Introduction
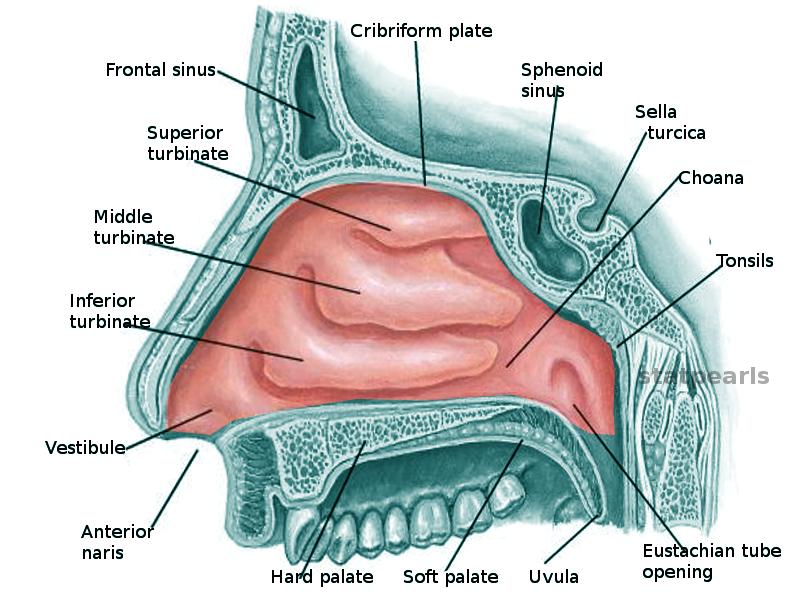
Three pairs of turbinates are commonly described along the lateral walls of the nasal cavity: the superior, middle, and inferior (see Image. Nasal Cavity).[1] The supreme turbinate exists in some individuals, with 8% having unilateral and 80% having bilateral development.[2][3] The turbinates' bony components are called the "conchae." The conchae of the middle, superior, and supreme turbinates are projections of the ethmoid bones. Meanwhile, the inferior turbinate—the largest turbinate—is a separate bone unto itself.
Beneath the attachment of each turbinate to the lateral nasal wall is a space, a meatus, into which drain several different outflow tracts originating in the orbits and paranasal sinuses. Turbinates play an important physiological role by warming and humidifying inspired air and regulating nasal airflow. However, turbinates may also contribute to nasal airway obstruction when inflamed, as in cases of allergy and viral upper respiratory infections. Understanding the anatomy and function of the nasal conchae is crucial when treating nasal and orofacial disorders.
Structure and Function
The nasal turbinates, also known as nasal conchae, are curved, bony structures protruding from the lateral walls of the nasal cavity. The 3 pairs of turbinates are the inferior, middle, and superior turbinates. Some individuals may also have a 4th, smaller pair called the "supreme" or "highest turbinate."[1]
Inferior Turbinate
The inferior turbinate is the largest and is located in the lower part of the lateral nasal wall. The inferior turbinate is a separate bone that articulates with the maxillary, palatine, and ethmoid bones. The inferior turbinate has a robust, scroll-like structure that increases the surface area for air contact.
The inferior meatus, located beneath the inferior turbinate, contains the opening of the nasolacrimal duct, which drains tears from the eye into the nasal cavity. The inferior meatus also contains the Hasner valve, or the plica lacrimalis, a mucosal fold that prevents air reflux from the lacrimal system.
Middle Turbinate
The middle turbinate is positioned above the inferior turbinate, attached to the lateral wall of the nasal cavity. The middle turbinate is part of the ethmoid bone and has a thin, curved bony structure. This turbinate is covered by mucosa with a dense vascular supply and glandular tissue.
The middle meatus, located beneath the middle turbinate, contains the openings of the maxillary, anterior ethmoidal, and frontal sinuses. These openings connect via the hiatus semilunaris, situated just inferior to the ethmoid bulla and posterior to the uncinate process of the ethmoid bone.
