Continuing Education Activity
Sigmoid volvulus is the most common type of colonic volvulus and occurs when a portion of the intestine twists around its blood supply. In sigmoid volvulus, this occurs at the base of the mesentery. It most commonly presents in patients who are bedbound and have a history of chronic constipation. Patients may demonstrate a loss of appetite, diminished or absent bowel output, and worsening abdominal distension. This activity outlines the evaluation and treatment of sigmoid volvulus and describes the role of the interprofessional team in improving care for patients with this condition.
Objectives:
- Review the typical presentation of a patient with sigmoid volvulus.
- Identify the testing that should be done if sigmoid volvulus is suspected.
- Explain the management strategies for sigmoid volvulus .
- Summarize the importance of cooperation among the interprofessional team to recognize the typical presentations of sigmoid volvulus and provide prompt decompression, which will improve outcomes.
Introduction
A volvulus is a twist of the intestine around the axis of its blood supply. In the case of a sigmoid volvulus, the twist occurs in the sigmoid mesentery at its base. Sigmoid volvulus is the most common type of volvulus of the colon. Less common are caecal volvulus and volvulus of the transverse colon. It presents most commonly in patients who are less mobile, bed bound and institutionalized, usually with a background of chronic constipation.[1][2][3][4][5]
Etiology
In order for a volvulus to occur, the bowel needs to be able to twist around a narrow-based mesentery. This occurs mostly in less mobile patients with a history of chronic constipation, where the sigmoid colon becomes chronically distended and redundant.
Epidemiology
Sigmoid volvulus is more common in Africa, as the food intake is of high fiber and the base of the sigmoid mesentery in the African population is narrow compared with other ethnic groups, leading to an anatomical situation that makes the population more susceptible to developing a sigmoid volvulus.
Pathophysiology
Volvulus is a classical example of a large bowel closed loop obstruction. If inflow and outflow of the colon are both obstructed, the obstructed bowel will continue to distend, due to a large amount of gas forming bacteria trapped inside. This will eventually lead to a perforation of the obstructed segment.
While the colon is obstructed and distending, there is impaired blood supply, leading to ischemia, as well as bacterial translocation of the gut flora. Usually, the venous outflow is compromised first, increasing congestion even further, until arterial supply stops. The colonic mucosa is most susceptible to ischaemic insult, leading to an impaired barrier and translocation of bacteria, until the ischemia affects muscular and serosa, leading to necrosis and perforation.
Sigmoid volvulus can become a recurrent situation, and in those patients treated conservatively, the base of mesentery will eventually become fibrotic and the bowel chronically distended.
History and Physical
Patients presenting with volvulus are usually of an older age group with potential other comorbidities, often have reduced mobility or are bed bound and commonly get referred from residential and nursing homes. A history of chronic constipation is common. The symptoms usually leading to acute hospital admission are a loss of appetite and reduced oral intake, increasing abdominal distension, and cessation of bowel output. Patients complain of discomfort due to the significant distension, but are rarely in pain, unless ischemia and/or a perforation have occurred. They can, however, have respiratory compromise due to the splinting of the diaphragm that is a result of the colonic distension.
Patients may present with sigmoid volvulus as a recurrent problem if they have been treated with conservative measures in the past. A recurrent episode of volvulus needs to be taken a seriously as a first presentation and requires the same attention to history and physical examination as a patient presenting with volvulus for the first time.
Examination of the abdomen reveals significant distension, a generalized tympanitic percussion note and potentially guarding and rebound over areas of ischemia or impending perforation. If a perforation has already occurred, the patient will be grossly peritonitic. Digital rectal examination reveals an empty and often capacious rectum.
Evaluation
The patient should have the standard blood work (full blood count and renal function tests), to aid in resuscitation and assess the kidney function for a potential CT scan with contrast. Plain abdominal radiographs will show the classical coffee bean or kidney bean sign, and often dilatation of the proximal colon. Depending on the duration of symptoms, the proximal colon can decompress into the distal small bowel, as long as the ileocaecal valve is incompetent. CT scan shows the characteristic "whirl" appearance of the twisted mesentery, as well as the distended loop of sigmoid colon with an air-fluid level. Free air on either the abdominal radiograph or the CT scan indicates a more serious bowel perforation and requires immediate action.[6][7][8][9]
A CT scan is recommended to establish the diagnosis and distinguish the etiology from other causes of large bowel obstruction, such as a malignant tumor. This is especially the case if the patients present with symptoms for the first time and have not had any previous colonic investigations such as a colonoscopy.
