Introduction
Edema refers to excessive fluid accumulation in the interstitial spaces, beneath the skin, or within the body cavities caused by any of the following and producing significant signs and symptoms.[1]
- An imbalance among the "Starling forces."
- Damage/blockage of the draining lymphatic system
The affected body part usually swells if edema is present beneath the skin or produces significant signs and symptoms related to the body cavity involved.
There are several different types of edema, and a few important ones are peripheral edema, pulmonary edema, cerebral edema, macular edema, and lymphedema. The atypical forms are idiopathic edema and hereditary angioneurotic edema.
Pulmonary edema refers to the accumulation of excessive fluid in the alveolar walls and alveolar spaces of the lungs. It can be a life-threatening condition in some patients.[2] Pulmonary edema can be:
- Cardiogenic (disturbed starling forces involving the pulmonary vasculature and interstitium)
- Non-cardiogenic (direct injury/damage to lung parenchyma/vasculature)
Pathophysiology
The cardiogenic form of pulmonary edema (pressure-induced) produces a non-inflammatory type of edema by the disturbance in Starling forces. The pulmonary capillary pressure is 10mm Hg (range: 6 to 13) in normal conditions, but any factor that increases this pressure can cause pulmonary edema.[8] The alveoli are normally kept dry because of the negative pressure in extra-alveolar interstitial spaces, but when there is[9]:
Increased pressure/pooling--> Increased pulmonary venous pressure--> Increased pulmonary capillary pressure--> fluid in interstitial spaces--> Increased pressure in interstitial spaces--> fluid in alveoli (pulmonary edema).
Pulmonary capillary wedge pressure can be measured and graded and will produce different presentations on X-rays.
History and Physical
Patients usually present with shortness of breath, which may be acute in onset (from minutes to hours) or gradual in onset, occurring over hours to days, depending upon the etiology of pulmonary edema.
Acute pulmonary edema will have[11]:
- Excessive shortness of breath worsening on exertion or lying down
- A feeling of the heart sinking and drowning/anxiety worsening on lying down
- Gasping for breath
- Dizziness and excessive sweating
- A cough may be associated with worsening edema
- Blood-tinged/pink-colored frothy sputum in very severe disease
- Chest pain (myocardial infarction and aortic dissection)
- Cold, clammy skin
Chronic pulmonary edema will have the following:
- Shortness of breath on exertion
- Orthopnea
- Paroxysmal nocturnal dyspnea
- Swelling of the body/lower extremities
- Weight gain
- Fatigue
Ortner syndrome, which refers to hoarseness due to compression of recurrent laryngeal nerve because of an enlarged left atrium, may also be occasionally present in some patients.
Physical Examination
On examination, the positive findings include:
Confusion, agitation, and irritability may be present, associated with excessive sweating, cold extremities, upright posture (sitting upright), and cyanosis of the lips.
Usually raised.
Hypertension is more often present, but if hypotension prevails, it is an indicator of severe left ventricular systolic dysfunction, and cardiogenic shock must be ruled out. Cold extremities are a feature of low perfusion and shock.
Tachypnea is usually present, with the patient gasping for breath.
Tachycardia (increased heart/ pulse rate) and associated finding of the cause in the pulse.
Usually co-exists with pulmonary edema in chronic heart failure.
Dyspnea and tachypnea are usually present and may be associated with the use of accessory muscles for respiration. Fine crackles are usually heard at the bases of the lungs bilaterally and progress apically as the edema worsens. Ronchi and wheezing may also be presenting signs.
- Cardiovascular Findings
- Tachycardia and hypotension may be present along with jugular venous distention. Auscultation of the heart helps to differentiate between the various causes of valvular lesions causing pulmonary edema.
- Auscultation typically reveals an S3 gallop in volume overload states, which may be associated with accentuation of the pulmonic component of S2.
- Several different types of murmurs can be heard depending on the cause of the valvular lesion.
- Mitral stenosis produces a low-pitched, rumbling diastolic murmur associated with an opening snap at the apex, which becomes accentuated on expiration and produces loud S1.
