Continuing Education Activity
Urinary incontinence is the involuntary leakage of urine. This condition is prevalent in older adults but can also affect younger adults and significantly impacts both health and quality of life. The 5 main types include stress, urge, mixed, overflow, and functional incontinence. Possible treatments include lifestyle adjustments, physical therapy, pelvic floor exercises, fluid management strategies, prompted voiding, biofeedback, catheters (intermittent or permanent), pads, pharmaceuticals, botulinum toxin injections, sacral neuromodulation, bedside suction devices, and numerous procedures, including male and female slings, artificial sphincters, and prostate surgery.
This activity reviews the different types of urinary incontinence, effective screening practices, and evidence-based management strategies. Participants gain comprehensive knowledge of the latest diagnostic techniques and treatment modalities, enabling them to provide improved patient care. Clinicians also learn about the psychosocial aspects of the condition and how to address them, enhancing their ability to support patients holistically. This activity also highlights the role of the interprofessional team in the care of patients with urinary incontinence, leading to better clinical outcomes and improved quality of life for individuals affected by urinary incontinence.
Objectives:
Differentiate the etiologies of the various types of urinary incontinence.
Identify the key components in the evaluation of urinary incontinence.
Assess the management options available for the various types of urinary incontinence.
Implement interprofessional team strategies for screening and treating patients with urinary incontinence to improve health and quality of life outcomes.
Introduction
Urinary incontinence, the involuntary leakage of urine, is a common condition among older individuals, particularly those in nursing homes, but it can also affect younger adults of both sexes. This condition significantly impacts patient health and quality of life. The prevalence of urinary incontinence is likely underestimated, as many patients do not report their symptoms to healthcare providers for various reasons.[1]
There are several types of urinary incontinence—stress, urge, functional, mixed, and overflow incontinence. Initial evaluation typically does not require urologic or gynecologic assessment, but reversible causes should be ruled out. Management strategies depend on the type and severity of incontinence, and the patient's discomfort and morbidity.[2][1]
Etiology
The 5 types of urinary incontinence and their causes are as follows:[3][2]
Stress Urinary Incontinence
Stress urinary incontinence is the involuntary leakage of urine that occurs with increased intra-abdominal pressure during activities such as exertion, straining, Valsalva, sneezing, or coughing due to the urethral sphincter weakness, pelvic floor weakness, or urethral hypermobility. Young women active in sports may experience this type of incontinence.[4] In addition, pregnant women and women who have experienced childbirth may be prone to stress urinary incontinence. Stress incontinence in men is typically a complication of prostate surgery, resulting in sphincteric insufficiency. Please see StatPearls' companion resource, "Stress Incontinence," for further information.
Urge Incontinence
Urge incontinence is the involuntary leakage of urine that may be preceded or accompanied by a sense of urinary urgency (but can be asymptomatic as well) due to detrusor overactivity. The contractions may be caused by bladder irritation or loss of neurologic control. The condition may be caused by detrusor instability, overactive bladder, or neurological conditions such as stroke, Parkinson disease, or multiple sclerosis. Please see StatPearls' companion resource, "Urge Incontinence," for further information.
Mixed Urinary Incontinence
Mixed urinary incontinence is the involuntary leakage of urine caused by a combination of stress and urge urinary incontinence, as described above. Typically, either urge or stress incontinence is more predominant or bothersome. Please see StatPearls' companion resource, "Mixed Urinary Incontinence," for additional information.
Overflow Urinary Incontinence
Overflow urinary incontinence is the involuntary leakage of urine from an overdistended bladder due to impaired detrusor contractility and bladder outlet obstruction. Neurologic diseases such as spinal cord injuries, multiple sclerosis, and diabetes can impair detrusor function, resulting in a hypotonic neurogenic bladder. Bladder outlet obstruction can be caused by external compression by abdominal or pelvic masses, urethral strictures, and pelvic organ prolapse, among other causes. A common etiology in men is benign prostatic hyperplasia.
Overflow urinary incontinence is the only type of urinary incontinence considered directly physically dangerous, as it can lead to renal failure and permanent bladder damage. Please see StatPearls' companion resources, "Female Urinary Retention" and "Male Urinary Retention: Acute and Chronic," for further information.
