Introduction
The heart muscle is the myocardium or middle layer of the heart walls. The myocardium is responsible for the contractile function of the cardiac pump. Composed of cardiomyocytes, the heart muscle has distinctive cellular and physiological features, allowing it to generate force to maintain adequate tissue and organ perfusion throughout the body. The heart muscle is one of the earliest functioning embryonic organs, and it continues to contract and beat throughout a person's lifetime. Supplied by a complex system of coronary vasculature, cardiac lymphatics, and autonomic innervation, cardiomyocytes form the thickest layer of every heart chamber.
Cardiovascular diseases are the leading cause of mortality worldwide. A vast number of these diseases involve the heart muscle with diverse pathophysiological mechanisms, leading to contractile dysfunction, cell damage and death, and cardiac pump failure. However, numerous interventions, treatment options, and therapies are aimed at minimizing damage, restoring functionality, preventing the occurrence, and reducing the risk of cardiovascular disease. Understanding heart muscle anatomy and function is crucial in managing various cardiovascular conditions.
Structure and Function
Three distinct layers comprise the heart walls, from inner to outer:
- Endocardium
- Myocardium
- Epicardium
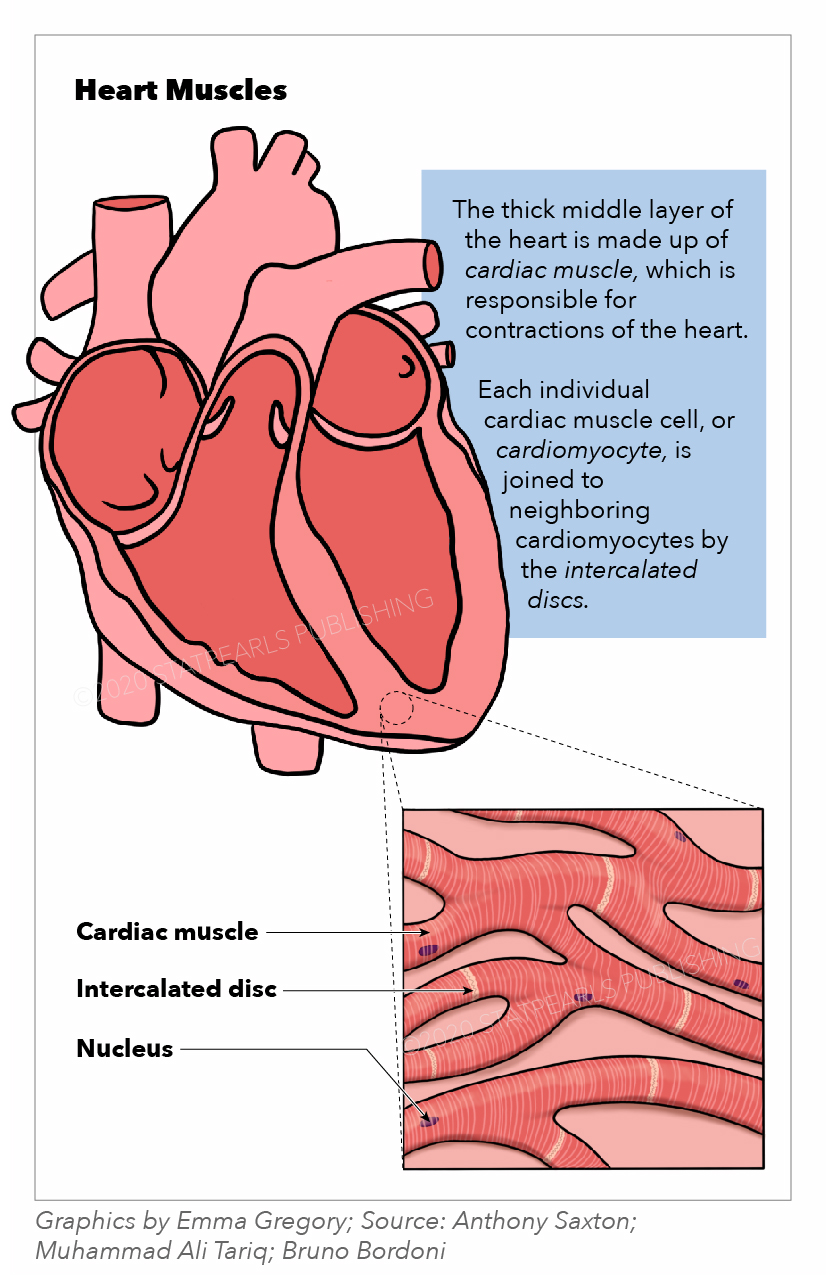
The heart muscle, or myocardium, comprises the middle and thickest layer of the heart wall (see Image. Heart Muscles). The myocardium lies between the endocardium, which lines the inner chambers, and the epicardium, the inner pericardial layer that surrounds and protects the heart. Histologically, the heart muscle is composed of cells called "cardiomyocytes," with unique structures and properties correlating to their contractile function.
