Introduction
The uterine arteries are the main blood vessels that supply blood to the uterus. They give off branches that supply different portions of the uterus and plays an important role in maintaining blood supply during physiological processes, such as the altering endometrium during the menstrual cycle and growth of the uterus during pregnancy. During its course, the uterine artery passes anterior to the distal ureter; some refer to this as “water under the bridge.”
Structure and Function
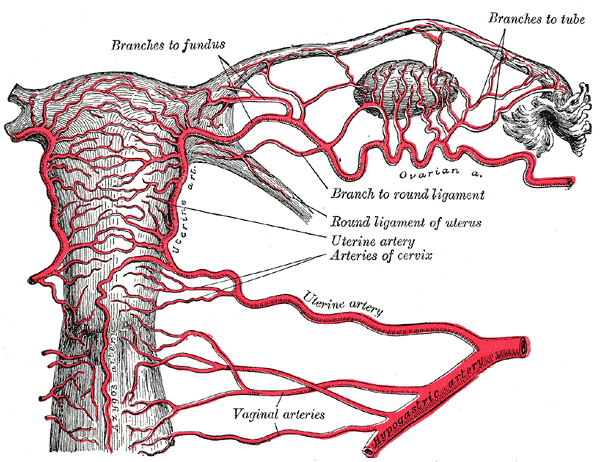
There are two uterine arteries, one on each side (left and right). The uterine artery is a branch of the internal iliac artery also called hypogastric artery. The right uterine artery is a branch of the right anterior division of the internal iliac artery. The uterine artery courses from lateral to the medial direction through the bottom part of the broad ligament also called the cardinal ligament. At the uterine isthmus level, the uterine artery is divided into ascending and descending branches.[1][2][3]
After the bifurcation, the ascending artery further rises superiorly next to the uterus and runs a tortuous course with the lateral side of the uterus. The ascending artery, in multiparous women, become much more convoluted and tortuous in size and shape. The ascending branch of the uterine artery anastomoses to the ovarian artery. The ovarian artery is a direct branch of the abdominal aorta. The ovarian artery supplies oxygenated blood to the ovary, fallopian tube, and uterus. In the myometrium, the uterine artery further branches out to the arcuate artery, radial artery, spiral artery, and basal artery.
The descending branch supplies blood to uterine cervix and vagina. The arcuate artery around the cervix is also called the circular artery of the cervix. The uterine artery also circulates branches towards the fallopian tube and ureter as it goes across it. Cervicovaginal branches anastomose with vaginal arteries to create the azygos arteries of the vagina.
The arcuate arteries of uterus supply blood to the smooth musculature of the uterus called myometrium. The arcuate arteries penetrate throughout the circumference of the myometrium and supply blood to anterior and posterior walls of the uterus. The arcuate artery terminates in the spiral artery, which supplies the endometrium, decidua, and placenta during pregnancy. The rhythmic contraction and relaxation of these vessels help to maintain the endometrial stability and necessary control of blood supply. These vessels are usually demonstrated in the late luteal phase. Before the beginning of menses and during menses, these vessels are less apparent. Estrogen causes an increase in the size and the number of these vessels and increases blood flow. Estrogen is responsible for the proliferation of the uterine endometrium during the proliferative phase of the menstrual cycle.
The spiral arteries supply blood to the endometrium of the uterus, more specifically, the functional zone which sheds off during menstruation. In histology, identification of spiral arteries helps to make the diagnosis of the luteal phase of the menstrual cycle.
The basal arteries supply the blood to the endometrium, more specifically, the basal zone. The basal zone starts the regeneration of the denuded endometrium after menstruation. This regeneration happens under the influence of estrogen during the proliferative phase of the menstrual cycle. Maintenance of the stroma occurs with progesterone.[4]
Surgical Considerations
In pathological conditions like fibroid uterus, the course of uterine artery and its branches are distorted significantly. Uterine fibroids are most common uterine tumors in reproductive age of a female. The uterine artery supplies blood the growing fibroids, and this blood supply facilitates the growth of the fibroid. Most of the fibroids are benign and asymptomatic. Symptomatic fibroids may cause severe pelvic pain, dysmenorrhea, menorrhagia and iron deficiency anemia. Symptomatic fibroids are the most common indication of hysterectomy in the United States. Symptomatic fibroids are usually treated by surgery. After the reproductive age, uterine fibroids may be treated with gonadotropin-releasing hormone (GnRH) to shrink the fibroids. Uterine artery embolization blocks blood flow to fibroids, shrinking them in size; this radiological procedure may improve symptoms in many patients. It is not recommended during the reproductive period as it may cause atrophy of ovaries leading to menopausal symptoms.[5]
During a hysterectomy, it is important to isolate the descending ureter from the uterine artery to avoid injury to the ureter. A surgical injury to the lower ureter happens during a difficult surgery, such as in cases of a tubo-ovarian abscess, pelvic mass or various malignant conditions of pelvic organs. Many times, injuries of the ureter are missed during surgery. Postoperative cystoscopy and visualization of the free flow of a dye from both ureters may assure intact ureters.[6]
During a cesarean delivery, there may be excessive bleeding during the surgery. Suturing or compressing the uterus or medical management may not succeed. In this situation, bilateral uterine artery ligation may stop bleeding. Recanalization of uterine vessels automatically takes place after recovery.
Clinical Significance
Pregnancy is a physiological state where uterine smooth muscles and blood vessel proliferate continuously. In pregnancy, there is a considerable decrease in uterine vascular and muscular tone and a rise in uterine blood flow. The increased amount of steroid hormones during pregnancy, such as estrogen, progesterone, and cortisol, all affect uterine vasculature and musculature. Estrogen is a major factor in the increased size of the uterus and thickening of the uterine wall.[4]
The myometrium, the middle layer of the uterine wall, mainly consists of smooth muscle cells. The myometrium greatly enlarges during pregnancy. There is a lack of uterine contractions during the normal gestational period. The prevention of contraction is done through progesterone inhibition of myocytes. During pregnancy, the myocytes go under continuous stretching, hypertrophy, and remodeling. These physiological changes are necessary for a successful pregnancy. During early pregnancy, extravillous cytotrophoblasts invade the decidualized endometrium and myometrium. The spiral arteries transform into large vessels of low resistance that occur with a gradual loss of the normal musculo-elastic structure of the arterial wall. In preeclampsia or fetal growth retardation, the trophoblastic invasion and spiral artery dysfunction deters normal physiological changes.
During pregnancy, a uterine artery Doppler study may be used to scan uterine artery flow. This study shows the amount of uterine artery obstruction. In the cases of fetal growth retardation, diabetes, hypertensive disorders and preeclampsia, there is dysfunction of blood flow to the placenta and fetus. Uterine artery color imaging and pulsed wave Doppler ultrasound studies may be helpful to evaluate the uterine artery flow, mean arterial pressure, and uterine artery resistance index. Pregnant patients who have increased mean arterial pressure but a normal uterine artery resistance index may expect a favorable pregnancy outcome. Those with increased mean arterial pressure with an abnormal uterine artery resistance index may have an unfavorable outcome.
Increased uteroplacental blood flow is necessary for a normal outcome of pregnancy. This is accomplished through systematic growth and remodeling of the uterine circulation and formation of the placenta. During pregnancy, the diameter of the main uterine artery approximately doubles in size. There is no thickening of arterial wall during the enlargement of arterial diameter.
In postmenopausal women, calcifications may be found in the wall of arcuate arteries. These calcified patches are echogenic and appear as linear echoes with shadowing. This is a normal aging process which may be increased in diabetic patients. These calcified lesions are distinctive from calcified fibroids.