Functional Urinary Incontinence
Functional urinary incontinence is the involuntary leakage of urine due to environmental or physical barriers to toileting. This type of incontinence is sometimes referred to as toileting difficulty.
Epidemiology
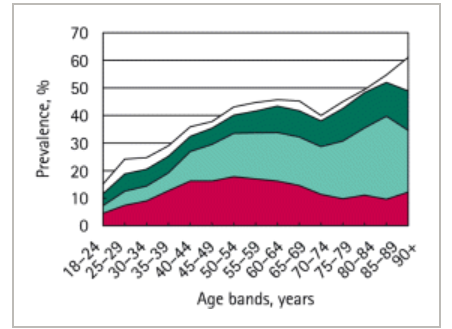
Accurate prevalence data are difficult to obtain due to underreporting, differing definitions for urinary incontinence, and varying study designs.[5][6] However, it is estimated that approximately 423 million individuals aged 20 or older worldwide experience some form of urinary incontinence (see Image. Types of Urinary Incontinence by Age Bands).[7]
In the United States, approximately 13 million individuals are directly affected by urinary incontinence. The prevalence is 50% or greater among residents of nursing facilities and rises to more than 75% among long-term (>100 days) residents.[8][9] Caregivers report that 53% of the homebound older individuals are incontinent. A random sampling of hospitalized older patients reports that 11% of patients have persistent urinary incontinence at admission and 23% at discharge.[6]
Approximately 24% to 45% of women reported urinary incontinence. Among women aged 20 to 39, 7% to 37% experience some degree of incontinence. In women older than 60, approximately 9% to 39% reported urinary incontinence on a daily basis. An increased risk of urinary incontinence is associated with pregnancy, childbirth, diabetes, and increased body mass index.
The overall prevalence of incontinence in men is about half that of women.[6] Urinary incontinence is reported in 11% to 34% of older men, with 2% to 11% reporting daily occurrences. Increased risk is associated with prostate surgery.[5]
The estimated overall prevalence for specific types of urinary incontinence is as follows:[2]
- Stress urinary incontinence: 24% to 45% in women older than 30
- Urge urinary incontinence: 9% in women aged 40 to 44, 31% in women older than 75, 42% in men older than 75 years
- Mixed urinary incontinence: 20% to 30% of those with chronic incontinence
- Overflow urinary incontinence: 5% of those with chronic incontinence
- Functional urinary incontinence: uncertain
Among adult women in the United States (approximately 80 million individuals), over 60% report some degree of urinary incontinence, with one-third experiencing leakage at least monthly.[10] The most common incontinence type reported was stress (37.5%), followed by mixed (31.3%) and urge incontinence (22%).[10]
History and Physical
A thorough history and physical examination are essential in evaluating patients with urinary incontinence. This comprehensive assessment helps identify the underlying causes, differentiate between types of incontinence, and guide appropriate management strategies.
History
The history should be used to determine the type, severity, burden, and duration of urinary incontinence. Voiding diaries may help provide details about episodes of incontinence. Signs and symptoms of emergent conditions, such as cauda equina syndrome, and reversible causes should be investigated.
The history can often determine the type of urinary incontinence:
- Stress urinary incontinence: Patients can generally predict the inciting activity, typically laughing, coughing, abdominal straining, or sneezing.
- Urge urinary incontinence: Frequency, urgency, and nocturia may be present. There is variable volume loss, ranging from almost nothing to flooding. Bladder post-void residual urine volume is typically low.
- Mixed urinary incontinence: There are characteristics of both stress and urge incontinence. This type helps determine which component is most predominant or bothersome.
- Overflow urinary incontinence: This condition is associated with poor bladder emptying or urinary retention in both men and women. Post-void residual urine volume is typically very high, and the patient may note the need to strain. Please see StatPearls' companion resources, "Female Urinary Retention" and "Male Urinary Retention: Acute and Chronic," for more information.
- Functional urinary incontinence: The history may suggest physical or cognitive impairment.
