Introduction
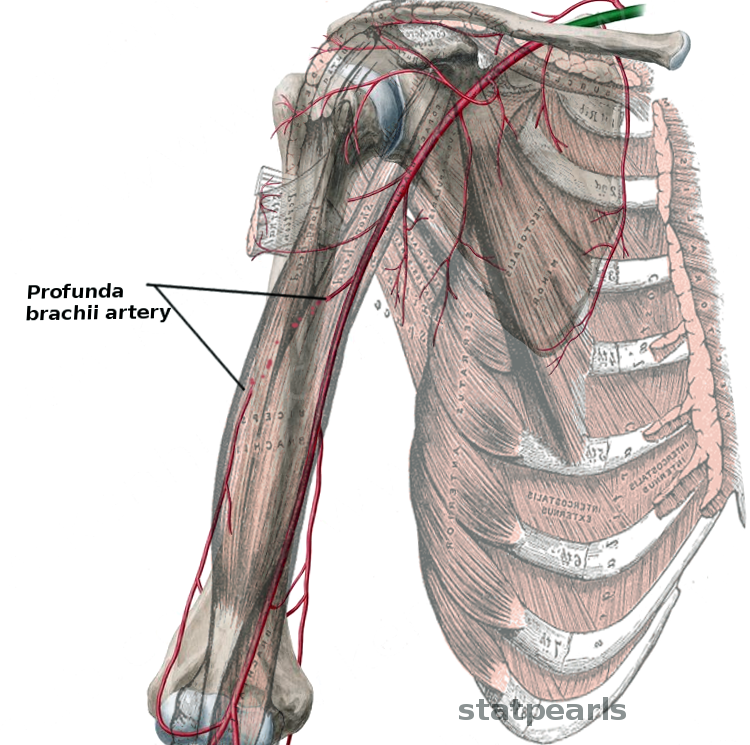
The profunda brachii artery, also called the "deep brachial artery," is the first and largest branch of the brachial artery (see Image. Profunda Brachii Artery). This blood vessel bifurcates from the posterior portion of the brachial artery below the teres major's inferior border. It then traverses the triangular interval, entering the posterior compartment of the arm along with the radial nerve.
Once in the posterior compartment, the profunda brachii artery gives off a branch that connects with the posterior circumflex humeral artery. The profunda brachii artery then continues inferiorly along the radial sulcus (aka radial groove), branching into the radial and middle collateral arteries at a point inferior to the latissimus dorsi.
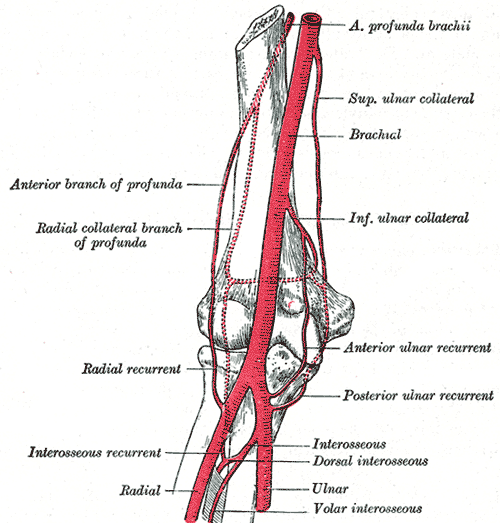
The radial collateral artery further divides into the anterior and posterior radial collateral arteries.[1][2] The anterior radial collateral artery anastomoses with the radial recurrent artery. The middle and posterior radial collateral arteries fuse with the recurrent interosseous artery.
The profunda brachii is essential to upper extremity circulation because of its vast arterial connections. This article focuses on this important blood vessel.
Structure and Function
Formation Of The Profunda Brachii Artery
Blood supply to the upper extremity is traceable back to the aorta. On the right side, the aorta gives off the brachiocephalic artery, which gives rise to the right subclavian artery. On the left side, the aorta empties directly into the left subclavian artery. The subclavian artery becomes the axillary artery at the lateral border of the 1st rib. The axillary artery continues as the brachial artery at the lower border of the teres major muscle.
The axillary artery is the principal artery supplying the upper limb. This blood vessel is traditionally divided into 3 parts. The part number gives a clue to the number of branches each one possesses.
- 1st part: This portion of the axillary artery runs between the first rib's lateral border and the medial boundary of the pectoralis minor. The first part is protected by the axillary sheath and has one branch, the superior thoracic artery.
- 2nd part: This segment runs on the posterior surface of the pectoralis minor and has 2 branches. The first is the thoracoacromial artery, which passes medial to the pectoralis minor. The second is the lateral thoracic artery, which travels lateral to the pectoralis minor. The thoracoacromial arterial trunk has 4 branches, which are better remembered by the mnemonic "PAC-D." These branches are the pectoral, acromial, clavicular, and deltoid arteries.