Superior Turbinate
The superior turbinate is the smallest of the 3 main turbinates and is located above the middle turbinate. This turbinate is also part of the ethmoid bone and has a similar thin, curved shape. The superior turbinate is covered by mucosa thinner than the inferior and middle turbinates.
The superior meatus, located beneath the superior turbinate, provides drainage for the posterior ethmoidal sinuses. The sphenoethmoidal recess, located posterosuperior to the superior turbinate, drains the sphenoid sinus.
Supreme Turbinate
The supreme (highest) turbinate is located above the superior turbinate. Not all individuals have this structure. Like the other turbinates, the supreme turbinate is part of the ethmoid bone covered by mucosa.
Mucosal Lining
The turbinates are covered by a pseudostratified columnar epithelium, commonly called the respiratory epithelium. This epithelium contains goblet cells that secrete mucus, which traps particles and pathogens. Beneath the mucosal layer lies a submucosal layer of erectile tissue containing venous sinuses. This tissue can swell or shrink to regulate the airflow and resistance within the nasal cavity.
Function
The nasal turbinates have the following crucial functions in the respiratory system:
- Warming and humidifying air: The turbinates ensure that air is adequately warmed and humidified as it passes through the nasal cavity and into the nasopharynx, larynx, and lower respiratory tract. The turbinates' curved, shelf-like bodies protruding from the lateral nasal walls increase the surface area available for air warming and humidification.
- Regulating airflow: The inferior turbinates regulate airflow by swelling and contracting to maintain appropriate moisture levels within the nasal cavity. This process is controlled by the underlying erectile tissue containing venous sinusoids, adjusting turbinate volume based on autonomic stimulation. In most individuals, one inferior turbinate swells while the other contracts, directing most airflow through one nostril at a time. This alternation, known as the "nasal cycle," lasts from half an hour to 6 hours, with longer cycles occurring during sleep.[4]
- Immune function: The inferior turbinates, the first intranasal structures to contact outside air, are pivotal in immune surveillance. Cells in these turbinates can detect the pathogenicity of inhaled particles and trigger immune responses.[5]
- Olfactory function: The middle and superior turbinates, not primarily involved in immune responses, support olfaction. The olfactory neuroepithelium is located at the nasal cavity's apex, the cribriform plate of the ethmoid bone, and along the dorsal aspect of the nasal septum and medial aspects of the superior and middle turbinates. The superior turbinate contributes to the sense of smell in over 80% of the population, while the posterior portion of the middle turbinate contains olfactory neuroepithelium in 30% to 40% of individuals. The supreme turbinate is also likely involved in olfaction due to its location.[6][7]
These functions are essential for maintaining respiratory health and ensuring effective inhalation and detection of environmental particles.
Embryology
The buds of the turbinates appear at week 7 of embryonic development, arising from mesenchymal stem cells, which are heterogeneous, pluripotent cells.[8] The maxilla begins to ossify and enlarge at weeks 9 to 10. The nasal capsule begins to ossify with the inferior turbinates during Weeks 17 to 18. Middle turbinate growth starts during week 20, deriving from the 2nd ethmoturbinal ridge, which is an extension of the lateral wall of the nasal capsule. The superior turbinates begin to ossify from the 3rd and 4th ethmoturbinals after Week 21, and the supreme turbinates come from the 4th and 5th ethmoturbinals. The olfactory fascia, which runs between the nasal cartilages and the olfactory mucosa, also appears to contribute to turbinate development, with turbinate growth directionality significantly impacting nasal cavity formation.[9]
Blood Supply and Lymphatics
The nasal turbinates receive a rich blood supply, primarily derived from branches of both the internal and external carotid arteries. This vascular network is crucial for the functions of the turbinates, including warming, humidifying, and filtering the inhaled air.[10][11]
Arterial Supply
Branches of the external carotid artery supplying the nasal turbinates include the sphenopalatine, greater palatine, and facial arteries. The sphenopalatine artery is the primary source of blood supply to the nasal turbinates. This blood vessel is a terminal branch of the internal maxillary artery, a branch of the external carotid artery. The sphenopalatine artery enters the nasal cavity through the sphenopalatine foramen and provides branches to the lateral nasal wall and the turbinates.
