Introduction
The distal radioulnar joint (DRUJ) is responsible for the integrity of the articulation between the distal radius and distal ulna; this is important in both the supination and pronation of the forearm and anteroposterior translational stability. The distal radioulnar joint is a critical stabilizing structure of the ring, stabilizing the radius and ulna, and pathologies afflicting the distal radioulnar joint can impact the hand, wrist, and elbow.
Clinically, the distal radioulnar joint carries critical importance as it can undergo an acute injury or chronic degeneration due to long-term sequelae from previous injuries. This spectrum of pathology leads to significant wrist pain, dysfunction, degeneration, and subtle to gross instability. The goal of this activity is to provide an anatomic review and the basics of clinical importance for the education of current and future healthcare providers.
Structure and Function
The primary role of the distal radioulnar joint is to stabilize the articulation of the radius around the stationary ulna during pronation and supination.
Osteology
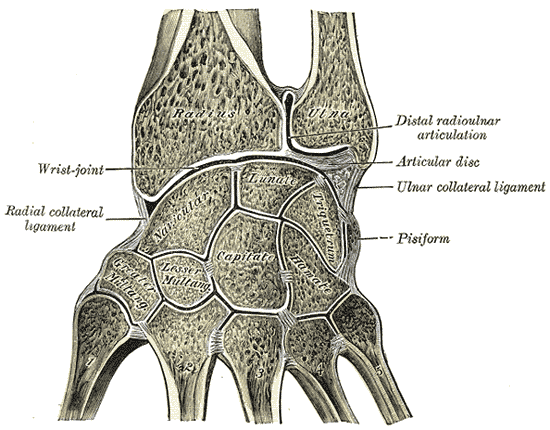
The distal ulna has a styloid process and an ulnar head. There is a fovea or depression between them. The ulnar head is located within the sigmoid notch of the radius. The styloid process is a site for the attachment of the radioulnar ligaments.[1] The shape of the distal end of the ulna is determined by the fovea, the sulcus of the tendon of the extensor carpi ulnaris, the styloid process, and the shape of the joint cartilage.
An anatomic study of this osseous anatomy revealed that the length of the sigmoid notch increases from volar to dorsal. There is additionally significant variation of the ulnar length, which was found to have a negative correlation to the mid-coronal length of the sigmoid notch.
Obliquity of the distal radioulnar joint was also found to correlate with the ulnar variance. In patients with a typical negative ulnar variance, the sigmoid notch was found to be angled in a proximal-ulnar direction, but as ulnar variance became more positive, this became progressively less angled, eventually resulting in a reverse obliquity. There was considerable variability between the specimens analyzed but bilateral consistency in a given specimen. This variability indicates that comparison may be made within a particular patient but should be made cautiously when comparing anatomy between patients.[2]
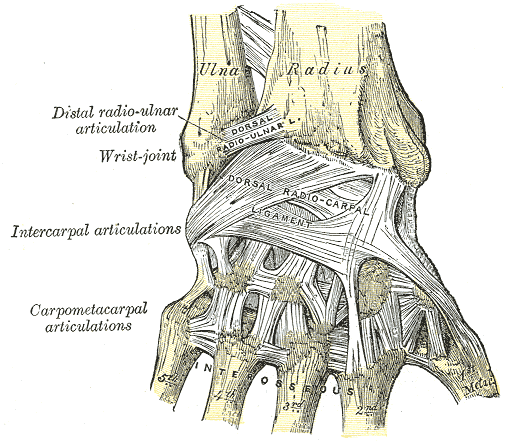
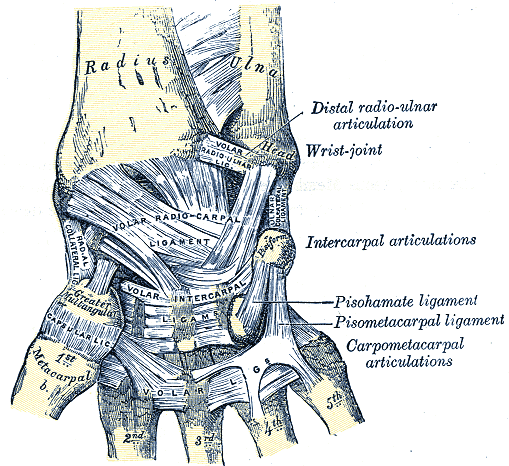
Ligaments
The radioulnar ligaments are the major stabilizers of the distal radioulnar joint (DRUJ). These are proximal condensations of the triangular fibrocartilage complex TFCC.[2]
The ulna has prominence on the dorsolateral aspect of the styloid process. This is the site of attachment of the radioulnar ligaments. The radioulnar ligaments connect the styloid process of the distal ulna to the articular surface of the fovea.[1][3] The volar and dorsal radioulnar ligaments unite the radius and ulna, which form the radioulnar joint. The radioulnar ligaments, which connect the articular disc and distal ulna, are important in stabilizing the DRUJ under dynamic loading.[4] The articular disc separates the distal radioulnar joint from the wrist joint cavity.