Cardiomyocytes are striated, uninucleated muscle cells found exclusively in the heart. Cardiomyocytes facilitate cell-to-cell communication through intercalated discs, which contain gap junctions and other cell adhesions. These discs reduce internal resistance, allowing action potentials to spread quickly throughout the heart muscle via electrically charged particles called ions. Thus, the heart muscle acts as a functional syncytium with rapid synchronized contractions responsible for pumping blood. Functionally, the heart muscles rely on electrochemical gradients and the potential to generate contractile force for each heartbeat.
The sinus, or sinoatrial, node within the right atrial myocardium spontaneously depolarizes and thus determines the heart rate. These depolarizations are ion influx currents traveling from the sinus node to the heart muscle via conducting cells. Heart muscle depolarization opens voltage-gated sodium channels, allowing a rapid influx of sodium ions into the cardiomyocytes and depolarizing the cells. The positive membrane potential opens voltage-gated potassium and calcium channels, allowing potassium and calcium to rush out.
The initial calcium influx is necessary for the second calcium release from the sarcoplasmic reticulum within the heart muscle cells. The accumulation of intracellular calcium ions binds to troponin C, moving tropomyosin aside to allow actin-myosin binding and cross-bridge cycling responsible for muscle contraction. The amount of calcium released is directly proportional to the amount of actin-myosin interaction allowed and thus correlates with the contractile force of the heart muscle generated. Physiologically, this corresponds with parameters such as stroke volume, ejection fraction, and cardiac output used to assess heart function.
At the end of each cycle, calcium returns to the sarcoplasmic reticulum via the sarco(endo)plasmic reticulum (SER) Ca2+ ATPase (SERCA) pumps. In contrast, sodium-potassium and sodium-calcium ATPase pumps restore the cardiomyocyte membrane potential so the cycle can repeat with the subsequent incoming depolarization.[1]
Embryology
The heart muscle originates from the mesoderm layer and begins forming during the 3rd week of embryonic development. The mesoderm is the primary source of myocardial precursor cells, which comprise the cardiogenic or primary heart field during early development. A primitive, horseshoe-shaped endothelial heart tube is formed and begins contracting to facilitate the early circulatory system.
Within the next several weeks, the proliferation of cardiomyocytes expands the myocardial layer and generates the multichambered system of the mature heart. While existing cardiomyocytes contribute to the growth of the myocardium via proliferation and organization, new heart muscle cells are also recruited from adjacent mesenchymal layers that further expand the muscle layer.[2]
The heart walls undergo further maturation, compaction, and trabeculation following myocardial development. Dilatations or swellings of the heart tube embryonic structures, along with neural crest cell migration, facilitate the development of the chambers and inflow and outflow tracts. These processes result in a mature, fully functional, contracting heart by the 8th embryonic week and throughout adulthood.
Blood Supply and Lymphatics
The heart muscles’ blood supply comes directly from the coronary arteries within the epicardial layer. Two main coronary arteries, the left (LCA) and right coronary arteries (RCA), branch directly off the aorta via the coronary ostia. These arteries and their branches supply vessels that run perpendicular to the heart surface and transverse from the epicardium, through the myocardium, and down to the endocardium.
The LCA quickly branches into the left anterior descending (LAD) and left circumflex (LCX) coronary arteries. The LAD runs vertically down the interventricular groove toward the apex. This vessel supplies blood to the anterior left ventricular myocardium, anterior two-thirds of the interventricular septal myocardium, and anterolateral papillary muscle connecting the mitral valves. The LCX courses horizontally along the atrioventricular groove and gives rise to the left obtuse marginal coronary artery, supplying the lateral and posterior left ventricular myocardium.
The RCA runs horizontally along the right atrioventricular groove, giving rise to the right acute marginal coronary artery, which supplies the right ventricular myocardium. The RCA also gives rise to the posterior descending artery (PDA) in about 90% of the human population. The PDA comes from the LCX in the other 10%. The PDA supplies the posterior myocardium of both ventricles, the posterior third of the interventricular septal myocardium, and the posteromedial papillary muscle of the mitral valves.
Blood flow via the coronary arteries to the myocardium occurs during diastole and ventricular relaxation via the passive blood flow into the aortic ostia. Systolic ventricular contraction compresses the coronary arteries, impeding myocardial blood flow.
