Introduction
Arterial lines placement is for real-time monitoring of blood pressures and arterial blood sampling in critically ill patients or those undergoing complex procedures and surgeries. Anesthesiologists, emergency physicians, and intensivists perform the procedure, and increased use of ultrasound has reduced its difficulty. The radial artery is a common site for placement; however, it can be placed in other large arteries most commonly the femoral artery. This article will discuss the indications, contraindications, materials needed, setup, and the procedure itself.[1]
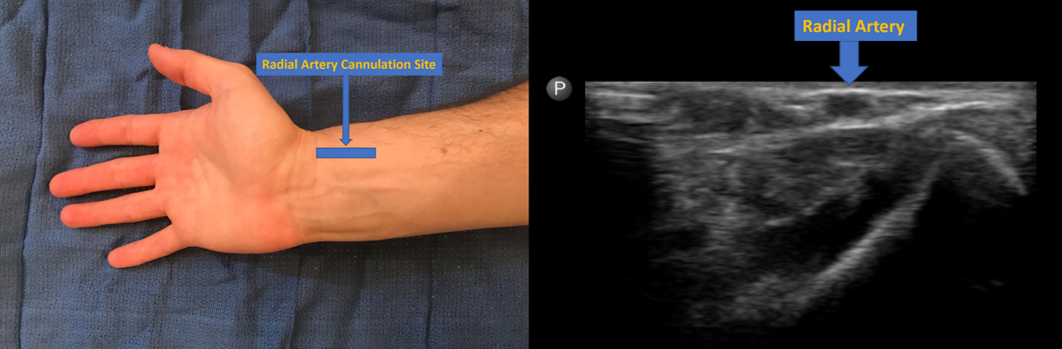
Anatomy and Physiology
The radial artery is a major artery in the forearm. It is a superficial vessel that runs along the lateral, volar aspect of the forearm. It originates in the antecubital fossa as the brachial artery bifurcates into the radial and ulnar arteries. It perfuses the forearm and hand in conjunction with the ulnar artery. It traverses through the forearm, through the anatomic snuff box and terminates in the hand where it transitions into the deep palmar arch. It is extremely superficial at the distal radius which provides access for palpation of a pulse, drawing an arterial blood gas (ABG), and placement of the arterial line.[2]
Indications
Indications for placement of a radial arterial catheter include[3]:
- Real-time, dynamic monitoring of blood pressure in critically ill patients including those experiencing shock, hypertensive emergency, stroke, patients on titratable vasoactive medications, and those undergoing complex surgical procedures.
- Access for frequent blood draws including ABG’s in ventilated patients.
- Monitoring cardiac function in conjunction with separate technologies (i.e., pulse pressure variation).
Contraindications
Contraindications for placement of a radial artery catheter include[4][5]:
Absolute:
- Patient refusal
- Infection overlying the site
- Absent pulse/poor circulation assessed by the Allen test. Positive Allen test which assesses proper collateral perfusion from the ulnar artery. This test is performed by having the patient make a tight fist. The examiner then occludes the radial and ulnar arteries at the wrist, and the patient is asked to relax. The hand should reveal pallor at this point. The examiner then releases the ulnar artery, and the patient should have a return of blood flow through the hand as evidenced by hyperemia throughout the entire hand within 1 to 5 seconds. In a negative test, this provides the performer evidence that there is less chance of an ischemic event to the palmar arch if the radial artery were to be occluded, transected, or thrombosed due to the collateral circulation from the ulnar artery. A positive test would have the return of blood flow in more than 5 seconds and warrant choice of another site.
Relative:
- Coagulopathy
- Partial/full thickness burn
- Vascular graft in upper extremity
- Raynaud syndrome
- Thromboangitis obliterans
Equipment
The materials needed for proper insertion and use of a Radial Arterial line include[6]:
- Transducer kit with all IV lines, transducer cables, and proper monitor setup.
- Chlorhexidine or any available sterile cleansing solution
- Sterile towels or drapes
- Insertion needle with a guidewire (this will be institution-specific as to which kit/supplies are available)
- Lidocaine with syringe/needle
- Ultrasound with a high-frequency probe(optional)
- Suture material( silk or other nonabsorbable suture)
- Needle driver or sutures on a straight needle
- Gauze
- Tegaderm or other sterile dressing
- Sterile supplies including mask, cap, gown, and gloves (depending on the planned length of placement with arterial lines for surgeries often being placed with only sterile gloves and those that will be indwelling for a longer period placed under maximal barrier precautions)
Personnel
This procedure can be performed solely by the physician or provider. An assistant may be helpful; however, it is not necessary in the majority of cases. The physician or provider should be able to set up the transducer and monitor and be able to perform the procedure without any assistance. The assistant can help with the setup, monitoring the sterile field, and obtaining extra equipment if necessary.
