Introduction
The perineum is a diamond-shaped space below the pelvic diaphragm and refers to the lowest region of the trunk. An imaginary line between the anterior ends of the ischial tuberosity divides the perineum into 2 triangular divisions. The anterior smaller triangle is known as the urogenital triangle, and the posterior larger division is called the anal triangle of the perineum. The urinogenital triangle is further divided by a quadrangular fascial layer called the perineal membrane into a deep perineal pouch above the perineal membrane and a superficial perineal space below the membrane.[1]
The superficial perineal space contains the erectile tissues, skeletal muscles, and the terminal branches of the internal pudendal vessels and nerves. Knowledge of the anatomy of the perineum is necessary to provide the best surgical outcomes in cases related to trauma, cancer-related extirpation, and congenital abnormalities.
Structure and Function
The perineum is a diamond-shaped region below the pelvic floor; it extends between the inferior facial layer of the pelvic diaphragm and the perineal skin, which is continuous with the skin over the lower abdominal wall and the medial aspect of the thigh. The surface projection of the perineum is best visualized in the lithotomy position, with the individual lying in a supine position and the hip joints in partial flexion and abduction. It is bounded by the lower border of the pubic symphysis and the arcuate ligament anteriorly, the tip of the coccyx posteriorly, the ischiopubic ramus, and the ischial tuberosities anterolaterally and the sacrotuberous ligaments posterolaterally. An imaginary transverse line (the inter-ischial line) between the anterior ends of the ischial tuberosity divides the perineum into an anterior urogenital triangle and a posterior anal triangle.
The urogenital triangle is the anterior region of the perineum. It is bounded by the pubic symphysis anteriorly, the inter-ischial line posteriorly, and the lower margins of the ischiopubic ramus on each side. The perineal membrane, also called the inferior fascia of the urogenital diaphragm, divides the urogenital triangle into the deep perineal space (above the membrane) and the superficial perineal space (below the membrane). The perineal membrane is attached to the inferior surface of the ischio-pubic ramus on each side. It extends posteriorly to attach to the perineal body and becomes continuous with the superior fascia of the urogenital diaphragm. The perineal membrane is thickened at its apical end to form the transverse perineal ligament.[2]
The superficial perineal space is further divided into the subcutaneous and superficial perineal pouch by the 3 fascia layers: the superficial fascia of the perineum, the deep perineal fascia, and the perineal membrane. The superficial perineal fascia is attached to the margins of the ischiopubic rami at its lateral end and the posterior margin of the perineal membrane at its posterior end. At its anterior end, the fascia continues to line the skin of the urogenital triangle. In males, the fascia also lines the skin of the scrotum that contains the dartos muscle. In both sexes, the fascia becomes continuous with the membranous layer of the superficial fascia of the anterior abdominal wall (also called the Scarpa's fascia). The deep perineal fascia firmly overlies the muscles of the superficial perineal pouch. It attaches to the perineal membrane and the perineal body posteriorly, the suspensory ligament of the penis or the clitoris anteriorly, and the ischiopubic rami laterally.[3]
The subcutaneous perineal pouch is limited by the superficial fascia of the perineum (also called the Colles' fascia) and the deep perineal fascia internally. It contains a thin layer of subcutaneous tissue, which provides mobility to the skin over the external genitalia.
The superficial perineal pouch is contained between the perineal membrane and the deep perineal fascia. The inner surface of the ischiopubic ramus on each side bounds it. It communicates anteriorly with the potential space between the Scarpa's fascia and the fascia of the abdominal wall muscles. The general organization of this region remains the same in both sexes; however, a significant amount of dimorphism occurs in the contents of this area. Although they have different functions in males and females, the ischiocavernosus, bulbospongiosus, and transverse perineal muscle are present in the superficial perineal space in both sexes, along with the branches of the internal pudendal vessels and nerves.