The greater palatine artery is another branch of the internal maxillary artery that also contributes to the blood supply of the inferior turbinate. This artery ascends through the greater palatine canal to the incisive foramen, where it anastomoses with the sphenopalatine artery. The facial artery gives rise to the superior labial artery, which contributes to the blood supply of the anterior nasal cavity, including the anterior parts of the turbinates.
The ophthalmic artery, a branch of the internal carotid artery, provides the anterior and posterior ethmoidal arteries. The anterior ethmoidal artery supplies the anterior and superior parts of the nasal septum and the anterior parts of the superior and middle turbinates. The posterior ethmoidal artery supplies the superior parts of the nasal cavity, including the superior turbinate and part of the middle turbinate.
Detailed Turbinate Blood Supply
The superior turbinate is primarily supplied by branches of the posterior ethmoidal artery (from the ophthalmic artery) and the posterior septal branches of the sphenopalatine artery. The middle turbinate is perfused anteriorly by the anterior ethmoidal artery (from the ophthalmic artery) and posteriorly by the posterior lateral nasal branches of the sphenopalatine artery.
The inferior turbinate is primarily supplied posteriorly by the posterior lateral nasal branches of the sphenopalatine artery. The anterior portion is perfused by an anastomosis between the anterior lateral nasal artery (a branch of the facial artery) and the anterior ethmoidal artery.
Venous Drainage
Venous drainage of the nasal turbinates follows the arterial pathways. Anteriorly, blood drains into the facial vein. Superiorly, blood empties into the cavernous sinus. Posteriorly, blood drains into the pterygoid plexus, which further drains into the external jugular vein. Some venous blood also reaches the cavernous sinus and internal jugular vein via communicating branches.[12]
The Woodruff plexus is located on the lateral nasal wall at the posterior aspect of the inferior turbinate. This submucosal network of veins is frequently injured during turbinoplasty and is the primary cause of posterior epistaxis (nosebleeds), which accounts for 5% to 10% of nasal bleeding cases.
Lymphatic Drainage
Lymphatic drainage of the nasal turbinates occurs through the lateral pharyngeal and retropharyngeal lymph nodes.[13] Both sets of nodes ultimately drain into larger lymphatic vessels that empty into the deep cervical lymph nodes, situated near the internal jugular vein in the neck. From there, lymphatic fluid eventually returns to the bloodstream via the thoracic or right lymphatic duct.
Nerves
The autonomic nervous system innervates the nasal cavity, particularly the turbinates. Competition between sympathetic and parasympathetic stimulation determines the region's secretomotor and vasodilatory activity. The nerve pathways in this area are described below.
Sympathetic Innervation
The sympathetic innervation of the nasal turbinates begins in the central nervous system and follows a specific pathway to reach the target tissues in the nasal cavity. The journey of sympathetic fibers starts in the hypothalamus, which is responsible for the autonomic regulation of various bodily functions and provides preganglionic innervation to different body regions, including the turbinates. From the hypothalamus, the preganglionic sympathetic fibers descend through the brainstem and enter the spinal cord. The nerves travel down to the thoracic level, specifically the upper thoracic segments (T1-T4).
The sympathetic chain fibers exit the spinal cord via the white rami communicantes and enter the sympathetic chain via the paravertebral ganglia. The fibers ascend within the sympathetic chain to synapse in the superior cervical ganglion, located at the 2nd and 3rd cervical vertebrae level, and exit through the gray rami communicantes.
After synapsing in the superior cervical ganglion, the postganglionic sympathetic fibers proceed along a complex path. The postganglionic fibers form a plexus around the internal carotid artery known as the carotid plexus. Some fibers travel along the internal carotid artery and form the deep petrosal nerve. The deep petrosal nerve then joins the greater petrosal nerve (a parasympathetic nerve) to form the Vidian nerve or the nerve of the pterygoid canal. This nerve carries both sympathetic and parasympathetic fibers. The sympathetic fibers pass through the pterygopalatine ganglion without synapsing and continue into the nasal cavity.