- 3rd part: This section travels from the pectoralis minor's lateral margin to the inferior portion of the teres major. Its 3 branches are the subscapular artery and the anterior and posterior circumflex humeral arteries.The subscapular artery bifurcates into the circumflex scapular and thoracodorsal arteries. The anterior and posterior circumflex humeral arteries encircle the surgical neck of the humerus.
The axillary artery gives rise to the brachial artery at the inferior border of the teres major muscle. The brachial artery has 5 major branches critical to upper extremity circulation. These blood vessels are listed below in order of branching:
- Profunda brachii artery
- Superior ulnar collateral artery
- Inferior ulnar collateral artery
- Ulnar artery
- Radial artery
The profunda brachii is the most proximal of the 5 brachial artery branches. This blood vessel arises from the posterior portion of the brachial artery distal to the inferior margin of the teres major. From here, the profunda brachii runs alongside the radial nerve, entering the posterior compartment of the arm through the triangular interval. The triangular interval is the anatomic space bounded by the teres major muscle superiorly, the long head of the triceps brachii muscle medially, and the humerus laterally.[3]
The medial and lateral intermuscular septa divide the arm into the posterior and anterior compartments. The posterior arm compartment is where the profunda brachii gives off its first branch—a small artery that fuses superiorly with the posterior circumflex humeral artery. This branch provides additional circulation to the deltoid muscle.
The profunda brachii artery continues inferiorly and laterally around the radial sulcus, lying between the humerus and the lateral head of the triceps brachii muscle. It divides into the middle and radial collateral arteries distal to the inferior margin of the latissimus dorsi.
The middle collateral artery courses inferiorly in the medial head of the triceps brachii muscle. This blood vessel anastomoses with the inferior ulnar collateral and recurrent interosseous arteries at a level superior to the ulna's olecranon process. The fusion of the middle collateral and inferior ulnar collateral arteries contributes to the anastomoses around the elbow.[1]
The radial collateral artery continues in the radial sulcus until it pierces the lateral intermuscular septum. This artery then bifurcates into the anterior and posterior radial collateral arteries at the level of the brachioradialis muscle's origin. The posterior radial collateral artery travels within the lateral intermuscular septum. This blood vessel connects with the recurrent interosseous artery at the level of the olecranon process.[4] Meanwhile, the anterior radial collateral artery passes anterior to the lateral intermuscular septum and fuses with the radial recurrent artery at the level of the lateral humeral epicondyle.[1][2]
The profunda brachii artery is important because it supplies the humeral shaft and the posterior arm muscles. This blood vessel also participates in the elbow's anastomotic network (see Image. Elbow Joint Arterial Anastomosis). The relationships between the arm's arterial branches must be noted during procedures like brachial plexus repair, brachial plexus blocks, and surgery of the axillary structures.[5]
Histology Of The Profunda Brachii Artery
The profunda brachii is classified histologically as a muscular artery. Muscular arteries bridge elastic arteries to arterioles. The defining characteristics of muscular arteries are their tunica media's thick, smooth muscle layers and prominent internal elastic laminae.
Embryology
The developing limb buds' blood supply comes from the intersegmental arteries, a group comprised of 30 arteries arising from the embryonic aorta. The lateral branch of the 7th intersegmental artery forms the primary axial artery. This blood vessel becomes the brachial artery and its branches, which include the profunda brachii artery.
Nerves
The radial nerve, which arises from the C5 to T1 nerve roots, provides motor and sensory impulses to portions of the upper extremity. This nerve initially traverses the triangular interval alongside the profunda brachii artery until the latter divides into the radial and middle collateral arteries. Inferior to this level, the radial nerve takes a more superficial course, following the anterior radial collateral artery into the anterior arm compartment.
Muscles
Extensive arterial networks supply upper extremity muscles. The profunda brachii artery provides additional circulation to the deltoid, triceps brachii, and anconeus.
Physiologic Variants
Anatomical variations of the different upper extremity arteries are described extensively in the literature. Their rarity can impact surgical outcomes significantly. This section discusses some notable variants.
Profunda Brachii Variations
The profunda brachii artery exhibits variations in its origin and termination. The most common physiologic variant is the anomalous origin of the profunda brachii artery from the axillary artery rather than the brachial artery. Studies report its prevalence to range between 2% and 16.6%.[3]
Brachial Artery Variations
The brachial artery typically divides at the mid-humeral level into the radial and ulnar arteries. However, some individuals exhibit different brachial artery branching patterns.