In males, the superficial perineal pouch contains a pair of erectile bodies called the corpora cavernosum of the penis. Posteriorly the paired cavernosum divide to form the crura of the penis that is attached to the ischiopubic ramus. Nestled on the ventral surface of these tissues lies a midline structure called the corpus spongiosum of the penis. It is attached to the perineal membrane at its base and expands to form the glans penis at its proximal, which serves to cap the cavernosal tissue. Each of these erectile tissues contains a core of expandable vascular tissue that engorges with blood to generate effective tumescence for vaginal penetration. In addition to the vascular tissues, the corpus spongiosum also contains the spongy urethra.[4]
A bi-layered sheath of fibro-elastic tissue called the tunica albuginea surrounds each corpus spongiosum and the corpora cavernosa. Superficial to this sheath lies Buck’s fascia, which aids in the attachment of the erectile bodies to the pelvic bones and the perineal membrane. The bulbospongiosus and the ischiocavernosus muscles lie superficial to Buck’s fascia, overlying the deep perineal fascia.[4]
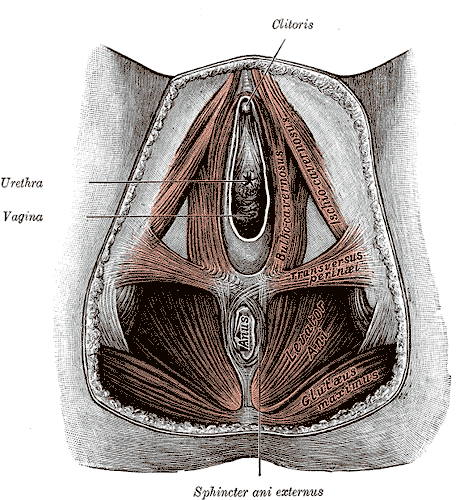
The superficial perineal pouch in females contains a highly neurovascular tissue called the clitoris (see Image. Female Perineum). It contains the female erectile bodies, which include a pair of vestibular bulbs and a pair of corpora that are continuous with the crura. The midline structure of the clitoris, also called the glans clitoris, is a non-erectile body and is only an external manifestation of the clitoris. The deep and suspensory ligaments of the clitoris provide clitoral stability during sexual intercourse.[5][6]
In addition to the erectile tissues, the superficial perineal pouch in females also contains a pair of pea-sized glands called the Bartholin’s gland or the greater vestibular glands. They are located on each side of the vaginal ostium and open via a small duct in the groove between the labia minora and hymen. Its secretions help in the lubrication of the vagina and the vestibule.[7]
Embryology
In males, the corpora cavernosa, corpus spongiosum, and the glans penis develop from the mesoderm of the genital tubercule under the influence of dihydrotestosterone. The penile urethra is formed from the tubularization of the endoderm.[8]
In females, the genital tubercle differentiates to form the clitoris and the bulbs of the vestibule. The Bartholin’s gland is a derivative of the urogenital sinus.[9]
Blood Supply and Lymphatics
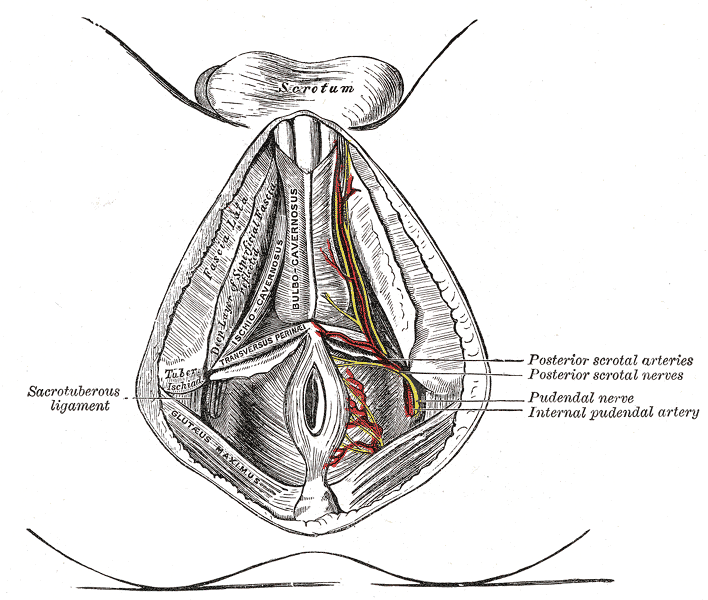
The perineum receives its blood supply primarily from the internal pudendal artery, a terminal branch of the anterior division of the internal iliac artery. It runs anterior to the pyriformis and sacral plexus along the lateral pelvic wall. It exits the pelvic cavity via the greater sciatic foramen and courses around the ischial spine lateral to the nerves. It traverses through the Alcock's canal (pudendal canal) along the lateral wall of the ischiorectal fossa before entering the perineum via the lesser sciatic foramen.[10][11] The branches of the internal pudendal artery supplying the contents of the superficial perineal space include the perineal artery and the terminal branches of the internal pudendal arteries.
