Introduction
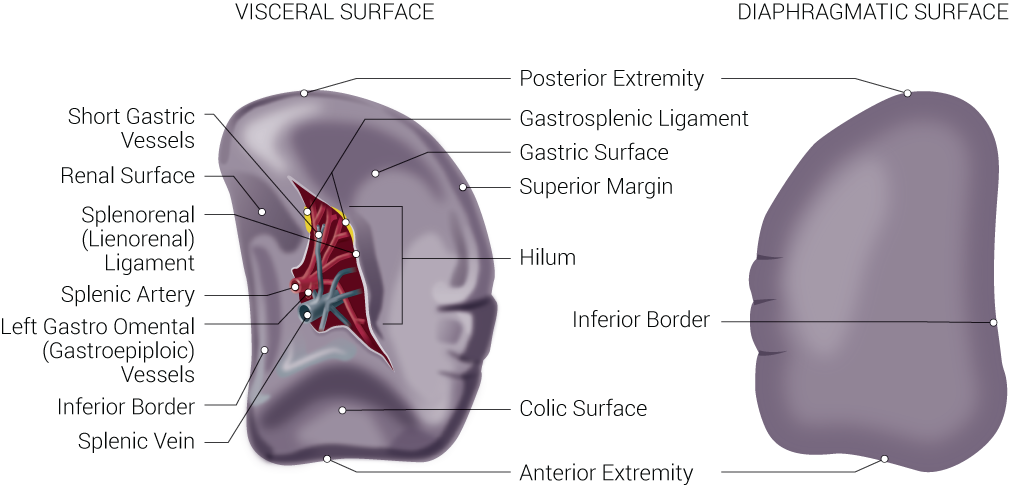
The spleen is the largest organ of the lymphatic system positioned between the fundus of the stomach and the diaphragm in the left hypochondriac region of the abdominal cavity, relatively below the left costal margin between the ninth and 11th ribs. The spleen is spongy and appears reddish purple on account of it being densely vascularized. A healthy spleen is usually not palpable in most individuals. It is encased in a weak outer connective tissue capsule which allows for protection and also the expansion of the organ and is subdivided into many smaller internal sections termed lobules. The spleen has an anterior and posterior segment and rests on the upper pole of the left kidney and tail of the pancreas. The spleen has 3 distinct borders: superior, inferior, and intermediate. The superior border of the spleen has a notch on the anterior end. The spleen has 2 surfaces, the visceral and diaphragmatic. The latter surface is convex and smooth, whereas the former surface is concave and irregular with several imprints. The most concave imprint on the spleen is a resultant of the fundus of the stomach. The left kidney leaves an imprint on the intermediate and inferior borders. The colic imprint is from the splenic flexure of the colon. The tail of the pancreas leaves an impression between the hilum and colic impression sites. The splenic hilum is found on the inferomedial aspect of the gastric imprint. The splenic hilum contains nerves, splenic vessels, and also contains attachments for the splenorenal and gastrosplenic ligaments. It is roughly the size of an individual’s fist, measuring about 10 cm to 12 cm (about 3.94 to 4.72 in) and weighing about 150 g to 200 g (about 5.29 oz to 7.05 oz).[1][2]
Structure and Function
The spleen has several functions, including the filtering of blood, removing microbes and inadequate red blood cells (RBCs), producing white blood cells (WBCs), and antibody synthesis. It is important to note, that while the spleen does have a wide range of functions, it is not a vital organ. Individuals can survive without a spleen as other organs of the body, such as the liver, can adapt in its absence to serve just about the same functions. The spleen consists of 2 different tissue types, termed white pulp and red pulp, with each tissue type serving unique functions. White pulp is composed of periarteriolar lymphoid sheaths (PALS) and lymphatic nodules. The white pulp tissue is involved with the production and maturity of WBCs, particularly lymphocytes (types B and T) and thereby the production of antibodies. The red pulp is composed of splenic sinusoids (wide blood vessels) and cords/threads of connective tissue. The red pulp tissue is involved more so with the filtering aspect of the blood. The red pulp removes old, damaged, and/or useless red blood cells. Contained within the red pulp are also WBCs, particularly phagocytes (macrophages in particular) which destroy microorganisms such as viruses, bacteria, and fungi. The red pulp also acts as a storage area for WBCs and platelets, which are typically released to injury sites to aid in healing and inflammation regulation or to assist in blood loss compensation. The white and red pulp regions are separated by a border known as the marginal zone which functions as a filter, filtering pathogens out of the blood and into the white pulp. [3]
Embryology
Mesenchymal cells are the source from which the spleen is derived from, which are located between the tiers of the dorsal mesogastrium as early as the fifth and sixth weeks of fetal development. The characteristic shape of the spleen is something which occurs early in the fetal period. The rotation of the stomach during embryonic development causes the left mesogastrium surface fusion with the peritoneum above the left kidney and the resultant dorsal attachment of the lienorenal ligament. The yolk sac wall and near dorsal aorta are the sources of the cells needed for the hemopoietic function of the spleen. By the second trimester, the spleen is capable of both RBC and WBC generation.