The 3 incontinence questions is a brief questionnaire that may be useful to distinguish among stress, urge, mixed urinary incontinence, and other causes. The 3 incontinence questions predict stress urinary incontinence with a specificity of up to 92%, but its utility may depend on the population studied.[11][12]
Patients should be asked about medical conditions such as chronic obstructive pulmonary disease and asthma, which can cause cough; heart failure, with related fluid overload and diuresis; neurologic conditions, which may suggest dysregulated bladder innervation; and musculoskeletal conditions, which may contribute to toileting barriers.
Surgical history should also be assessed as the anatomy and innervation involved may have been affected by prior surgeries. Male stress incontinence, for example, is almost always due to postoperative complications from urologic surgery. Please see StatPearls' companion resource, "Slings for Male Incontinence," for further information.
For females, obtaining a gynecologic history should be obtained to assess the number of births, mode of deliveries (vaginal or Cesarean section), and current pregnancy status. In addition, estrogen status should be determined as atrophic vaginitis and urethritis may contribute to reversible urinary incontinence during perimenopause.
Patients should be asked about their medication and substance use, such as diuretics, alcohol, and caffeine, as they can either directly or indirectly contribute to incontinence. Potential adverse effects include impaired cognition, alteration of bladder tone or sphincter function, cough induction, and promotion of diuresis.
Symptom severity and patient therapeutic preferences are ascertained, along with possible surgical tolerance and acceptability, to determine the appropriate degree of treatment aggressiveness.[2][13]
Physical Examination
A thorough patient history should guide the clinician toward an appropriate physical examination. Emergent conditions and reversible causes should be explored.
Components and findings of Physical examination that should be assessed, if appropriate, include:
- Cardiovascular: Pedal edema and jugular venous distension
- Pulmonary: Pulmonary crackles and cough
- Abdominal: Masses and surgical scars
- Genitourinary/rectal: Bladder distension, vaginal atrophy, pelvic organ prolapse, prostatic hypertrophy, fecal impaction, and rectal tone
- Musculoskeletal: Extremity strength, range of motion, and overall function
- Neurologic: Cognitive function, sensation, and reflexes [2][13]
Optional tests and maneuvers to consider are as follows:
Cough stress test: The patient is asked to cough to demonstrate the involuntary leakage of urine. The test is more sensitive when performed in a standing position.[13] A Valsalva urinary stress test is similar.
Cotton swab test: The female patient is asked to Valsalva after insertion of a lubricated cotton swab placed just into the bladder through the urethra to demonstrate the degree of urethral hypermobility (associated with stress urinary incontinence), with an angle change >30° being a positive result. There may be poor agreement of the test result when the angle is from 21° to 49°.[14]
Pediatric Foley catheter test: This test is used to screen for intrinsic sphincteric deficiency, a subtype of stress incontinence. An 8-French pediatric Foley catheter is placed in the bladder, the balloon is inflated, and the catheter is gently withdrawn. If the catheter, with its bulb inflated, can be easily extracted from the urethra, the test is positive, suggesting intrinsic sphincteric deficiency.[15] This diagnosis is confirmed if the cotton swab test is negative, indicating no urethral hypermobility.[15]
Evaluation
The evaluation of urinary incontinence should include a focused but detailed history and thorough physical examination. Potentially reversible causes, including abnormal sleep patterns, fluid overload, misuse of diuretics, and similar entities, should be identified. Medication reconciliation should be carried out, and comorbidities should be determined.[2][13][16] Minimal laboratory testing or imaging is required for evaluation. Most laboratory and diagnostic tests are used to rule out other harmful conditions and sequelae.[2][13][16]
Urinalysis should be performed on all patients to assess for urinary tract infection, glycosuria, proteinuria, and hematuria. A urine culture is indicated in all cases suspected of an infection. Serum blood urea nitrogen and creatinine should be performed to assess renal function if an obstruction is suspected.
Post-void residual volume should be evaluated, particularly if overflow urinary incontinence is suspected. A bladder ultrasound is performed after a patient voids, either as a formal ultrasound examination or by a dedicated bladder ultrasonic scanner. Detection of >200 mL of urine remaining in the bladder after voiding suggests overflow urinary incontinence and possible bladder hypotonicity. High post-void residuals suggest inadequate emptying, hypotonic bladder function, and possible overflow incontinence. Low post-void residuals are more common with urge incontinence and overactive bladder symptoms. Please see StatPearls' companion resource, "Bladder Post Void Residual Volume," for more information.