- Mitral regurgitation produces a blowing, high-pitched pan-systolic murmur best heard at the apex, radiating to the left axilla and accentuating on expiration, producing soft S1.
- Aortic stenosis produces a harsh crescendo-decrescendo ejection systolic murmur at the aortic area, increasing on expiration, usually radiating towards the right side of the neck.
- Aortic regurgitation produces a high-pitched blowing early diastolic murmur best heard in the aortic area, greatest during expiration.
Tender hepatomegaly may be a feature in cases of right-sided cardiac failure, which may worsen to hepatic fibrosis and hepatic cirrhosis in chronic congestion. Ascites may sometimes be present.
Evaluation
No single definitive test is available for diagnosing pulmonary edema, but clinically, one proceeds from simple to more complex tests while searching for the diagnosis and the associated etiology.
Blood Tests[12]
- CBC (to rule out anemia and sepsis)
- Serum electrolytes (patients on diuretic therapy may have disturbances )
- Pulse oximetry and ABGs (assessing hypoxia and oxygen saturation)
- BNP (brain natriuretic peptide levels: low levels rule out cardiogenic type )
ECG
Used to rule out ischemic changes and rhythm abnormalities.
Radiologic Investigations[13]
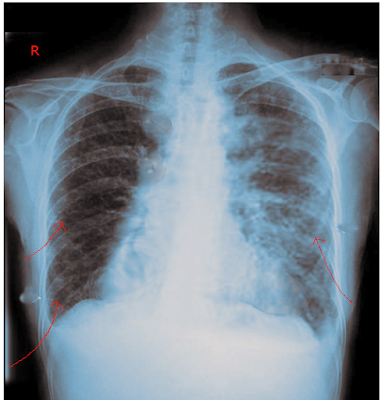
Chest X-ray (It is one of the most important investigations required for the evaluation of pulmonary edema and overload states.
Early Stage
- In the early stages, cardiomegaly is present, usually identified as an increase of cardiothoracic ratio over 50%.
- Broad vascular pedicle
- Vascular redistribution
- Cephalization
Intermediate Stage
- Interstitial edema
- Kerley B lines
- Peribronchial cuffing
- Thickened interlobar fissure
Late Stage
- Alveolar edema
- Perihilar batwing appearance
- Pleural effusion
Ultrasonography
Ultrasonography may be helpful in further strengthening of diagnosis. Transthoracic ultrasound usually differentiates COPD from CCF as a cause of acute exacerbation of chronic dyspnea.
Echocardiography[14]
Extremely important in determining the etiology of cardiogenic pulmonary edema. It differentiates systolic from diastolic dysfunction and valvular lesions.
- Cardiac tamponade
- Acute papillary muscle rupture
- Acute ventricular septal defect
- Valvular lesions
Invasive Technique
Pulmonary Arterial Catheter
A Swan-Ganz catheter is inserted into the peripheral vein and advanced until the branch of the pulmonary artery is reached, and then the pulmonary capillary wedge pressure is measured.
Treatment / Management
General Management[15]
ABC must be addressed initially as the patient arrives.
- Airway assessment ( Make sure the airway is clear for adequate oxygenation and ventilation)
- Breathing ( Note the pattern of breathing and oxygen saturation.)
- Circulation ( Vital signs and cardiac assessment and management )
- Oxygen delivery and ventilatory support (Through nasal cannula, face mask, non-rebreather mask, noninvasive pressure support ventilation, and mechanical ventilation as required)
- Prop up
- Intravenous access
- Urine output monitoring
After initial airway clearance, oxygenation assessment, and maintenance, management mainly depends upon presentation and should be tailored from patient to patient. Supplemental oxygen is a requirement if the patient is at risk of hypoxemia (SPO2 less than 90% ). Unnecessary oxygen should not be administered as it causes vasoconstriction and reduction in cardiac output. Supplemental oxygen, if necessary, should be given in the following order:
Nasal cannula and face mask ---> Non-rebreather mask ---> Trial of non-invasive ventilation (NIV) ---> Intubation and mechanical ventilation
If the respiratory distress and hypoxemia continue on oxygen supplementation, a trial of non-invasive ventilation should follow if there are no contraindications of NIV, as evidence suggests that it lowers the need for intubation and improves respiratory parameters. If the patient does not improve or has contraindications to NIV, then intubation and mechanical ventilation (with high positive end-expiratory pressure) should be considered.