Treatment / Management
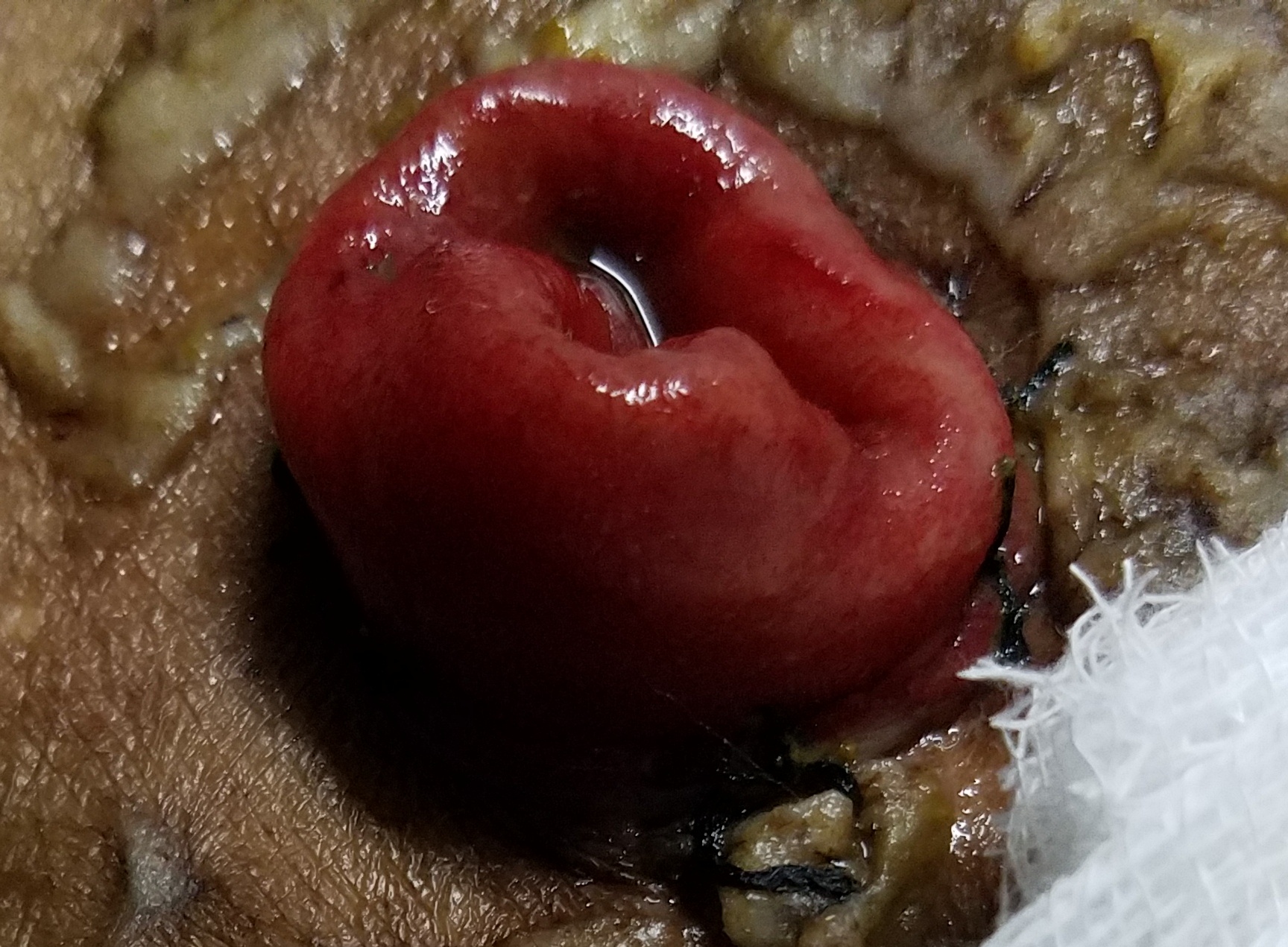
Before any surgical intervention, the patient needs to be adequately resuscitated with intravenous fluids, and electrolyte imbalances should be corrected. A nasogastric tube can aid proximal decompression. Decompression of the sigmoid volvulus should be attempted with a soft rectal flatus tube by the bedside, ideally feeding the tube under direct vision through a rigid sigmoidoscope. Flexible Sigmoidoscopy with gentle insufflation is indicated if the bedside decompression fails or if there are concerns about the viability of the bowel wall, as the mucosa can be inspected during the sigmoidoscopy and areas of mucosal ischemia will become obvious.[10][11][12]
Those patients who cannot be decompressed or who have progressed to compromised viability of the colon will need surgical intervention. The surgery of choice is a sigmoid colectomy with either a primary anastomosis or an end colostomy, depending on findings during the surgery and the individual patients’ physiological reserves.
A patient presenting with bowel perforation will require aggressive resuscitation and an immediate laparotomy to control the fecal contamination and remove the perforated segment of bowel.
Patients presenting with recurrent episodes of sigmoid volvulus that can be decompressed should have an informed discussion about the benefits and risks of an elective resection of the sigmoid to prevent further episodes of volvulus leading to emergency admission to hospital. In the elective situation, a sigmoid colectomy can usually be performed with a primary anastomosis instead of an end colostomy, unless the patient has significant comorbidities.
Differential Diagnosis
- Abdominal Aortic Aneurysm
Pearls and Other Issues
Bedside decompression with a flatus tube should only be carried out by experienced physicians, and under no circumstance against resistance, as there is a risk of inadvertent iatrogenic perforation. The safest method to decompress the sigmoid colon is under direct vision with rigid or flexible sigmoidoscopy.
A successful decompression will immediately result in the evacuation of liquid and gas per rectum with subsequent resolution of the abdominal distension, resulting in a soft abdomen.
This resolution can be documented on a repeat abdominal radiograph.
It is important to assess the patient for sustained resolution once the flatus tube has been removed and the patient is started on oral intake, to avoid the volvulus recur before the patient is even discharged.
Enhancing Healthcare Team Outcomes
The diagnosis and management of sigmoid volvulus is with an interprofessional team that consists of a surgeon gastroenterologist, primary care provider, nurse practitioner, and an internist. The initial treatment is decompression with a flexible endoscope but because of recurrence, surgery is recommended. Most of the patients are old and frail with several comorbidities. Hence, great caution should be used in recommending aggressive treatments. The outcomes for healthy patients after surgery are excellent. [13][14](Level V)