Continuing Education Activity
Tympanocentesis is a minor surgical procedure used to treat otitis media and many otologic disorders. Otitis media is a prevalent condition characterized by infection or inflammation of the middle ear and is a common reason individuals seek medical attention from pediatricians, family practitioners, and urgent-care healthcare professionals. Tympanocentesis involves puncturing the tympanic membrane with a small-gauge needle and removing fluid behind the eardrum for therapeutic and diagnostic purposes. Due to the widespread availability of antimicrobial drugs, many clinicians empirically treat otitis media without aspirating middle ear fluid for culture to guide antibiotic selection.
Currently, clinicians perform the tympanocentesis procedure for treating otitis media cases unresponsive to conventional antibiotic therapy, particularly those involving multidrug-resistant otopathogens, and for managing other otologic disorders, including retraction of the tympanic membrane, Ménière disease, and sudden sensorineural hearing loss. Tympanocentesis reduces the risk of treatment failure, susceptibility to otitis, and the need for tympanostomy tube placement while also serving as a conduit for the drainage of otorrhea. This activity describes the indications, contraindications, techniques, and potential complications associated with tympanocentesis, equipping healthcare professionals with the knowledge and tools to enhance patient care.
Objectives:
Identify the clinical scenarios where tympanocentesis is indicated, distinguishing cases of recurrent or refractory otitis media and specific otologic disorders that may benefit from this procedure.
Screen patients presenting with otitis media for factors that may warrant tympanocentesis, including treatment unresponsiveness and the presence of multidrug-resistant otopathogens.
Apply knowledge of indications, contraindications, and potential complications to make informed decisions regarding tympanocentesis in clinical practice.
Collaborate with other healthcare professionals, particularly otolaryngologists and infectious disease specialists, to optimize patient outcomes through a coordinated and interdisciplinary approach.
Introduction
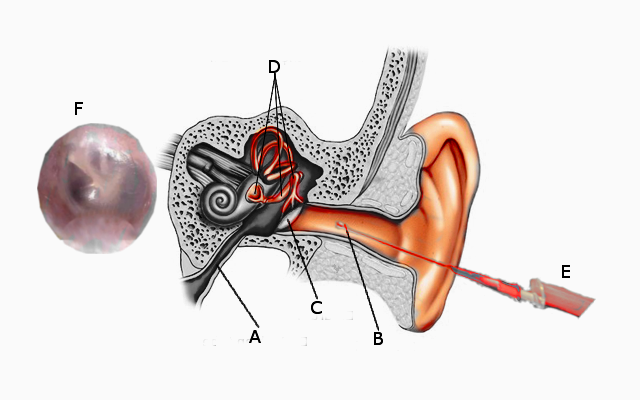
With the advent of antibiotics, many interventions and treatments previously used for infectious diseases, such as tympanocentesis, have become less utilized. Tympanocentesis is a minor surgical procedure used to treat otitis media and many otologic disorders. The procedure involves puncturing the tympanic membrane with a small-gauge needle and removing fluid behind the eardrum for therapeutic and diagnostic purposes (see Image. Tympanocentesis). Tympanocentesis was first documented in 1768 and has been used to manage ear diseases, particularly otitis media, and has undergone significant advancements.
Otitis media is a prevalent condition characterized by infection or inflammation of the middle ear and is a common reason individuals seek medical attention from pediatricians, family practitioners, and urgent-care healthcare professionals. The common subtypes of otitis media include acute otitis media, adhesive otitis media, otitis media with effusion, and chronic suppurative otitis media.[1]
Currently, clinicians perform the tympanocentesis procedure for treating otitis media cases unresponsive to conventional antibiotic therapy, particularly those involving multidrug-resistant otopathogens, and for managing other otological disorders, including retraction of the tympanic membrane, Ménière disease, and sudden sensorineural hearing loss (SSNHL).[2]
Due to the widespread availability of antimicrobial drugs, many clinicians empirically treat otitis media without aspirating middle ear fluid for culture to guide antibiotic selection. Tympanocentesis reduces the risk of treatment failure, susceptibility to otitis, and the need for tympanostomy tube placement while also serving as a conduit for the drainage of otorrhea.