A 24-hour or 3-day voiding diary may be helpful in selected cases.[17][18] The patient is instructed to write down and record the time and the amount of urine voided in mL for at least a full 24 hours. Overactive bladder patients tend to void in small volumes frequently throughout the entire period. Patients with global polyuria have relatively large voided urine volumes throughout the day and night, with very large total volumes. A normal 24-hour urine total volume is about 1300 mL. More than 3000 mL is considered polyuria.
A 24-hour pad test is used to assess the severity of urinary incontinence in selected patients and can also be repeated to track the success of treatment. Weighed pads are used by the patient until they become soaked or at 6 hours. They are weighed again when changed, and the difference between the 2 weights represents the amount of urine leaked. Mild incontinence is up to 20 g, 21 to 74 g is moderate, and 75 g or more is considered severe.[19][20]
A renal ultrasound should be considered to assess hydronephrosis in cases of suspected obstruction and in patients with renal failure. Urodynamic testing is unnecessary except for complicated (intractable) cases or if surgery is being considered.[21] Please see StatPearls' companion resource, "Urodynamic Testing and Interpretation," for more information.
Treatment / Management
Treatment and management of urinary incontinence depends on its type. Conservative, pharmacologic, and surgical treatment modalities exist. Medications should be reconciled, and substances such as caffeine and alcohol should be avoided if they are contributing to the patient's incontinence. Treatment should begin with the least invasive methods and then escalate as appropriate.[2][13][22]
Type-specific treatment strategies include the following:
Stress Urinary Incontinence
- Conservative management: Behavioral therapy, including controlling fluid intake, prompted voiding, bladder training, and constipation management; electrical stimulation; mechanical devices, such as cones, pessaries, and urethral plugs; physical therapy; biofeedback; pelvic floor muscle strengthening, such as Kegel and floor muscle exercises; weight loss; pads, such as diapers; condom catheters; and dietary adjustments, such as eliminating caffeine and other irritants.
- Pharmacologic management: Alpha-adrenergic agonists, such as phenylpropanolamine; duloxetine (not FDA-approved; imipramine; vaginal estrogen cream; and overactive bladder pharmaceutical agents as appropriate.[23]
- Surgical management: Trans- or periurethral injections of bulking agents, sling procedures, urethropexy, implantable dual-balloon adjustable continence device, and artificial sphincters.
Urge Urinary Incontinence
- Conservative management: Similar to the treatment for stress urinary incontinence with the exception of mechanical devices.
- Pharmacologic management: Antimuscarinics, such as darifenacin, solifenacin, oxybutynin, tolterodine, fesoterodine, and trospium;[24] topical vaginal estrogen (not FDA-approved); mirabegron; vibegron; and imipramine.
- Surgical management: Sacral neuromodulation, tibial nerve stimulation, onabotulinum toxin A bladder injections, and augmentation cystoplasty.
Mixed Urinary Incontinence
- As mentioned above, treatment and management focus on the most dominant symptoms.
- Please see StatPearls' companion resource, "Mixed Urinary Incontinence," for further information.
Overflow Urinary Incontinence
- Conservative management: Clean intermittent catheterization, indwelling urethral catheter, and relief of obstruction.
- Pharmacologic management: Bethanechol, a detrusor stimulant, and alpha-adrenergic antagonists, such as doxazosin, terazosin, tamsulosin.[23]
- Surgical management: Suprapubic catheter and transurethral prostate resection, if detrusor muscle tone is sufficient and capable of generating at least 30 to 35 cm of water pressure.
Functional Urinary Incontinence
Underlying causes should be addressed and alleviated if possible.
Differential Diagnosis
Establishing a differential diagnosis for urinary incontinence is crucial for identifying the specific type and underlying cause of the condition. This process involves distinguishing between various forms of incontinence, such as stress, urge, overflow, and functional incontinence, and ruling out other potential medical issues. A thorough differential diagnosis ensures appropriate and targeted treatment for each patient.