The perineal artery originates from the internal pudendal artery in the distal part of the pudendal canal and supplies the muscles of the superficial perineal pouch. It also gives rise to the posterior labial artery, which supplies the skin of the labia majora and labia minora in females, and the posterior scrotal artery, which supplies the skin of the scrotum in males. The deep artery of the penis or clitoris originates from the internal pudendal artery in the deep perineal space, passes through the perineal membrane, and runs between the corpus cavernosa of the penis/clitoris and supplies these structures. The artery of the bulb of the penis, a branch of the internal pudendal artery, supplies the bulbourethral glands. Then it passes through the perineal membrane to supply the corpus spongiosum of the penis. In females, the artery to the bulb of the vestibule supplies the vestibular bulbs and the related areas of the vagina. The terminal branch of the internal pudendal artery: the dorsal artery of the penis/clitoris, runs between the perineal membrane and pubic symphysis and supplies the corpus spongiosum and the glans of the penis in males and the glans and prepuce of the clitoris in females.[1]
Venous drainage to the superficial perineal space is derived from the internal pudendal vein, formed from the venae comitantes of the internal pudendal vein, which unite to drain as a single vessel into the internal iliac vein. The lymphatics from the skin over the external genitalia drain into the superficial inguinal lymph nodes, and the glans, corpus spongiosum, and corpora cavernosa drain to the deep inguinal lymph nodes and external iliac lymph nodes.[1]
Nerves
The pudendal nerves supply the major cutaneous and motor innervation to the structures in the perineum. It is formed from the anterior division of the anterior rami of the second, third, and fourth sacral spinal nerve of the sacral plexus. The pudendal nerve leaves the pelvic cavity via the greater sciatic foramen and passes around the sacrospinous ligament to enter the anal triangle via the lesser sciatic foramen. It lies medial to the internal pudendal artery.
The larger terminal branch of the pudendal nerve, the perineal nerve, divides into the muscular branches and the posterior labial or scrotal branches in females and males, respectively. In females, the posterior labial nerve has a medial and lateral branch. It runs along the lateral part of the urethral triangle to supply the skin of the labia majora and sensory innervation to the skin of the lower vagina. In males, the posterior scrotal nerve also has a medial and lateral branch that runs along the urethral triangle's lateral aspect to innervate the scrotum's skin (see Image. Perineal Arteries and Nerves, Male Perineum).
The dorsal nerve of the penis and clitoris originates in the deep perineal pouch and penetrates the perineal membrane to supply sensory innervation to the penis and clitoris.[12][13] Muscular branches of the perineal nerve supply the bulbospongiosus, ischiocavernosus, and the superficial transverse perineal muscles. A nerve to the bulb of the urethra supplies the corpus spongiosum of the penis in males and terminates in the urethral mucosa.
Muscles
The superficial perineal space contains 3 pairs of muscles within the superficial perineal pouch. These include the following:
Ischiocavernosus
The ischiocavernosus is a paired muscle covering the crus penis in males and the crus clitoris in females. It originates from the ischial tuberosity and the ischiopubic ramus and forms the lateral boundary of the perineum. It attaches to the under-surface of the crus clitoris and the crus penis. It is innervated by the deep branch of the perineal nerve and receives its arterial supply from the perineal artery, a branch of the internal pudendal artery. Contraction of the ischiocavernosus muscle pushes the blood away from the roots of the erectile tissue and also leads to the compression of the surrounding veins, preventing venous return. This helps in maintaining the turgidity of the penis and the clitoris during erection.[14]
Bulbospongiosus
The bulbospongiosus covers the bulb of the penis in males and encircles the vaginal orifice in females. It is a bipennate muscle with different origins and insertions in the 2 sexes. In females, it originates from the perineal body and is inserted into the dorsal surface of the corpora cavernosa of the clitoris.