Anatomy and Physiology
The human ear is responsible for hearing and maintaining the balance of our body. The human ear comprises the following 3 parts (see Image. Ear Anatomy):
- The outer ear, containing the auricle or pinna and the external auditory canal
- The middle ear, and
- The inner ear, containing the cochlea and vestibular system
The topic being discussed is centered around the middle ear.
The Middle Ear
The middle ear is located within the aerated middle ear cleft of the tympanic portion of the temporal bone and functions as an amplification medium for acoustic energy collected from the external ear via the pinna and tympanic membrane. Subsequently, this acoustic energy is transmitted to the ossicles, the fluid-filled structures of the inner ear, and the eighth cranial nerve.
The middle ear comprises the following structures:
- Bones or ossicles: Malleus, incus, and stapes
- Round and oval windows
- Muscles: Stapedius and the tensor tympani
- Nerves: The facial nerve, the chorda tympani nerve, and the tympanic nerve plexus
- Eustachian tube orifice
- Aditus ad antrum: It refers to the entrance to the mastoid cavity
Embryology
The ossicles of the middle ear originate from neural crest cells of the first and second arch mesenchyme. In contrast, the tympanic cavity originates from the first pharyngeal pouch and maintains its embryologic connection to the nasopharynx via the eustachian tube. The mesodermal layers of the first and second arches give rise to the muscles of the middle ear—the stapedius and tensor tympani— which dampen the transmission of loud sounds to the cochlea. The tympanic cavity consists of 2 parts—the tympanic cavity proper and the epitympanic recess—both of which are in continuity with the air cells of the mastoid bone.[3]
Tympanic Membrane
The tympanic membrane is an oval-shaped, thin, semitransparent membrane measuring approximately 1 cm in diameter in adults and separates the external auditory canal and the middle ear cavity. The 2 primary components of the tympanic membrane are mentioned below.
The pars flaccida: The pars flaccida of the tympanic membrane is situated in the posterior superior portion of the eardrum above the malleolar folds and consists of an inner mucosal layer and an outer squamous layer. The chorda tympani lies on the internal surface of the tympanic membrane in this area.
The pars tensa: The pars tensa constitutes the remaining part of the eardrum and comprises 3 layers—external squamous, middle fibrous, and internal mucosal. Connected to the malleus and surrounding the umbo, the pars tensa is the segment of the tympanic membrane crucial for sound transmission. The manubrium of the malleus bone is connected to the middle portion of the tympanic membrane, allowing direct transmission of acoustic vibrations to the incus and the stapes. Needle placement in tympanocentesis is done through the pars tensa, preferably in the anterior inferior or posterior inferior quadrant of the membrane. Importantly, instrumenting the posterior superior quadrant should be avoided to prevent potential damage to the underlying incus and stapes.
Physiology
Eustachian tube dysfunction can result in chronic negative pressure and the accumulation of transudate fluid in the middle ear space. Due to the airtight nature of the tympanic membrane, the sole mechanism for equalizing middle ear pressure with environmental pressure is through the Eustachian tube. The fluid accumulation in the middle ear dampens tympanic membrane vibrations, causes hearing loss, and creates a potential site for infection. Microorganisms from the nasopharynx can colonize this space by traversing the Eustachian tube. If this fluid persists for an extended period, the middle ear mucosa absorbs the aqueous component. However, the mucoid proteins persist, resulting in a viscous fluid unlikely to resolve without manual removal. This condition is sometimes referred to as "glue ear."
Indirect communication between the middle and inner ear occurs through the round window and, to a lesser extent, the oval window, which is covered by the stapes footplate. These connections facilitate the osmotic transmission of inflammatory mediators and other molecules between the middle and inner ear spaces. One theory regarding the etiology of SSNHL suggests that the transmission of viral particles from the middle ear space to the inner ear during an upper respiratory infection may occur, potentially causing damage to cochlear elements.
Indications
Tympanocentesis has both diagnostic and therapeutic indications. Diagnostically, tympanocentesis facilitates culture and sensitivity analysis of the aspirate. In contrast, therapeutically, tympanocentesis allows for the direct administration of medication to the middle ear and improves hearing via physical removal of middle ear fluid.
