in cardiopulmonary arrests, airway obstructions, the overdose of narcotics, and benzodiazepines.
The depth of breathing is also a crucial parameter. Hyperpnea is described as an increased depth of breathing and is seen during exercise and in anxiety states, lung infections, and congestive heart failure. Hyperventilation, on the other hand, is described as both increased in the rate and depth of breathing and can again be seen in anxiety states like anxiety or due to exercise but is also seen in pathological conditions like diabetic ketoacidosis or lactic acidosis. The term hypoventilation describes the decreased rate and depth of ventilation. This condition results from excessive sedation, metabolic alkalosis, and in instances of obesity hypoventilation syndrome.
The pattern of breathing also gets affected in various conditions and indicates the underlying pathology. Biot respiration is a condition where there are periods of increased rate and depth of breathing, followed by periods of no breathing or apnea. These can vary in length of time. This pattern is suggestive of raised intracranial pressure as in space-occupying lesions of the skull or conditions like meningitis. Cheyne-Stokes respiration is a peculiar pattern of breathing where there is an increase in the depth of ventilation followed by periods of no breathing or apnea. This presentation occurs in conditions of raised intracranial pressure but is also seen with excessive usage of sedatives and worsening congestive heart failure. Kussmaul breathing refers to the increased depth of ventilation, although the rate remains regular. This presentation is in patients with renal failure and diabetic ketoacidosis. Orthopnea refers to difficulty in respiration occurring on lying horizontal but gets better when the patient sits up or stands It is seen characteristically in congestive heart failure. Paradoxical ventilation refers to the inward movement of the abdominal or chest wall during inspiration, and outward movement during expiration, which is seen in cases of diaphragmatic paralysis, muscle fatigue, and trauma to the chest wall.
Blood Pressure
Blood pressure is an essential vital sign to comprehend the hemodynamic condition of the patient. Unfortunately, though, there are a lot of inter-person variabilities when measuring it. Many times, the basic measurement techniques are not followed and lead to erroneous results.
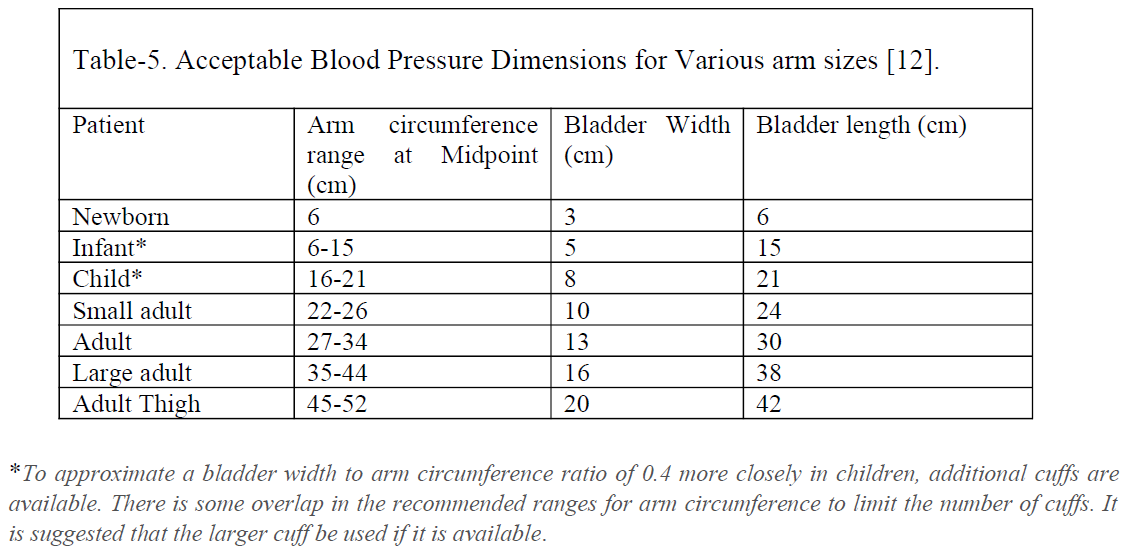
All healthcare providers should be aware of making sure all the essential pre-requisites are met before checking the blood pressure of the patient. The patient should not have taken any caffeinated drink at least one hour before the testing and should not have smoked any nicotine products at least 15 minutes before checking the pressure. They should have emptied their bladder before checking the blood pressure. Full bladder adds 10 mmHg to the pressure readings. It is advisable to have the patient be seated for at least five minutes before checking their blood pressure. This step takes care of or at least minimizes the higher readings that could have occurred secondary to rushing in for the clinic appointment. The providers should not be having a conversation with the patient while checking his blood pressure. Talking or active listening adds 10 mmHg to the pressure readings. The patient’s back and feet should be supported, and their legs should be uncrossed. Unsupported back and feet add 6 mmHg to the pressure readings. Crossed legs add 2 to 4 mmHg to the pressure readings. The arm should be supported at the heart level. Unsupported arm leads to 10 mmHg to the pressure readings. The patient’s blood pressure should get checked in each arm, and in younger patients, it should be tested in an upper and lower extremity to rule out the coarctation of the aorta. Using the correct cuff size is very important. Smaller cuff sizes give falsely high, and larger cuff sizes give a falsely lower blood pressure reading.[11]
Nursing, Allied Health, and Interprofessional Team Interventions
Variability of Vital Signs in the Geriatric Age Group
Since vital signs are an indication of the changes in physiological processes, they tend to change with age. With age, core body temperature tends to be lower, and the ability of the body to change with different kinds of stressors becomes minimized. Even subtle variation from the core body temperature can be a significant finding as fever in an older patient often indicates a more severe infection and is associated with increased rates of life-threatening consequences.[12]
There can be a decrease in response to changes in the oxygen and carbon dioxide at the molecular level along with anatomical changes resulting due to stiffness of muscles and compliance of the chest wall. Respiratory rate sometimes might be the most neglected of the vital signs reported in hospitalized patients but is more sensitive than other vital signs in picking up a critically ill patient.[13]
The aging blood vessels also lead to higher arterial stiffness, leading to higher systolic blood pressure and increased pulse pressure. There is also the issue of orthostatic hypotension due to decreased autonomic responsiveness. This response becomes exaggerated with the use of polypharmacy and reduced fluid intake. Thus, it is imperative to check orthostatic vitals in this population. Resting heart rate, in contrast, is often observed to increase with age due to deconditioning and autonomic dysregulation.[14]
Limitations of Vital Signs
Accurately measuring vital signs is a clinical skill that needs time and practice to refine. A review of literature is abundant about the inter-observer variability observed and reported secondary to lack of this skill. Clinicians should be wary of this and always re-check the vital signs themselves if there is a profound or unexpected change. Clinics and organizations should continuously strive to check and educate their nursing and ancillary staff to sharpen these skills.