Parasympathetic Innervation
The parasympathetic innervation of the nasal turbinates follows a distinct pathway starting from the brainstem. The parasympathetic pathway begins in the superior salivatory nucleus in the pons. Preganglionic parasympathetic fibers exit the brainstem along with the facial nerve, which is responsible for various facial motor and sensory functions in the face. The greater petrosal nerve arises as the facial nerve traverses the temporal bone. This nerve carries the preganglionic parasympathetic fibers and travels through the hiatus of the facial canal.
The greater petrosal nerve joins the deep petrosal nerve (which carries sympathetic fibers) to form the Vidian nerve. The Vidian nerve then passes through the pterygoid canal. The Vidian nerve reaches the pterygopalatine ganglion, located in the pterygopalatine fossa. Here, the preganglionic parasympathetic fibers synapse with postganglionic neurons.
After synapsing in the pterygopalatine ganglion, the postganglionic parasympathetic fibers follow various branches to reach their target tissues. The postganglionic fibers travel along several branches of the maxillary nerve (a branch of the trigeminal nerve) to innervate the nasal cavity. These branches include the nasopalatine, posterior superior nasal, and greater and lesser palatine nerves. The fibers innervate the mucosal lining of the nasal cavity and the turbinates, providing parasympathetic control over the nasal glands and blood vessels.
Somatosensory Innervation
Beyond autonomic innervation, somatic and sensory functions in the turbinates are critical and are carried out by the olfactory neuroepithelium and trigeminal nerve.[14][15] The olfactory neuroepithelium is located in the superior, supreme, and middle turbinates, allowing dissolved particulate odorants to bind with olfactory receptors. The signals are transmitted through the cribriform plate of the skull base via the olfactory projections of the 1st cranial nerve to the olfactory cortex of the ventral forebrain, contributing significantly to the human sense of taste.
The maxillary and ophthalmic branches of the trigeminal nerve, via the sphenopalatine and nasociliary nerves, respectively, provide somatic sensory innervation. This sensory function is essential for people to feel airflow through the nose. The absence of this sensation can be distressing. Somatic fibers within the nose are highly sensitive. Prolonged slight pressure, such as from a septal deviation contacting a turbinate, can cause substantial discomfort, leading to rhinogenic headache (Sluder syndrome). Treatment may involve lateralizing the turbinate or performing septoplasty to correct the deviation.
Physiologic Variants
The ethmoid bone exhibits significant structural variability in terms of the number of nasal turbinates and pneumatization. Most individuals are born with at least 3 pairs of turbinates, with the middle and superior arising from the ethmoid bone and the inferior turbinate comprising an independent bone. The supreme turbinate, a small bony process superior to the superior turbinate, is not generally clinically significant and, therefore, is not consistently described in the literature. This turbinate may be present bilaterally, unilaterally, or not at all, and its presence is more common in certain ethnic groups.[3]
The form of the other turbinates also varies, with pneumatization of one or both middle turbinates occurring in 30% to 70% of patients. However, pneumatization of the inferior or superior turbinates is rare.[16] Bifidity of the turbinates has also been described but is uncommon.[17]
Surgical Considerations
Surgery within the nasal cavity typically involves the turbinates, which can be either the surgical targets or dissection landmarks. The middle and superior turbinates represent important waypoints during endoscopic sinus surgery. The middle meatus houses the outflow tracts of the anterior ethmoid, maxillary, and frontal sinuses. The ethmoid bulla contains many anterior ethmoid cells and the uncinate cells' process under which lies the lacrimal sac. The middle turbinate, therefore, guides surgical planning involving access to these structures.
The basal lamella of the middle turbinate divides the anterior and posterior ethmoid sinuses. This lamina serves as a milestone on the path to the sphenoid sinus. The sphenoid sinus can be accessed via several different approaches, but the superior turbinate represents a major landmark for locating the sphenoid ostium, which uniformly lies medial to the superior turbinate.[18] The superior turbinate is often removed during sinus surgery when locating and enlarging the sphenoid ostium, but the middle turbinate is generally left intact because of its consistent relationship with so many nearby structures that an experienced sinus surgeon can use to orient rapidly, even in revision cases.