Therapeutic Indications for Tympanocentesis
Otalgia relief: Pain is a classic symptom associated with various otologic disorders. Otitis media, an inflammatory disease of the middle ear, may manifest with pain along with other clinical symptoms. Patients, particularly pediatric patients, experiencing severe otalgia due to acute otitis media can be acutely managed with tympanocentesis while awaiting results from a course of antibiotics.
Administration of medications: Tympanocentesis facilitates the administration of intratympanic drugs, including antibiotics and corticosteroids, to manage otological disorders.[4] In cases of Ménière disease refractory to hydrochlorothiazide, betahistine, and a low-salt diet, treatment options may include intratympanic steroid injections or gentamicin to ablate the vestibular system if steroid injections fail.[5][6][7] Intratympanic steroid injections, often used in conjunction with systemic oral steroids, are a cornerstone of treatment for SSNHL.[8][9] Patients with Bell palsy have demonstrated benefits from intratympanic steroid injections, along with oral steroids and antivirals, especially in cases where the prognosis is deemed poor based on history and physical examination findings.[10][11]
Diagnostic Indications for Tympanocentesis
Acute otitis media in an immunocompromised patient: Identifying and effectively managing the causative organism for acute otitis media in an immunocompromised host can be challenging. In such cases, patients may not respond clinically in predicted ways, and tympanocentesis allows the clinician to conduct a microbiologic culture and analysis of the ear aspirate, enabling culture-directed therapy.[12][13]
Unresolved acute otitis media: For patients with an episode of acute otitis media that is unresponsive to 2 standard courses of antibiotics or with recurrent episodes of acute otitis media, a diagnostic tympanocentesis may be warranted for identification of the pathogens and determination of antimicrobial susceptibility before the selection of a third line antimicrobial agent.[12][13][14]
Acute otitis media in neonates: Managing acute otitis media in neonates or infants poses challenges for clinicians. Tympanocentesis can aid in distinguishing acute otitis media from sterile middle ear fluid in neonates with a fever of unknown origin. These patients are more prone to atypical pathogens causing acute otitis media than the general population.
Management of tympanic membrane retraction: Although tympanocentesis is not a standalone management modality for patients with retracted tympanic membranes, it can assist clinicians in determining whether the insertion of a ventilation tube may aid in elevating the retracted tympanic membrane. This is particularly relevant in clinical scenarios where pneumatic otoscopy is unavailable, as air can be gently instilled into the middle ear space to evaluate the clinical and hearing response.[13]
Electrocochleography: Electrocochleography is a method commonly used for diagnosing Ménière disease by monitoring cochlear potentials and can be performed in either an invasive or noninvasive manner. The invasive approach involves passing the electrode through the tympanic membrane onto the cochlear promontory in the middle ear, offering clearer tracing of electrical potentials.
Contraindications
Performing a tympanocentesis is not recommended in certain situations. Below are some contraindications to consider.
Uncooperative patient: Uncooperative patients pose a contraindication to tympanocentesis, as the procedure requires absolute patient cooperation for safe execution.
Intact tympanostomy tubes: Tympanocentesis is contraindicated in patients with intact tympanostomy tubes.
Intratympanic tumor: Tympanocentesis is contraindicated in patients with intratympanic tumors such as globus tympanicum, facial neuroma, and meningioma, as it carries the risk of causing bleeding, facial paralysis, and cerebrospinal fluid leak, respectively.
Acute otitis external: Tympanocentesis is relatively contraindicated in cases of acute otitis externa due to the potential risk of introducing bacteria or fungi into the middle ear, as well as the challenge of visualizing the tympanic membrane caused by edema in the external auditory canal.
Vascular abnormalities: Tympanocentesis is contraindicated in patients with vascular abnormalities, such as a high-riding jugular bulb, due to the associated risk of bleeding.
Suboptimal visibility: Tympanocentesis requires optimal visibility of critical landmarks for safe execution.