The mnemonic DIAPPERS can be used as an aid to develop a differential diagnosis for reversible causes of urinary incontinence:
- Delirium, dementia, or other cognitive impairments
- Infection (urinary tract infection)
- Atrophic vaginitis or urethritis
- Pharmaceuticals or substances, such as diuretics, caffeine, and alcohol
- Psychological disorder
- Excessive urine output, such as diabetes and diabetes insipidus
- Reduced mobility or reversible urinary retention
- Stool impaction [2]
Other conditions to consider include the following:
- Anatomic abnormalities such as urogenital fistulas, diverticula, renal duplication, and ectopic ureters (though these are less common)
- Hydronephrosis
- Intra-abdominal or pelvic mass
- Interstitial cystitis
- Neurologic conditions such as spinal cord injuries, cauda equina syndrome, multiple sclerosis, cerebral vascular accidents, normal pressure hydrocephalus, spinal stenosis, Parkinson disease, and diabetic neuropathy
- Pelvic organ prolapse
- Polyuria
- Urinary tract infection
- Urolithiasis (especially distal ureteral calculi)
- Vesicoureteral reflux [25]
Prognosis
Response to treatment and management varies among patients. For those whose symptoms cannot be eliminated, optimal symptom control should be sought by multiple treatment modalities. Median cure rates for stress, urge, and mixed urinary incontinence by select modalities are as follows:[26]
Stress Urinary Incontinence
- 58.8% at 12 months for women who used supervised pelvic floor muscle training.
- 78% at 6 months for men that used pelvic floor muscle training.
- 84.4% at 12 months for women who received surgical interventions.
- 50% of patients who received an artificial urinary sphincter have complete continence after 5 years, whereas another 40% can manage with only 1 pad per day. Please see StatPearls' companion resource, "Artificial Urinary Sphincters and Adjustable Dual-Balloon Continence Therapy in Men," for further information.
- 55% of patients who received a dual-balloon adjustable continence device reported long-term cures or substantially reduced leakage. Please see StatPearls' companion resource, "Artificial Urinary Sphincters and Adjustable Dual-Balloon Continence Therapy in Men," for further information.
- 75% of properly selected men who received a sling indicated a cure or a substantial improvement in their stress urinary incontinence. Please see StatPearls' companion resource, "Slings for Male Incontinence," for further information.
- 53% after 3 years for males who received slings.
Urge Urinary Incontinence
- 49% at 12 months for women who used antimuscarinics.
- 15.9% to 50.9% at 3 months in women who used onabotulinum toxin A.
- 17% at 10 years for women who used sacral neuromodulation.
- 24% to 35% at 12 months for men who used supervised pelvic floor muscle training.
Mixed Urinary Incontinence
- 28% at 6 months for women with supervised pelvic floor muscle training.
- 47% of men who used supervised pelvic floor muscle training.
- 82.3% of women who received surgical interventions.
Several inventories and tools may be used to monitor symptoms and treatment effectiveness.
- Michigan incontinence symptom index (M-ISI): This questionnaire assesses the frequency of urinary incontinence, the amount of protection used, and the impact of urinary incontinence on daily activities.[27]
- International consultation on incontinence questionnaire form (ICIQ-UI short form): This questionnaire has high intra- and interobserver reliability.[28]
- Sandvik questionnaire (incontinence severity index): This questionnaire assesses the frequency and amount of leakage and is highly correlated with the ICIQ-UI short form.[29]
- 24-hour pad test.[19][20]
Complications
Urinary incontinence can lead to many complications that significantly impact a patient's health and quality of life. These complications range from physical issues, such as skin infections and urinary tract infections, to psychological effects, including anxiety and depression. In addition, the condition can cause social isolation and decreased mobility. Understanding the complete scope of complications is crucial for comprehensive patient care.
The complications associated with urinary incontinence include the following:[13][23][30]
- Cellulitis
- Decreased physical activity and libido
- Depression
- Increased caregiver burden
- Increased risk of falls and subsequent fractures
- Mechanical failure (leak)
- Medication adverse effects
- Alpha-adrenergic agonists: Dry mouth, restlessness, hypertension, and insomnia.[23] Please see StatPearls' companion resource, "Adrenergic Drugs," for more information.
- Alpha-adrenergic antagonists: Hypotension, dizziness, fatigue, and sedation.[31] Please see StatPearls' companion resources, "Alpha-Blockers" and "Phenoxybenzamine," for more information.