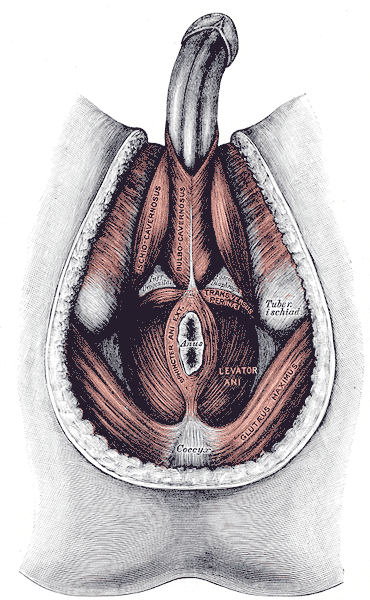
In males, the muscle originates from the median raphe and the perineal body and divides into 3 fibers: the anterior fibers that radiate to encircle the corpus cavernosum, the middle fibers encircle the bulb of the penis and the corpus spongiosum, the posterior fibers attached to the perineal membrane (see Image. Muscles of the Male Perineum). It is innervated by the deep branch of the perineal nerve and receives its blood supply from the perineal artery a branch of the internal pudendal artery. In males, the compression of the bulbospongiosus aids in emptying the penile urethra during urination and ejaculation. In both sexes, the contraction of the muscle aids in the process of erection by forcing blood from the corpus spongiosum in males and the bulb of the vestibule in females to more distal structures.[15]
Superficial Transverse Perineal Muscle
The superficial transverse perineal muscle is a transverse strip of muscle that runs across the superficial perineal space anterior to the anus. It originates from the anterior and medial aspect of the ischial tuberosity and inserts at the perineal body. The deep branch of the perineal nerve also innervates it.
Surgical Considerations
Due to the clearly defined anatomy of the fascial compartments of the male perineum, several clinical presentations are identifiable. In case of a traumatic injury to the penile urethra or penile fracture, if the Buck’s fascia remains intact, the extravasated blood is confined within the penile shaft, resulting in ecchymoses commonly described as an eggplant deformity. Traumatic rupture, secondary to straddle injuries that lead to the rupture of Buck’s fascia and the deep perineal fascia, can cause the urine and blood to leak into the subcutaneous perineal pouch. The resulting hematoma and urine spread into the scrotum and the anterior wall, but it is limited halfway between the pubic symphysis and the umbilicus due to the membranous layer of the superficial fascia of the anterior abdominal wall. The posterior spread is limited by the attachment of the Colles' fascia to the perineal body.[4]
The same anatomic pathways account for the progression of necrotizing fascitis - Fournier gangrene within the perineal region. Buck's fascia and Colles' fascia limit the fasciitis progression beyond and beneath their attachments, secondary to the obliterative endarteritis of the arteries supplying the region due to endotoxemia. The treatment of a case of Fournier’s gangrene is a surgical emergency and requires urgent surgical excision of the dead and infected tissue.[16][17]
Clinical Significance
The tunica albuginea, a fibro-elastic connective tissue surrounding each corpus cavernosum and the corpus spongiosum, facilitates penile rigidity during erection. Peyronies disease can lead to the development of plaques in this layer and disrupt the natural ability of tunica albuginea to perform its function.[18]
The Bartholin glands in females are within the superficial perineal space. These glands secrete a fluid that lubricates the vagina. The Bartholin glands are not visible in normal circumstances, but if the glands are blocked, they can swell and present as a fluid-filled cyst. If the fluid gets infected, a condition known as bartholinitis occurs, which can lead to an abscess. The diagnosis requires a pelvic exam, and the treatment is incision and drainage with marsupialization. Unfortunately, a simple incision and drainage are associated with recurrences.[19][20]