Preparation
To prepare for this procedure, the operator or provider must have proper indications, confirm there are no contraindications, and consent the patient or health care proxy if available. They can then gather materials, confirm that the transducer is ready for when cannulation is obtained, and perform a proper time out. The Allen test can be performed to assure adequate perfusion and collateral circulation (although this is controversial with many providers opting against performance due to lack of evidence).[7] The operator can now position the patient. The patient should be comfortable in bed, forearm parallel with ground supported by a table, arm supinated and wrist dorsiflexed. A roll gauze or towel can be placed under the wrist to get a comfortable extension. The hand can also be taped to the table to maintain the proper position. The operator can then prepare their sterile field and gather appropriate tools. They will then wash their hands and gown and glove in a proper sterile fashion. The insertion site can then be prepped and draped in the usual sterile fashion. The patient is now adequately prepared for the performance of the procedure.
Technique or Treatment
After positioning the patient, timeout performed, and both the patient and operator prepping in a sterile fashion, the procedure can commence. This procedure can either take place with the addition of ultrasound or blind. There are also multiple different kits, some which have separate guidewires and some that have the needle, catheter, and guidewire in one self-contained apparatus. The procedure is similar, either way. Adequate anesthesia involves injecting 1 to 2 ml of lidocaine at the insertion point for adequate anesthesia.[3]
If this procedure is done blind, the non-dominant hand is used to palpate the radial artery 1 to 2cm proximal to the wrist. The needle is then inserted in a proximal direction, at a 30 to 45-degree angle while watching for a blood flash. There should be bright red pulsatile blood returned with the correct vessel. Upon obtaining the flash, advance the needle slightly further. At this point, the clinician can drop the angle to approximately 10 degrees to aid the guidewire entering the vessels. At this point, the wire needs to be placed into the needle/catheter. Either place the separate guidewire into the needle/catheter or slide the wire down the all-inclusive device. It is possible to remove the needle from the catheter, depending upon the device used. There should not be any resistance to the wire. If there is, remove the wire and reposition the needle until the return of pulsatile blood. Once the wire is sufficiently in the vessel, slide the catheter over the wire and into the artery. The guidewire can now be removed from the catheter; however, before this, make sure to occlude the artery proximal to the insertion site to prevent blood loss from the catheter. Confirmation is also necessary that the transducer is set up and the lines are ready to connect to the arterial catheter. Once confirmed and the artery is occluded, remove the wire while still supporting the catheter as to make sure it will not be dislodged. Attach the transducer line to the arterial catheter and release pressure on the artery. The catheter can now be secured to the patient with the silk suture. Sterile dressings are to be placed overtop.
This procedure is also performable under ultrasound guidance, which improves the success rate, especially the first stick success rate. The linear probe can be placed in the longitudinal or transverse plane, whichever is more comfortable for the operator. Once the catheter is visualized entering the artery, the probe is set down, and the remainder of the procedure is the same.
Complications
Complications are similar for all arterial catheter sites with a few exceptions.[8][9]
Site-specific complication of a radial artery catheter is peripheral neuropathy. General complications include:
- Bleeding
- Infection
- Thrombosis
- Pain
- Embolization
- Ischemia
- AV Fistula
Clinical Significance
Arterial lines play an important role in the management of critically ill patients, and radial artery catheters are the most common. Their placement is necessary for any patient in shock requiring vasoactive medications, CVAs where blood pressure titration is needed, and patients in the ICU requiring frequent blood draws for ABGs. These are just a few circumstances where arterial lines are integral to the proper management of these patients.
Enhancing Healthcare Team Outcomes
Radial line cannulation is a simple, straightforward procedure that has become even easier with the widespread use of ultrasound. It is a procedure that should be in the repertoire of any emergency physician, intensivist, or anesthesiologist. ICU nurses perform the monitoring of the radial line and the distal extremity. If ever, the hand becomes cold; the radial line requires removal.