The structures involved in strengthening and stabilizing the distal radioulnar joint (DRUJ) are formed from volar and dorsal radioulnar ligaments (RULs) and the triangular fibrocartilagenous complex (TFCC).
The radioulnar ligaments are the major stabilizers of the distal radioulnar joint. These are proximal condensations of the triangular fibrocartilage complex. The current school of thought states that during pronation, the dorsal radioulnar ligament becomes tight while the palmar radioulnar ligament becomes lax; during supination, the reverse occurs. Though some debate surrounds the role of ligamentous stability in the distal radioulnar joint, a growing body of evidence supports this model.[5]
Several studies have also looked into the role of the radioulnar ligaments in the translational stability of the distal radioulnar joint. These studies have agreed that the dorsal radioulnar ligament is particularly important to dorsal translational stability when the forearm is in pronation. The palmar radioulnar ligament correlates with the stability of volar translational stability with the forearm in supination. Additionally, radioulnar ligament disruption was found to increase the rotational range of motion in the biomechanical study performed by Ward et al. This novel report indicates the importance of the ligamentous complexes to the rotational stability of the distal radioulnar joint.[6]
Triangular Fibrocartilage Complex (TFCC)
The most common cause of DRUJ instability involves lesions of the triangular fibrocartilage complex (TFCC) because it plays a critical role in stabilizing the distal radioulnar joint.[7] The triangular fibrocartilage complex is composed of the following components: articular disc, proximal and distal laminae, volar (anterior) radioulnar ligament, dorsal radioulnar ligament, ulnar collateral ligament, ulnolunate ligament, ulnotriquetral ligament, ulnocollateral ligament, and the insertion of the tendon of the extensor carpi ulnaris on the fovea.[8][3]
The fovea is part of the triangular ligament. It is the site of a radioulnar ligament on the distal ulna.[1] The foveal attachment contributes most significantly to the ligamentous stability of the distal radioulnar joint.[9] Disruption of the triangular fibrocartilage complex can produce ulnar variance when the wrist is under load.[9]
Interosseous Membrane
The interosseous membrane stabilizes the radioulnar joint, especially in supination.[10] The triangular fibrocartilage complex and the interosseous membrane connect the ulna and radius. The components of the interosseous membrane of the forearm are the central bundle, proximal bundle, and distal bundle of the forearm. The interosseus membrane is involved in longitudinal stability.
In cases of fracture of the proximal radial head, both the central band of the interosseous membrane and the triangular fibrocartilage complex are important in giving axial stability to the radius.[10] Instability resulting from fracture of the distal radioulnar joint can take many directions: anterior, posterior, and intermediate directional instability.[3]
Joint Capsule
The radioulnar joint cavity is shaped like an “L.” The radioulnar joint capsule is formed by a fibrous band enclosing the distal radioulnar joint. It has a sack-shaped recess to accommodate twisting of the capsule with pronation.