Blood Supply and Lymphatics
As previously mentioned, the spleen is an organ of high vascularity. The splenic artery primarily supplies the organ arterially, entering the splenic hilum near the middle of the visceral surface. The splenic artery branches off of the celiac trunk and runs within the splenorenal ligament, lateral and across the superior pancreatic aspect. Upon approaching the spleen, the splenic artery divides into 5 branches which supply blood to different regions of the organ. The result of this is vascular segmentation of the spleen as the 5 sub-branches do not anastomose. The splenic vein allows for the venous drainage of the spleen. It also runs from the hilum and runs posteriorly to the pancreas and later joins with the superior mesenteric vein to constitute the portal vein. The spleen is a major organ of the lymphatic system, and as such contains lymphatic vessels not necessarily in proper splenic tissue, but rather some arisen from the capsule region. However, the lymphatic vessels of the spleen are solely efferent lymphatic vessels, with the spleen acting analogously to a large lymph node supplying lymph material to neighboring nodes such as the pancreaticosplenic lymph nodes.
Nerves
Sympathetic innervation of the spleen comes from the celiac plexus. Parasympathetic innervation comes from the vagus nerve (CN X).
Physiologic Variants
There are not many natural physiological variations in spleens. Some common variations which do exist naturally are in relation to organ size, with differences being minimal. Nevertheless, congenital abnormalities of the spleen do exist and include, but are not limited to, the following:
- Shape (lobulations, notches, and clefts)
- Accessory spleen
- Wandering/displaced spleen
- Polysplenia (Chaudhry's disease)
Surgical Considerations
Surgery of the spleen is not uncommon and is typically required for any traumatic event to the spleen which causes bleeding. Splenic rupture and/or lacerations may lead to life-threatening internal bleeding warranting a splenectomy. Partial splenectomy may also be considered based on the vascular segmentation of the spleen via the un-anastomosed arterial supply. A splenectomy may be performed via laparoscopy or laparotomy. Whenever possible, laparoscopy is recommended as it typically results in less scarring and faster recovery time for the patient as a less invasive approach compared to laparotomy. Other conditions which may require splenectomy include, but are not limited to hypersplenism (overactive spleen), blood disorders such as idiopathic thrombocytopenia purpura (ITP), thalassemia, hemolytic anemia, sickle cell anemia), and cancer such as lymphoma, Hodgkin disease, and leukemia.[4][5][6]
Clinical Significance
Understanding the spleen and issues related to the spleen is of great clinical significance because despite it not being a vital organ, issues thereof can potentially be life-threatening. Understanding the function of the spleen and how those functions and responsibilities may be taken up by red bone marrow, the liver, and lymph nodes allow for the spleen to be classified as a no-vital organ and treatment decisions can be made on this basis. Such treatments may include repair, partial splenectomy, or even complete splenectomy as previously cited.
The spleen is one of the abdominal organs with the greatest incidence of injury, with rupture being a big concern possibly justifying splenectomy to avoid excessive hemorrhaging into the peritoneal cavity. A rupture is characterized by a break of the capsule encasing the spleen and disruption of the parenchyma beneath. Such rupture may be caused by blunt force or penetrating trauma. It is also important to note that splenic rupture should be watched for in the presence of left rib fractures as it is not uncommon for a rib bone fragment to puncture the spleen.
The spleen may also become enlarged (splenomegaly) for a variety of reasons. Some of these reasons include viral or bacterial infection, vein blockages and related increased venous pressure, cancer, and circulations issues relate to abnormal cells. Splenic enlargement poses a risk for splenic rupture which may warrant surgical removal. An enlarged spleen may be palpable allowing for detection upon physical examination and may be further evaluated via radiographic imaging studies.
It is also important to note the clinical significance of spleen removal when discussing splenic injury and justification of removal. With the absence of a spleen, individuals lose some of their immunological potentials, resulting in the lesser potential to combat disease and infection. Those without a spleen are also more susceptible to specific infections including those brought upon by Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Thus, it is recommended that patients who have a surgical history of splenectomy be vaccinated accordingly to reduce vulnerability. Sickle cell disease also may warrant the use of immunizations and vaccinations to aid the immunological response that may be impaired by the abnormal interaction the irregular cells may have in the spleen thereby preventing optimal splenic function.