Removal of all or part of the inferior turbinate is common because of its role in nasal obstruction. Inferior turbinate hypertrophy in allergic rhinitis is often managed with intranasal steroid and antihistamine sprays. Surgical reduction of the inferior turbinates is necessary when medical management provides insufficient symptomatic relief, particularly in cases of compensatory inferior turbinate hypertrophy, which occurs in the setting of a deviated nasal septum. When the nasal septum deviates significantly to one side, the inferior turbinate on the concave side of the deviation often hypertrophies markedly to provide airflow regulation through that side of the nasal passage. In these cases, the soft tissue is engorged with blood, and the bone itself gains significant volume.[19]
Turbinoplasty, as the procedure to reduce the size of the turbinates is known, may be performed using many methods, from lateralizing the turbinates by outfracturing them to removing them partially or entirely. Most surgeons currently perform some combination of debulking and outfracturing either under local or general anesthesia when combined with septoplasty or rhinoplasty. An effective turbinoplasty in the correct surgical candidate should improve the patient's nasal obstruction symptom evaluation score by 35 to 40 points on a 100-point scale, substantially relieving the obstruction.[20][21]
Common turbinoplasty methods currently employed include radiofrequency ablation, electrocautery, mechanical microdebridement, and turbinate incision to access and remove a portion of the bony concha. The remainder of the turbinate is typically lateralized, leaving as much mucosa intact as possible to avoid damaging the nose's ability to secrete mucus and humidify the inspired air.
The mucosa also contains sensory nerves that allow the nose to feel airflow. When excessive damage to intranasal mucosal surfaces occurs, often due to overly aggressive turbinoplasty or turbinectomy, the nerves can no longer feel airflow. Affected individuals often complain of apparent nasal obstruction, even though the nasal passages may be widely patent. This condition is known as empty nose syndrome or atrophic rhinitis. Empty nose syndrome can significantly reduce a patient's quality of life and is sometimes treated with turbinate implantation to increase their bulk and resistance and the sensation of airflow within the nose.[22][23] Thus, surgical reduction of the middle and inferior turbinates should be undertaken carefully, although the operation is often performed to alleviate nasal obstruction caused by inferior turbinate hypertrophy and middle turbinate concha bullosa.
Significant turbinate damage should generally be avoided when possible. However, some patients may require frank removal of the turbinates for oncological or reconstructive purposes. Common indications for turbinate resection are the development of Schneiderian papillomas, specifically inverted ones, which often arise in the middle turbinates and require resection to prevent recurrence or malignant degeneration into squamous cell carcinoma. Partial or total maxillectomy may be necessary for other sinonasal or orofacial malignancies. These procedures also often involve resection of one or more turbinates.
The turbinates themselves may be used as part of a reconstructive effort. The inferior turbinates are commonly used as regional flaps, based on the blood supply at the anterior face of the turbinate arising from the anterior lateral nasal and anterior ethmoidal arteries. The flaps effectively provide mucosal resurfacing during total or subtotal nasal reconstruction or repair of large septal perforations.[24]
Clinical Significance
The nasal turbinates play important roles in respiration, immune surveillance, and olfaction. Most patients are unaware the turbinates exist when they function properly. However, dysfunction of the turbinates, particularly the inferior ones, can significantly impair quality of life. Hypertrophied turbinates produce anatomical nasal obstruction. If these turbinates are resected or their mucosa is severely injured, the sensation of nasal obstruction in the absence of a physical blockage can occur. Olfactory epithelial dysfunction leads to a loss of smell and reduced taste sensation, which can significantly impact patient well-being.[25][26][27]
The nasal turbinates' rich vascular supply makes them a common site for nosebleeds (epistaxis), particularly the Kiesselbach plexus (Little area) located on the anterior part of the nasal septum, where several arteries anastomose.
Numerous medical and surgical therapies are available to help manage turbinate dysfunction, often administered by primary care providers, allergists, and otolaryngologists. An interprofessional team strategy will ensure patients receive appropriate evaluation and individualized treatment.