Equipment
Successful performance of tympanocentesis necessitates a range of equipment and tools, including:
- Jobson Horne probe or cerumen loop
- Otologic microscope
- Topical anesthesia
- Lidocaine 4% instilled into the external auditory canal
- Micro-cotton balls soaked in phenol or 4% cocaine solutions to anesthetize the planned tympanocentesis site
- Lidocaine 2.5% and prilocaine 2.5% (EMLA) cream
- A syringe of 3 cc
- Sterile culture swabs and culture media
- A spinal needle of 3-inches, 20- or 21-gauge, with a tympanocentesis aspirator
- Appropriate procedural chair and procedural restraint board as needed
- Examination specula of various sizes
- Suction
- Tissue wicks
- Cotton balls
- Hydrogen peroxide of 3% concentration
- Iontophoresis device and electrodes (optional)
Personnel
Tympanocentesis is typically carried out by otolaryngologists, pediatricians, and family physicians. Generally, the procedure is performed in an office setting using local or topical anesthetic agents. Usually, an assistant aids the operating clinician in preparing the necessary equipment and passing instruments during the procedure.[15] An audiologist performs the test in electrocochleography, while an otolaryngologist places the monitoring electrode.
Preparation
Procedural Education and Informed Consent
As with any other surgical procedure, patients meeting the indications for tympanocentesis should receive a detailed explanation of the procedure, with clear information on the benefits, risks, and alternative options. Following this, the clinician obtains written informed consent.
Antibiotics
No preoperative antibiotics are necessary to administer before undergoing a tympanocentesis procedure.
Anesthesia
Patients can undergo tympanocentesis with topical, local, or general anesthesia. The use of general anesthesia requires the availability of additional trained personnel. Anesthesia is beneficial for patients who may be uncooperative, such as children or those with developmental disabilities or neuropsychiatric conditions. Topical agents such as lidocaine, prilocaine, and phenol are used in patients who cooperate with the procedure. These agents are associated with faster recovery time, reduced bleeding tendencies due to the vasoconstrictive properties of these agents, and an overall reduced procedural cost.
Newer noninvasive alternatives, such as iontophoresis and the application of EMLA cream, provide additional options. Acetaminophen with codeine is a suitable choice for oral pain relief during the procedure. Intravenous agents, such as midazolam, necessitate additional expertise, typically from an anesthesiologist or conscious sedation nurse, and are often administered in an operating room setting.
Positioning
The standard positioning for a patient undergoing tympanocentesis is the supine or semi-reclined position, with the patient's head turned away from the operator to facilitate proper visualization of the tympanic membrane using the appropriately sized ear speculum.
Technique or Treatment
To ensure a successful tympanocentesis procedure, clinicians should follow the following steps:
- Position the patient as described above in the Preparation section.
- Place the largest aural speculum that will fit comfortably into the ear and remove any cerumen within the ear canal.
- Administer the required anesthetic agent. Notably, topical anesthetic agents have bacteriostatic properties, necessitating the removal of excess anesthetic solution before conducting a culture.
- Connect the 3 cc syringe to the 20- or 21-gauge spinal needle and make a 45º bend at the tip of the spinal needle to ensure adequate visualization beyond the needle while in the external auditory canal.
- Carefully advance the needle with great care to the anesthetized portion of the tympanic membrane.
- Carefully advance the needle 2 mm through the inferior aspect of the tympanic membrane at the maximum bulge, upon reaching the tympanic membrane, thereby ensuring placement only in the anterior inferior or posterior inferior quadrant.
- Gently aspirate the fluid from the middle ear using the tip of the needle if fluid is present.
- Create a secondary perforation, often referred to as a "borehole," if intratympanic administration of medication is necessary. This technique relieves pressure by allowing air to escape while injecting the drug, thereby preventing barotrauma to the round window. Alternatively, the placement of a pressure-equalization tympanostomy tube is a viable option. The clinicians should warm any injected medication beforehand by rubbing the vial between two hands or keeping it in a trouser pocket to bring it close to body temperature. Instilling cold fluid into the ear may induce a convection current in the lateral semicircular canal, leading to vertigo.
- Carefully remove the needle and speculum from the patient's ear.
- Use a laser tympanostomy with a special adaptor on the carbon dioxide laser to create a small perforation.
- Irrigate the ear canal with a 3% hydrogen peroxide solution and a tissue wick to absorb any excess fluid, if appropriate.
- Send the aspirated fluid for the appropriate laboratory pathogen analysis and sensitivity testing.
Complications
Although tympanocentesis is considered a relatively safe procedure, the potential complications are mentioned below.