Specific Management[16][17]
- Treatment of the underlying cause.
- Non Invasive Management
- Invasive Management
Non-Invasive Management[18] can be achieved by:
- Pre-Load Reduction which can be achieved by:
- Nitroglycerin
- Sodium nitroprusside
- Isosorbide dinitrate
- Loop diuretics (furosemide, torsemide, bumetanide)
- Morphine and nesiritide require extreme care.
- BIPAP can help move the fluid out of the lungs by increasing the intrapulmonary pressure
After initial resuscitation and management, the mainstay of treatment in acute settings is diuresis with or without vasodilatory therapy. The aggressiveness of treatment depends upon the initial presentation, hemodynamic, and volume status of the patient. VTE prophylaxis is generally indicated in patients admitted with acute heart failure. Sodium restriction is also necessary for patients with HF.
Patients presenting with acute decompensated heart failure (ADHF) with features of pulmonary edema should be treated with intravenous diuretics initially, regardless of the etiology. Patients with HF and features of pulmonary edema receiving treatment with early administration of diuretics had better outcomes according to guidelines of the American College of Cardiology Foundation/ American Heart Association Task Force.[19] A prospective observational study suggested that early treatment with furosemide in patients with AHF lowers in-hospital mortality, and the mortality increases with a delay in the time of administration.[20] Diuretic therapy for patients who have not received diuretics previously is as follows:
If renal function is adequate:
- Furosemide: 20 to 40 mg IV
- Torsemide: 10 to 20 mg IV
- Bumetanide: 1 mg IV
If renal function is deranged/severe HF:
- Furosemide: up to 160 to 200 mg IV bolus, or can be given as 5 to 10mg/hr drip.
- Torsemide: up to 100 to 200 mg IV bolus
- Bumetanide: 4 to 8 mg IV bolus
If the patient shows normal renal function, and there is very little/no response to initial treatment, the dose of diuretics should be doubled at 2-hour intervals until achieving the maximum recommended.
The patients who are on chronic diuretic therapy should receive higher doses of diuretics in acute settings. The initial dose for such patients should be greater than two times of daily maintenance dose. A continuous infusion can also be used as an alternative to bolus therapy if the patient responds to the bolus dose.
While being managed in the hospital for pulmonary edema, IV diuresis can be used using loop diuretics. Furosemide is the usual drug of choice. While diuresis, one should monitor the following:
- Daily weight
- Strict intake and output measures
- Telemetry
- A basic metabolic panel including kidney functions and electrolytes
- Keep serum potassium above 4.0 mEq/L and Mg over 2.0 mEq/L.
- Continuous pulse ox if indicated
- Renal functions
In addition to diuretic therapy, vasodilator therapy may be necessary. Indications include:
- Urgent afterload reduction ( severe hypertension )
- Adjunct to diuretics when the patient doesn't respond to diuretic therapy alone
- For patients with refractory heart failure and decreased cardiac output
Vasodilator therapy has to be used with great caution since it can cause symptomatic hypotension, and the evidence of its efficacy and safety is very limited. When they are needed, they should be used with great caution while monitoring hemodynamic response under expert opinion.
Nitrates (nitroglycerin and isosorbide dinitrate) cause greater venodilation than arterio-dilation and can be used intravenously in recommended doses. Nitroglycerin can be used at 5 to 10 mcg/min initially and can be increased gradually to the maximum recommended dose (200 mcg/min) while closely monitoring the hemodynamic responses. Isosorbide dinitrate has a much longer half-life than nitroglycerin, which puts it at a disadvantage if the drug requires discontinuation because of symptomatic hypotension.
