Introduction
The vertebral column, or spine, is composed of 33 vertebrae. These vertebrae play an essential role in protecting the spinal cord and the spinal nerves. They serve as a support for the head, neck, thorax, abdomen, and pelvis while also allowing for flexibility and mobility through the presence of intervertebral discs and facet joints without compromising their supportive function.
The spine consists of multiple segments. These are the following:
- Cervical spine - 7 vertebrae
- Thoracic spine - 12 vertebrae
- Lumbar spine - 5 vertebrae
- Sacral spine - 5 fused vertebrae
- Coccyx - 3 to 5 fused vertebrae
A typical vertebra consists of a vertebral body and vertebral arch. These structures enclose the vertebral foramen, which contains the spinal cord. Seven processes arise from each vertebra. These include two superior articular processes, two inferior articular processes, two transverse processes, and a spinous process. These processes serve as joint facets with adjacent vertebrae, attachment origins for muscles, and form intervertebral foramina from which spinal nerves arise.
Structure and Function
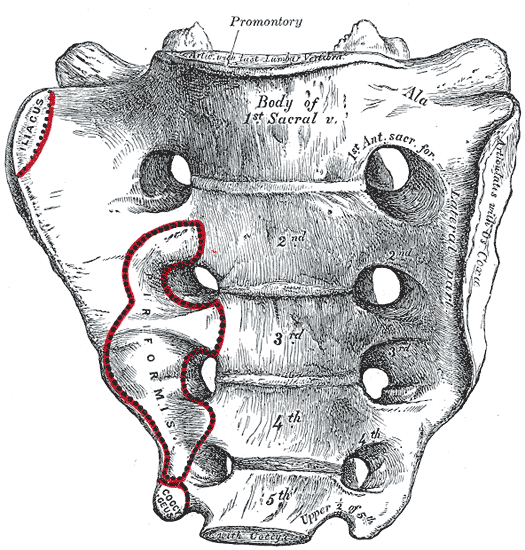
The sacrum is comprised of five fused vertebrae configured as an inverted triangular bone that is concave anteriorly and convex posteriorly. Within the sacrum lies the sacral canal, which is a continuation of the vertebral canal; it terminates as the sacral hiatus. The spinal cord ends in the lumbar region (L1-L2), but the dura mater extends to S2.[1]
Also contained within the canal is the filum terminale, a ligament that extends from the conus medullaris and attaches to the base of the coccyx, thus serving as an anchor for the spinal cord. Four bilateral sacral foramina can be appreciated both anteriorly and posteriorly, which give rise to the S1-S4 spinal nerves.
The superior aspect of the sacrum, referred to as the sacral promontory, articulates superiorly with the L5 vertebral body of the lumbar spine. This arrangement forms the lumbosacral joint, which is reinforced by iliolumbar and lumbosacral ligaments.
The alae (wings) of the sacrum articulate bilaterally with the ilia. These articulations are known as sacroiliac joints. They form an essential connection between the axial skeleton and the appendicular skeleton and function to transfer force from the lower limbs to the vertebral column. The anterior sacroiliac ligament, the posterior sacroiliac ligament, and the interosseous sacroiliac ligament all provide joint stabilization.[2]
The inferior aspect of the sacrum articulates with the coccyx via the sacral and coccygeal cornua.
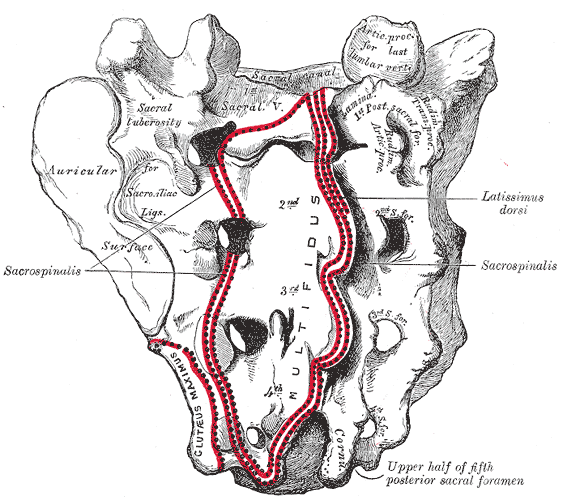
The posterior aspect of the sacrum exhibits numerous bony landmarks. The median sacral crest forms from the fusion of the first three sacral spinous processes and serves as the attachment point for the supraspinous ligament. The intermediate sacral crests form by the fusion of the articular processes. These serve as attachment sites for the posterior sacroiliac ligaments. The lateral sacral crests form by the fusion of the transverse processes. These are the attachment sites for the sacroiliac and sacrotuberous ligaments.