The role of the interosseous membrane, joint capsule, and articular disc in maintaining joint stability have been less well studied but are part of the sectioning sequences used in biomechanical studies and have not consistently correlated with gross instability of the joint.
Embryology
While a great deal of embryologic investigation has occurred relative to the triangular fibrocartilagenous complex, studies targeting other ligamentous structures of the wrist are lacking. Reports show that the ligamentous structures begin to appear in O’Rahilly stage 23 embryos and are complete by week 14 of gestation.
The interzone is a portion of the condensed mesenchymal structure whose appearance signals the beginning of wrist joint formation. The interzone forms three layers, of which the intermediate layer is thought to be most important to the formation of the ligamentous structures of the wrist.[11]
Blood Supply and Lymphatics
Arterial supply to the distal radioulnar joint derives primarily from the palmar and dorsal branches of the anterior interosseous artery. These arteries branch at the proximal border of the pronator quadratus and form an anastomotic complex. Other contributions are made by anastomoses as follows: dorsal interosseous artery to the dorsal branch of the anterior interosseous artery, ulnar artery to the palmar branch of the anterior interosseous artery, and collateral circulation from dorsal and palmar carpal arches.[12][13][14]
The lymphatic pathways of the upper extremity have been poorly described, but various courses have been noted, including perforators accessing the wrist compartment. These drain from distal to proximal and have little consistency in their flow from deep to superficial or superficial to deep. Primary lymph node collections in the upper extremity appear in the cubital and axillary regions.[15]
Nerves
Innervation to the distal radioulnar joint derives from distal continuations of the median nerve via the anterior interosseous nerve and the radial nerve via the posterior interosseous nerve.[16][17][18] These form articular branches that supply the region distal to the proximal border of the pronator quadratus.[19]
Muscles
The flexors and extensors of the wrist, hand, and fingers provide additional soft tissue support and stabilization to the distal radioulnar joint. Of particular note is the pronator quadratus. Biomechanical analysis has shown that the pronator quadratus has a role in tensioning the distal radioulnar joint. Both the deep and superficial heads of the pronator quadratus originate from the dorsoulnar aspect of the ulna and attach to the palmar aspect of the radius. This orientation allows for tensioning of the distal radioulnar joint during pronation, preventing interposition of the capsule and joint diastasis.[4]
Physiologic Variants
A significant physiologic variance exists with ulnar length relative to the radius, as discussed above in the Structure and Function Section; this also results in a considerable variation of the sigmoid notch. This variance has potential significance, and it should be considered when assessing a patient with a forearm fracture or wrist pain.[2]
Surgical Considerations
Tears of the TFCC can be treated arthroscopically or by open surgical repair. If necessary, tears of the FFCC can be repaired using the tendon of the palmaris longus.[7] Surgery is indicated for patients with isolated or associated injuries yielding significant distal radioulnar joint instability.
Surgical repair of the distal radioulnar joint is contraindicated for patients with other evident pathology, including radial and ulnar length discrepancies, distal radioulnar joint arthritis, sigmoid notch incompetence, extensor carpi ulnaris tendon subluxation, or other apparent reason for wrist pain. Reconstruction of the triangular fibrocartilage complex and distal radioulnar joint often does not restore stability to the joint, and careful patient selection should be carried out with the understanding that these procedures are performed primarily as adjunctive procedures to control pain.