Bleeding: Bleeding during tympanocentesis is typically minimal, and achieving hemostasis is usually straightforward and rapid. Any suspicion of a high-riding jugular bulb is a contraindication to this procedure.
Pain: Despite the use of topical anesthetic agents, the medial aspect of the tympanic membrane can still retain some sensitivity, potentially causing the patient to experience discomfort.
Chronic perforation of the tympanic membrane: There is a slight risk of a non-healing perforation and potential damage to other middle ear structures, such as the ossicles and the facial nerve. However, the likelihood is low when the procedure is carefully performed.
Ossicular damage: Ossicular damage is prevented by refraining from instrumenting the posterior superior quadrant of the tympanic membrane, where the ossicles are located.
Clinical Significance
Otitis media may be overdiagnosed, potentially resulting in the prescription of antibiotics for sterile middle ear effusions. This overdiagnosis contributes to increased antibiotic administration, elevating the risk of antibiotic resistance within the community.
In a study published in 2015 by Pichichero and Poole, pediatricians from Greece, Italy, South Africa, and the United States were compared, revealing a tendency to confuse otitis media with effusion with acute otitis media.[15] A 2010 study by Rogers et al demonstrated that it can be challenging for many clinicians, including otolaryngologists, to determine the presence of fluid in the middle ear space before tympanostomy.[16] Pichichero also evaluated the diagnostic accuracy of tympanocentesis skills in a conference involving both pediatricians and otolaryngologists. The study revealed that 50% of pediatricians correctly diagnosed acute otitis media compared to otitis media with effusion. On the other hand, 73% of otolaryngologists achieved the same level of accuracy.[17] However, only 83% of pediatricians routinely performed tympanocentesis compared to 89% of otolaryngologists, indicating variations in cultural and practical preferences among respondents from different countries of origin.[18]
According to a 2000 study by Pichichero, tympanocentesis is considered the gold standard for confirming otitis media. This procedure provides the ability to analyze fluid collected from the middle ear, identify microbes, and determine antimicrobial susceptibility. In addition, the procedure also considers various factors influencing the decision to perform the procedure instead of empirically treating for acute otitis media.[19]
In a 2004 survey among Canadian pediatricians and family physicians, only 4% of the participants had received training to perform tympanocentesis, and none had performed it by the time of the study. The paper also highlighted that most clinicians trained to perform tympanocentesis had completed medical school before 1970, suggesting that the procedure is no longer commonly taught to primary care clinicians.[20]
In 2002, Steinbach et al. reported that few pediatric and family medicine residency programs across the United States and Canada included tympanocentesis training in their curriculum. Current practice patterns in the West often lean toward empiric treatment of acute otitis media with antibiotics and adopt a watchful waiting approach for otitis media with effusion unless the patient is in the language-development years when the placement of pressure equalization tubes is common. Tympanocentesis is a valuable skill for the clinician practicing in an environment where antibiotic compliance and patient follow-up pose challenges. This procedure can direct or avoid antibiotic treatment, offering relief and helping to mitigate resistance patterns by preventing unnecessary over-prescribing of medications. In any clinical setting, it is advantageous for the clinician to be familiar with this technique to effectively address the conditions of their patients who are refractory to treatment or develop SSNHL.[21]
Enhancing Healthcare Team Outcomes
Performing tympanocentesis can be challenging for many clinicians, particularly as the widespread availability of antibiotics coupled with widely accepted guidelines for their use has obviated the need for the procedure in many settings. However, tympanocentesis still holds a place in modern medical practice, and familiarity with it can provide the astute clinician with an additional tool to treat select patients.[22]
Tympanocentesis is typically carried out by pediatricians, otolaryngologists, and family physicians based on their expertise and skills. Once mastered, the procedure is easily performed and is relatively safe, simple, and effective, with a low complication rate and few contraindications. An interprofessional team approach involving primary care clinicians and otolaryngologists offers the best patient outcomes by reducing the prescription of unnecessary antibiotics and providing relief for patients experiencing severe pain.[18]
Pediatric infectious disease experts currently advocate for tympanocentesis when dealing with refractory otitis media. Furthermore, tympanocentesis is firmly established as a method for intratympanic medication administration for various conditions.[18]