The heart muscles' venous system runs parallel to the coronary arteries. Venous drainage of the left ventricular myocardium is completed by the interventricular and great cardiac veins, which empty into the coronary sinus. The latter vessel is found in the posterior right atrioventricular groove and empties into the right atrium. The anterior cardiac veins direct blood from the right ventricular myocardium directly into the right atrium.[3]
The cardiac drainage system comprises lymphatic capillaries and precollector vessels organized in plexuses within each heart wall layer.[4] These lymphatic vessels and plexuses flow from the subendocardium, through the myocardium, up through the subepicardium, into the mediastinal lymph nodes, and ultimately drain into both left and right venous angles between the internal jugular and the subclavian veins. The flow source for lymphatic drainage comes from myocardial contractions, which generate the force required to propel fluid through the system toward the lymph nodes.
Nerves
Heart muscles are innervated primarily by the accelerans and vagus nerves, which provide sympathetic and parasympathetic stimulation, respectively. Intrinsic myocardial ganglia are present in the epicardium, which receives postganglionic sympathetic signals from the accelerans nerve and preganglionic parasympathetic impulses from the vagus nerve.
Most postganglionic sympathetic connections synapse directly with the heart muscle cells, releasing norepinephrine as the primary neurotransmitter. Upon binding, norepinephrine stimulates β-adrenergic receptors to increase myocardial contractility by increasing calcium influx. Preganglionic parasympathetic fibers synapse with the epicardial intrinsic ganglia, and then postganglionic neurons directly synapse with the myocardium.[5] Acetylcholine is the primary neurotransmitter for myocardial parasympathetic signals, acting on muscarinic (M2) receptors in the cardiomyocytes.
Muscles
Myocardium is found in the walls of all 4 heart chambers, though it is thicker in the ventricles and thinner in the atria. This disparity is due to the differences in the generated force of contraction needed for propelling blood between the atria and the ventricles, with the ventricles requiring much more power.
Physiologic Variants
Chronic primary hypertension is a prevalent disease affecting a large percentage of the population. Chronic systemic hypertension can result in structural and functional changes to the heart muscle. Chronically high afterloads from higher mean arterial pressures cause the left ventricular muscle to contract against greater pressures, leading to compensatory cardiomyocyte hypertrophy. The ventricular muscle wall thickens to reduce wall stress, increasing the ratio between wall thickness and chamber diameter. Left ventricular hypertrophy thus characteristically demonstrates concentric thickness and is a physiological response to, and a common complication of, chronic hypertension.[6] Physical examination findings of left ventricular hypertrophy may include a diffuse point of maximal impulse and an S4 gallop upon cardiac apex auscultation.
Typical aging processes alter heart muscle structurally and physiologically. Arteries stiffen and become less compliant over time, increasing afterload and requiring the heart muscle to contract against higher pressure, especially in older age. Left ventricular thickness increases from cardiomyocyte hypertrophy as a compensatory response. Cardiomyocytes eventually diminish due to apoptosis, necrosis, or autophagy, leading to an overall decrease in cardiomyocyte numbers in aged heart muscle. The remaining cardiomyocytes may hypertrophy or undergo pathological remodeling as a compensatory mechanism. These changes result in decreased cardiac compliance and increased wall stiffness.
Age-related changes within the heart muscle cells induce a shift from the α-myosin heavy chain to the β-myosin heavy chain with reduced cross-bridge cycling activity. This condition ultimately leads to contractile decline and diastolic dysfunction in the aging heart muscle. Calcium homeostasis is also affected by aging due to the reduced ability of SERCA and sodium-calcium pumps to restore resting membrane potential calcium levels effectively.[7] Disrupted calcium homeostasis affects heart muscle relaxation mechanics and thus leads to diastolic dysfunction.
Surgical Considerations
A significant yet underrecognized heart muscle complication after noncardiac surgery is perioperative myocardial injury, which is distinct from myocardial infarction. Risk factors for perioperative myocardial injury include age of at least 65 years and a preexisting history of atherosclerotic disease. An acute increase in high-sensitivity cardiac troponin T (hs-cTn) plasma concentrations during the perioperative period suggests the condition.[8]
Perioperative myocardial injury often presents without chest pain, dyspnea, or other typical cardiac injury symptoms and is, therefore, often missed during routine perioperative clinical workups. The condition correlates with a significantly increased risk of 30-day mortality post-noncardiac surgery.[8] Diagnosis requires perioperative hs-cTn screening to detect and quantify cardiomyocyte injury, which is necessary for reducing the risk of short and long-term mortality.