Various surgical reconstruction procedures exist in the literature, including reconstruction of the radioulnar ligaments, placement of an extrinsic radioulnar tether, and creation of a radiocarpal sling or tenodesis. These procedures have inherent limitations but have been found to help control symptoms.[20]
Arthroscopy of the wrist is part of the diagnostic process for pain on the ulnar side of the wrist.[3]
Distal radial fractures are a source of DRUJ instability as well as causing tears in the TFCC. These can be treated with an intramedullary nail.[21] Acute distal radioulnar joint dislocations occur with a fracture of the distal radius or radial head.[3] Other conditions accompanying such fractures are ulnocarpal abutment, extensor carpi ulnaris tendonitis, and ulnotriquetral ligament tears.[3] Malunion of fractures of the distal radius can cause instability of the distal radioulnar joint. Such fractures can be repaired using a fixed-angle volar locking plate.[22]
A fracture of the ulnar styloid process can complicate distal radioulnar fractures. In the treatment of a distal radial fracture, K-wire was used in the repair of the fracture. Under such circumstances, repairing the ulnar styloid fracture was unnecessary.[8]
Clinical Significance
Distal radioulnar joint instability may result from traumatic injury or chronic degeneration. These carry varying significance and treatment options, as discussed in the surgical considerations section of this article. Chronic tears should be suspected in older patients, while acute tears occur in the setting of upper extremity trauma. Injuries to the distal radius and ulnar styloid fractures are often implicated in these traumatic injuries to the distal radioulnar joint. The clinical importance of these injuries is a matter of debate, and functional outcomes more than likely correlate with appropriate treatment of radial fractures than treatment of ligamentous or ulnar styloid fractures. Evaluating distal radioulnar joint instability should include a thorough history and physical exam, including proper tests.[23]
Subluxation-related ulnar neuropathy (SUN) syndrome is a potential complication of chronic instability of the distal radioulnar joint. Compression and kinking of the ulnar nerve can occur within the Guyon canal leading to numbness and tingling of the fourth and fifth digits with potential weakness of the intrinsic muscles of the hand in more advanced cases. Evaluation of symptoms of ulnar neuropathy should include stressing the distal radioulnar joint to verify the condition's etiology.[24]
DRUJ TFCC Diagnosis
Instability of the distal radioulnar joint and tears of the triangular fibrocartilage complex can often be diagnosed clinically. CT and MRI can be performed in supination and pronation to help diagnose these conditions.[3] If the distance between the radius and ulna is more than 6 mm on CT examination, instability should be suspected. Radiographs are useful for other lesions that may occur, including pseudoarthrosis of the ulnar styloid, osteoarthritis, malunion of the distal radius, ulnocarpal impaction, and ulnocarpal abutment.[3]
Ulnar pain is usually seen with DRUJ instability. A "clunk" is seen in more severe cases due to a positional dislocation/relocation of the head of the ulna.[25] Pain is usually felt with pronation and supination against resistance, which can indicate TFCC damage.[3]
Diagnostic Tests for Distal Radioulnar Joint Instability and TFCC Tears
Diagnostic tests for distal radioulnar joint instability and TFCC tears:
Piano Key Sign – The examiner has the patient place the head of the ulna in a dorsal position (as in beginning to play the piano). The forearm is pronated. The examiner places a volar force on the head of the ulna. Increased translation compared to the other side is considered a positive test.[23]
Press Test – The patient begins sitting in a chair with arms, then arises from the chair by pressing his hands on the arms of the chair. Ulnar pain is present when the TFCC is torn.
Grind Test – The patient's distal forearm is held steady by the examiner. The other hand holds the wrist. The wrist is then supinated in ulnar deviation. Grinding the wrist over the forearm compresses the carpus against the TFCC.
Fovea Sign – The examiner compresses the interval between the styloid process and the tendon of the extensor carpi ulnaris. Tenderness here indicates a lesion of the DRUJ when the pain is greater than on the opposite side.
DRUJ (Ballotment) Test – One of the examiner's hands stabilizes the radiocarpal joint while the ulna is "shucked" by the other hand. The test is performed in supination and then in pronation.
DRUJ TFCC Repairs and Treatment
Instability of the distal radioulnar joint can result in weakness, pain, and degenerative arthritis.
Failure to treat an injury is a common cause of distal radioulnar joint instability. Tears limited to the distal radioulnar joint produced by falling onto an outstretched hand can be incorrectly treated as simple wrist sprains. Inflammatory arthritis can lead to instability of the distal radioulnar joint.
Disruption of the triangular fibrocartilage ligament can result in ulnocarpal abutment, which can be very painful. The pain is located on the ulnar head of the ulnar carpus.[9]
Further information is located in the section on Surgical Considerations.