Introduction
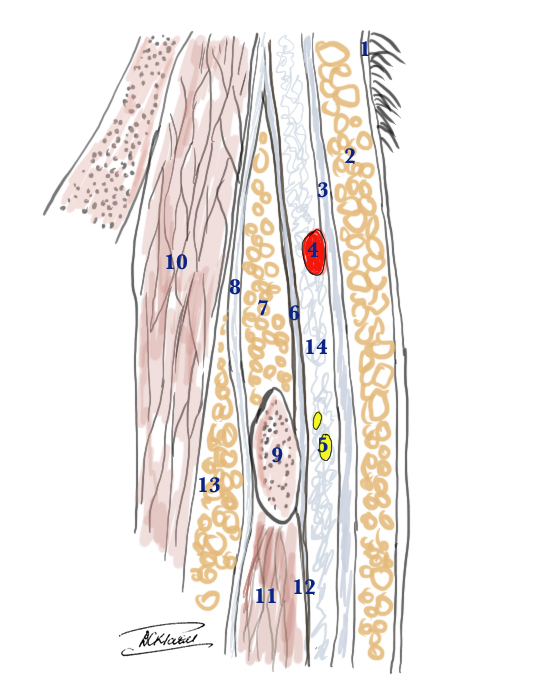
The temporoparietal fascia (TPF) lies under the skin and subcutaneous tissue over the temporal fossa. It is also known as the superficial temporal fascia. It is continuous with the superficial musculoaponeurotic system that is inferior to the zygomatic arch. These two structures are continuous with the platysma muscle in the neck, creating a unified fascia layer from the scalp to the clavicle. The temporoparietal fascia joins the orbicularis oculi and frontalis muscles anteriorly and the occipitalis muscle posteriorly.[1][2][3] It is approximately 2 to 3 mm thick. The layers from the skin to the cranium from superficial to deep in this region are as follows:
- Skin
- Subcutaneous tissue
- Temporoparietal fascia (superficial temporal fascia)
- Innominate fascia
- Deep temporal fascia (divides into a deep and superficial layer)
- Temporalis muscle
- Pericranium
- Cranium
The deep temporal fascia splits into a deep and superficial layer before it inserts into the superior aspect of the zygomatic arch. The superficial temporal fat pad divides these two layers. A proper understanding of the anatomy surrounding the temporoparietal fascia is essential for surgical considerations as it can serve as donor tissue for reconstruction. Additionally, a thorough knowledge of the temporoparietal fascia's relation to surrounding neurovascular structures is integral to safe surgical dissections in this area.