The anterior aspect of the sacrum is less coarse than the posterior aspect. Once the fusion of the sacral vertebrae is complete, four transverse ridges can be appreciated. These ridges represent the remnants of the fused intervertebral discs. The sacral promontory projects anteriorly, forming the posterior ridge of the pelvic inlet. The margins of the ala form the remainder of the pelvic inlet, the arcuate line of the ilium, the pubic pecten, and the pubic crest.
The fusion of the vertebrae and the large size of the sacrum form an ideal base that allows it to support the weight of the entire body.
Embryology
The development of the human skeleton initiates soon after conception. Around days 17 to 19, the notochordal process begins to form. The floor of this notochordal process fuses with the roof of the yolk sac to create the notochordal plate. The plate folds inward, thus forming the notochord. The notochord plays a vital role in maintaining the structure of the embryo and provides stimulation for the differentiation of surrounding tissue. The notochord stimulates the overlying ectoderm to form neuroectoderm, giving rise to the neural plate, eventually forming the neural tube. The neural tube provides the framework for the adult brain and spinal cord. The notochord itself will ultimately persist to form the nucleus pulposus in adults.[3]
Beginning in the third week of gestation, somites start to develop around the notochord in a cranial to caudal direction. These somites give rise to sclerotomes. Two adjacent sclerotomes will fuse to form each vertebral body in a process called segmentation.
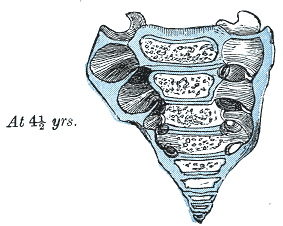
Endochondral ossification begins around the sixth week of gestation. Three primary ossification centers start to form in each vertebra. One center forms in the endochondral centrum and will lead to the ossification of the vertebral body, while the other two centers form in the neural processes and will lead to the ossification of each pedicle. This process begins in the thoracolumbar region and proceeds bi-directionally (both cranially and caudally). The primary cartilage is replaced by bone during the eighth week of gestation: the neural processes and the centrum fuse around 3 to 6 years of age. Endochondral ossification is not completed until around the age of 26.[4]
Sacral fusion begins around puberty and is completed by age 25 to 30.[5]
Blood Supply and Lymphatics
The blood supply of the sacrum is provided by the median sacral artery, as well as two lateral sacral arteries. The median sacral artery is a branch of the abdominal aorta that arises just before the bifurcation and proceeds to run along the midline of the sacrum. The lateral sacral arteries arise from the posterior division of the internal iliac artery bilaterally.[6]
Spinal veins drain into venous plexuses that are located both inside and outside the vertebral canal.[7]
Lymph nodes are located in the concavity of the sacrum. They receive lymphatic flow from the rectum and posterior pelvic wall.
Nerves
There are five pairs of sacral spinal nerves (S1-S5). The S1-S4 nerves originate from the cauda equina of the spinal cord, travel down the sacral canal, and exit via the four sacral foramina. S5 follows the same route other than it exits from the sacral hiatus rather than via foramina. The vertebrae themselves receive innervation by the meningeal branches of these spinal nerves.[8]
Muscles
The sacrum serves as the attachment point for numerous muscles. These muscles can group into those that attach to the anterior sacrum and those that attach to the posterior sacrum.[9]
- The anterior surface
- Piriformis - originates from sacral segments 2 through 4
- Coccygeus - inserts on the border of the lower sacrum and coccyx
- Iliacus - some fibers originate from the ala of the sacrum
- The posterior surface
- Gluteus maximus
- Multifidus lumborum
- Erector spinae
Physiologic Variants
The most notable physiological variant of the sacrum is represented by its sexual dimorphism. The sacrum tends to be shorter and broader in females than in their male counterparts. Females also have a less prominent sacral promontory, which allows for easier passage of offspring during childbirth.