- Antimuscarinics: Dry mouth, constipation, blurred vision, dry eyes, fatigue, difficulty in micturition, and palpitations.[26] Please see StatPearls' companion resource, "Muscarinic Antagonists," for more information.
- Duloxetine: Dry mouth, nausea, fatigue, constipation, and hyperhidrosis.[31] Please see StatPearls' companion resource, "Duloxetine," for more information.
- Mirabegron and vibegron: Urinary tract infections and hypertension.[30][32] Please see StatPearls' companion resource, "Mirabegron," for more information.
- Onabotulinumtoxin A injection: Urinary tract infections and urinary retention [31]
- Pressure ulcers
- Renal dysfunction secondary to obstructive uropathy
- Sexual dysfunction
- Social isolation
- Trauma and infection due to catheterization
- Treatment failure
- Urethral erosion
- Urinary tract infections
- Worsening of urinary incontinence after surgical intervention
Consultations
Consultations play a vital role in effectively managing urinary incontinence, ensuring comprehensive care tailored to individual patient needs. These consultations involve specialists such as urologists, gynecologists, and geriatricians, who provide expertise in diagnosing the type and severity of incontinence. They also guide personalized treatment plans, incorporating both conservative and surgical interventions when necessary to improve patient outcomes and quality of life.
Further evaluation is warranted and recommended in the following situations:[2]
- Incontinence associated with relapse
- Incontinence associated with recurrent symptomatic urinary tract infections
- Incontinence with new-onset neurologic symptoms
- Marked prostate enlargement
- Neurogenic bladder
- Pelvic organ prolapsed past the introitus
- Pelvic pain associated with incontinence
- Persistent or unexplained hematuria
- Persistent proteinuria
- Postvoid residual volume >200 mL
- Previous pelvic surgery or radiation
- Spinal cord injury
- Surgical complication
- Treatment failure
- Uncertain diagnosis
Deterrence and Patient Education
Deterrence and patient education are crucial in effectively addressing urinary incontinence. Patients and their families should be informed that although urinary incontinence is highly prevalent in older adults, it is not a normal part of aging. They should be aware that many causes of urinary incontinence are reversible, and all cases are treatable to some degree.
Educating patients about risk factors such as obesity, chronic cough, and pelvic floor weakness can empower them to adopt preventive measures, including weight management and regular pelvic floor exercises. Patient education also encompasses understanding the types and causes of incontinence, managing fluid intake, and recognizing symptoms early. Education about the various treatment and management options available, including conservative, pharmacologic, and surgical modalities, is essential.
Promoting open communication encourages patients to seek timely medical advice, reducing stigma and promoting proactive management strategies. By emphasizing education and preventive measures, healthcare professionals can significantly enhance patient awareness and self-management of urinary incontinence.
Pearls and Other Issues
In some cases, an incontinence system using a special pad and a bedside vacuum drainage system can provide symptomatic relief of wetness to bedridden patients even if the incontinence cannot be controlled.[33][34] Male and female incontinence pads are available.
Urinary incontinence in end-of-life care can be challenging to manage and should be handled on a case-by-case basis. In some instances, an indwelling catheter or condom catheter may be used to maximize patient comfort during the last stages of life.
Enhancing Healthcare Team Outcomes
Enhancing patient-centered care and outcomes related to urinary incontinence requires a collaborative approach involving physicians, advanced care practitioners, nurses, pharmacists, and other healthcare professionals. Clinicians need proficiency in comprehensive assessment skills to accurately diagnose and classify the type of urinary incontinence, ensuring tailored treatment plans. Strategic management involves integrating evidence-based practices with patient preferences and promoting shared decision-making and autonomy.
Pharmacists can provide critical input and assist with medication reconciliation. They help minimize unwanted anticholinergic effects of patient medications and suggest dosage adjustments for patients with renal failure. In more complicated cases of urinary incontinence, collaboration among primary care clinicians and specialists is needed to deliver seamless, quality care to patients.
The responsibilities of the interprofessional healthcare team include ongoing education on the latest treatment modalities and patient education strategies, empowering individuals to actively participate in managing their condition. Interprofessional communication is crucial for cohesive care delivery, fostering teamwork, and reducing medical errors. Care coordination ensures seamless transitions between healthcare settings, optimizing continuity of care and patient safety.