One variant has the brachial artery branching out as high as the corachobrachialis level. In this variant, the brachial artery divides into a medial branch, termed the "brachioradial artery," and a lateral brachioulnar artery. This bifurcation occurs distal to the origin of the nutrient artery and the corachobrachialis. The medial ulnar and radial arteries cross each other at the apex of the cubital fossa, and the median nerve lies between these structures.[6]
A very short brachial artery was once reported in a 45-year-old male cadaver. The brachial artery bifurcation into the ulnar and radial arteries occurred at a higher level than usual—the middle third of the humerus. The radial artery diverged medially, and the ulnar artery laterally at the bifurcation point. Inferiorly, the ulnar artery crossed over to the lateral side. The anterior and posterior interosseous arteries branched out directly from the ulnar artery instead of the common interosseous artery. The anterior and posterior recurrent arteries emerged from the ulnar artery at the level of the cubital fossa instead of a more distal location. The radial collateral, middle collateral, and posterior interosseous arteries arose from a common trunk originating more proximally along the ulnar artery.[7]
A high-bifurcating brachial artery may also have the radial artery–producing branches that are supposed to emerge from another. For example, the common interosseus artery may originate from the radial artery instead of the ulnar artery. The profunda brachii artery may arise from the radial artery instead of the brachial artery.[8]
Axillary Artery Variations
The axillary artery may also exhibit atypical branching patterns. In one variant, the superficial brachial, subscapular, and profunda brachii arteries directly bifurcate from the 3rd part of the axillary artery. The circumflex scapular, thoracodorsal, and lateral thoracic arteries diverge from the subscapular artery. The profunda brachii artery continues as the anterior brachial artery at the surgical neck of the humerus. The superficial brachial artery has 2 posterior brachial arteries, both traversing the spiral groove of the humerus along with the radial nerve.[3]
Another variant has a circumflex-subscapular arterial trunk arising directly from the axillary artery. This trunk continues posteriorly as the profunda profunda brachii artery.[9] The axillary artery may also divide into superficial and deep axillary trunks. The superficial axillary artery's deep division gives rise to all the named branches, including the profunda brachii artery.[9] Another variant has the profunda brachii artery branching out from the 3rd part of the axillary artery as a 4th branch and giving rise to the ulnar collateral arteries.[10]
Radial Artery Variations
The radial artery typically branches out from the brachial artery at the level of the cubital fossa. This branching pattern has a prevalence rate of 54%. However, variants with more proximal radial artery bifurcation points have been documented in a Kenyan subpopulation. In these variants, the radial artery may arise from the axillary or proximal or middle third of the brachial artery. Proximally bifurcating brachial arteries are more commonly observed on the right than the left side.[11]
Surgical Considerations
Lateral Arm Flaps
Skin flaps are either free or pedicled. Free skin flaps are totally severed from their native arterial supply, while pedicled ones remain attached to theirs. The posterior radial collateral artery, a branch of the profunda brachii artery, may be used as a vascular pedicle in lateral arm flaps.
Surgeons perform the lateral arm flap to repair deep forearm or hand skin defects. In this procedure, a skin flap with up to 5 cm diameter is taken from the area between the lateral epicondyle and deltoid muscle insertion. The flap is then disconnected from most of its blood supply except at one end where the posterior radial collateral artery is left intact. The area of the defect is then covered with the pedicled flap.[12][13][14]
The Anterolateral Approach To Humeral Shaft Fracture Repair
Humeral shaft fractures may be repaired using plates and screws. Narrow compression plates of size 4.5 mm have been successfully used in repairing such injuries. The arm's unique anatomy makes the anterolateral approach safer than the posterolateral approach.
The profunda brachii artery and radial nerve travel from the posteromedial to the posterolateral aspect of the humerus. The anterolateral approach provides better visibility of these structures than the posterolateral approach, making them easier to identify. Open reduction and internal fixation of humeral shaft fractures using the posterolateral approach are associated with a radial nerve palsy rate of 11.5%.[15][21]
Clinical Significance
Posterior Arm Circulation After A Brachial Artery Injury
The brachial artery ranks as the most commonly injured upper extremity artery and accounts for 28% of all vascular injuries.[16] The location of the injury with respect to the profunda brachii artery's origin, ie, proximal or distal, determines the degree of ischemia in the area supplied by this blood vessel. A proximal injury reduces the profunda brachii artery's ability to support posterior arm circulation. By comparison, a distal injury does not significantly affect the deep artery's function.[17]
Profunda Brachii Artery Pseudoaneurysm
Aneurysms are arterial dilations resulting from the weakening of the 3 blood vessel wall layers. Pseudoaneurysms can be differentiated from aneurysms as they involve only 1 or 2 layers. Arterial pseudoaneurysms of the brachial artery and its branches often result from trauma or infections.
In one reported case, an 8-year-old boy developed a left profunda brachii artery pseudoaneurysm after Kirschner wire repair of a previously sustained left supracondylar humeral fracture. The condition was noted 20 days after the procedure and was documented by CT angiography. Traumatic supracondylar humeral fractures account for approximately 17.9% of pseudoaneurysms in children younger than 16 years.[18]
Other Issues
The terminal branches of the profunda brachii artery have been a topic of great debate. Various sources list only the radial and middle collateral arteries as the profunda brachii's only terminal branches and exclude the anterior and posterior radial collateral arteries. Additionally, these sources state that anastomoses exist between the radial collateral and radial recurrent arteries and between the middle collateral and recurrent interosseous arteries.[19][20]