Another common variant is the presence of lumbosacral transitional vertebrae (LSTV). An LSTV may arise when either the L5 vertebra undergoes sacralization and fuses to the sacrum (resulting in 6 sacral vertebrae) or when the S1 vertebrae undergo lumbarization to become a 6th lumbar vertebrae (resulting in 4 sacral vertebrae). A meta-analysis from 1986 to 2007 revealed the prevalence of LSTV might be as high as 12.3%.[10]
Many more anatomical differences exist, such as a variation in the number of sacral foramina, as well as morphological defects, such as sacral agenesis, sacral spina bifida, and the presence of a sacral rib.
Surgical Considerations
Knowledge of these anatomical variations is essential in avoiding complications that may arise in orthopedic spine surgery, anesthesia, obstetrics, and forensics. Examples of cases that merit special consideration include:
- S1 transpedicular screw fixation
- Iliosacral screw fixation
- Caudal epidural block
- Obstetric-conjugate measurements in childbirth
Clinical Significance
The venous plexuses surrounding the vertebral column allow for cancer metastasis from the pelvis. The sacrum can also be the site for primary sarcomas. Sacral tumors can result in lumbosacral plexopathy.[11]
Sacral Stress Fractures
There are three patient populations prone to experiencing a fracture of the ala of the sacrum: (1) older patients; (2) postnatal subjects; and (3) athletes. In one study of 920 athletes, thirteen had fractures of the ala of the sacrum.[12][13][14]
Sacral Insufficiency (Fragility) Fractures
Sacral fractures have two basic types. Sacral insufficiency results when diminished or diseased sacral bone is stressed, most often in the presence of osteoporosis. Sacral insufficiency (fragility) stress fractures occur with a median of 71 years of age.[14]
Fragility fractures of the sacrum result from a normal force acting on a deficient or diseased bone.[15] Sacral insufficiency fractures have the following risk factors: osteoporosis (especially in older patients and undernourished females), pelvic radiation therapy, and rheumatoid arthritis. Regarding the physical examination, sacral insufficiency fractures have a hallmark symptom of pain being generated with pressure over the dorsum of the sacrum. In sacral insufficiency fractures, patients recall little or no trauma before the onset of symptoms. Sacral stress factors produce obscure or insidious pain in the lower back, buttock, or pelvis.[14]
Sacral fragility fractures may cause cutting of the distal sacral nerve roots. Electrophysiological analysis may help analyze the neural damage that can occur with sacral fractures.[16]
Sacral Fatigue Fractures
Sacral fatigue fractures occur when a normal sacral bone is stressed and fractures. This variety is most commonly seen in athletes and military recruits undergoing intense activity and training. Sacral fatigue fracture risk factors include deficiencies in diet and intensity of exercise.[14]
Traumatic Sacral Stress Fractures
Traumatic sacral stress fractures can embody elements of both types, as young athletes and older patients can both undergo trauma, such as an automobile accident. Traumatic sacral stress fractures involve high-energy sacral trauma, often involving lesions of the lumbosacral plexus.[17] The specific classification methods for sacral fractures, such as the Denis I, Denis II, and Isler classifications, have been studied.[17] Traumatic sacral fractures account for 20% to 30% of pelvic fractures.
Surgical options for traumatic sacral fracture include trans-sacral bar osteosynthesis, minimally invasive sacroiliac screws, open reduction with internal fixation, and spinopelvic stabilization.[18] Risk factors pertinent to sacral stress fractures have been described.[18]
Screening for sacral fractures with radiographs of the lumbar and sacral area often fails to detect the lesion. Laboratory studies can detect the presence of osteoporosis, which is the primary risk factor for sacral insufficiency fractures.
Sacral stress fractures are commonly misdiagnosed as a herniated intervertebral disc, herniated nucleus pulposus disease, sacroiliac disease, facet arthropathy, compression fractures, trochanteric bursitis, strains involving the hamstrings and muscles of the lower back, and spondylolisthesis.
Cervical Cancer Radiation and Sacral Stress Fractures
Cervical cancer can be treated by radiation therapy.[12] Although this is an effective treatment for cervical cancer, radiation therapy can result in a fracture of the sacrum. The incidence of cervical post-radiational fracture is 20% to 40%. Of these, 75% involve the sacrum. Detection of fracture lines is a crucial aspect of diagnosis, but these are not always present. Bone scintigraphy may be useful for detecting sacral fractures. CT can be specific for fracture lines. MRI has greater selectivity. Coronal fat saturation T2W is recommended for imaging of the sacrum, including sacral lines.[12]