Clinical Significance
Coronary artery disease (CAD), also termed "ischemic heart disease," is the most prevalent cardiovascular disease and the leading cause of global mortality, with significant implications and consequences for heart muscle functionality. CAD is characterized by atherosclerotic plaque formation within the coronary arteries, reducing blood flow and oxygen and nutrient delivery to the myocardium. CAD manifestations, termed "acute coronary syndromes" (ACS), include unstable angina and myocardial infarction. These conditions arise from insufficient oxygen perfusion due to at least 70% occlusion of the myocardial blood supply.
The most severe presentations of CAD are myocardial infarctions, colloquially termed “heart attacks.” Myocardial infarctions divide into ST- (STEMI) and non–ST- (NSTEMI) segment elevation myocardial infarctions, depending on total or near-total coronary vascular occlusions, respectively, and subsequent findings on electrocardiogram (ECG). Myocardial infarctions can be generally localized by identifying the ECG leads exhibiting abnormal ST-segment or T-wave morphologies. Myocardial infarctions result in cardiomyocyte necrosis. Diagnostic findings include elevated cTn and creatinine kinase myocardial band (CK-MB) levels.[9]
Following an infarction, the affected heart muscle wall often weakens from cell injury and death, inflammation, and fibrotic replacement, decreasing heart muscle contractility and increasing the risk of heart failure, free wall ruptures, arrhythmias, sudden cardiac death, and other complications. Myocardial infarction treatment includes pharmacotherapy such as antiplatelet drugs and fibrinolysis, minimally invasive procedures such as percutaneous coronary interventions, and major surgeries such as coronary artery bypass grafting aimed at restoring myocardial perfusion and vascularization.[9]
Cardiomyopathies are inherited or acquired heart muscle diseases that affect structure and functionality in the absence of other cardiovascular disease processes, such as CAD. Hypertrophic cardiomyopathy (HCM) is the most common genetically inherited heart disease and follows an autosomal dominant inheritance pattern with variable penetrance. The pathogenesis of HCM is mutations in myocardial sarcomere genes, leading to myofibrillar disarray, severe thickening, heart muscle wall hypertrophy, and diastolic dysfunction. Manifestations of HCM include dyspnea, syncope, palpitations, and sudden death. The condition most commonly presents in adolescence.
Dilated cardiomyopathy (DCM) is characterized by eccentric ventricular hypertrophy, cardiac muscle wall dilation, and systolic dysfunction.[10] DCM is the final myocardial response to a variety of genetic disorders and environmental stresses, such as chronic alcohol misuse, viral and parasitic infections, certain drugs, and other etiologies, with the most common being idiopathic DCM.[11] Treatment for cardiomyopathies includes pharmacotherapy to reduce heart muscle demand, such as calcium-channel blockers and β-blockers, implantable cardioverter-defibrillator placement to prevent life-threatening arrhythmias, and heart transplantation.
Myocarditis is the term for heart muscle inflammation. The condition has several etiologies; the most common etiology in the Western world is viral infections (infectious myocarditis). Other causes include toxic reactions and allergies to drugs, autoimmune diseases, and other infections (bacterial, fungal, parasitic).
Myocarditis involves damage and loss of both cardiomyocytes and cardiac vascular endothelial cells, which are common targets of infection, inflammatory processes, and white blood cell (often lymphocytic) infiltration into the heart muscle wall. Myocarditis has a diverse presentation with nonspecific symptoms, including chest pain, dyspnea, and flu-like manifestations, but can also be asymptomatic. Complications include interstitial cardiac fibrosis, wall motion abnormalities, arrhythmias, heart failure, myocardial infarctions, reduced ejection fraction, and sudden cardiac death.[12]
Heart failure is the common end-stage pathway and clinical manifestation of cardiac pump dysfunction from a variety of etiologies, including many diseases affecting the heart muscle. Heart failure is the inability of the heart to pump adequately, leading to congestion, reduced organ perfusion, and functional impairment. Etiologies and risk factors for this condition are diverse and encompass processes such as myocardial injury or infarction, CAD, chronic hypertension, valvular dysfunction, arrhythmias, and cardiomyopathies. The pathophysiology resulting in heart failure involves complex interactions of systems such as neurohormonal activation, peripheral vascular effects, and physiological processes within the heart muscle itself. Heart failure treatment includes medications like angiotensin-converting enzyme inhibitors and β-blockers to reduce heart stress and workload. Inotropes may also be used to boost contractility. Advanced heart failure therapies involve mechanical circulatory support, such as ventricular assist devices and heart transplantation.