Sodium nitroprusside causes both venous and arterio-dilation and can significantly lower blood pressure. It requires close hemodynamic monitoring through an intra-arterial catheter. It is used initially in a dose of 5 to 10 mcg/min, which can be titrated up to 400 mcg/min, which is the maximum recommended dose. At higher doses, it increases the risk of cyanide toxicity. Hence, it has to be used with extreme caution and with close monitoring under expert supervision.
Nesiritide should not routinely be a therapeutic option for the treatment of HF. A large randomized trial fusing nesiritide in patients of acutely decompensated heart failure (ADHF) shows that it was not associated with any change in the rate of death or rehospitalization, increased risk of hypotension, and a small non-significant change in dyspnea.[21] Nesiritide, if used, should be used initially as an intravenous bolus of 2 mcg/kg and afterward a continuous infusion of 0.01 mcg/kg.
Salt and water restriction is generally indicated for patients with HF.
Vasopressor receptor antagonist (tolvaptan) can also be used with caution and under supervision.
- After-Load Reduction which can be achieved by:
- ACE inhibitors or angiotensin receptor-neprilysin inhibitor (ARNI): captopril, enalapril, lisinopril, perindopril, etc.
- ARBs (angiotensin receptor blockers): valsartan, telmisartan, olmesartan, candesartan, etc.
- Sodium nitroprusside
ACE inhibitors, or ARNI, are the mainstay of chronic treatment for patients with HFrEF. If the patient doesn't tolerate ACE inhibitors or ARNI, then ARB should be considered the first-line choice for prolonged treatment. Beta-blockers and mineralocorticoid receptor antagonists require extra care if used.
If blood pressure is low, start ionotropic agents, and vasopressors (catecholamines and phosphodiesterase inhibitors) should commence. The treatment for heart failure with reduced ejection fraction (HFrEF) differs from heart failure with preserved ejection fraction. (HFpEF).
For patients of HFrEF presenting with hypotension, intense hemodynamic monitoring is necessary. The patient should undergo evaluation for signs of shock (confusion, cold extremities, decreased urine output, etc.). If the patient of HFrEF has signs of hypotension and/or blood pressure less than 80mmg, Ionotropes should be added immediately and titrated accordingly. For patients with persistent shock, vasopressors also have to be added.
For patients with HFpEF, only vasopressors are necessary. Inotropes are NOT indicated in patients with HFpEF and dynamic left ventricular obstruction (most commonly hypertrophic obstructive cardiomyopathy).
Invasive Management[14]
- IABP (intra-aortic balloon pump)
- Ultrafiltration
- Ventricular assist devices
- ECMO (extracorporeal membrane oxygenation)
- Cardiac transplant
- Valve replacement (in case of valvular issues)
- PCI (percutaneous coronary intervention)
- CABG (coronary artery bypass graft)
- Intubation (if required to maintain the airway and also helps in moving the fluid out)
In a patient of severe HFrEF with acute hemodynamic compromise and cardiogenic shock, mechanical cardiac support is available while waiting on a decision or waiting on recovery, hence called " bridge to the decision and "bridge to recovery." The patients usually have blood pressure less than 90mmHg, PCWP greater than 18mmHg, and a cardiac index of less than 2L/min per meter square.
IABP (intra-aortic balloon pump) is the device that is used most commonly among mechanical circulatory devices as it is the least expensive, easily insertable, and readily available. It consists of a balloon in the aorta that inflates and deflates synchronously with the heartbeat, causing increased cardiac output and coronary flow. IABPs are commonly used for temporary circulatory support with patients with advanced heart failure while waiting for a heart transplant or VADs. It is not a definitive therapy but is widely used as a bridge therapy for patients with cardiogenic shock and also as an adjunct to thrombolysis in acute myocardial infarction for stabilization.
Ventricular assist devices, as compared to IABP, have greater efficacy in increasing the hemodynamic parameters. These have more complications and require more expertise, take longer to insert and cost more in comparison. They are an option in acute decompensated heart failure. They can also be useful in complications of acute heart failure like cardiogenic shock, mitral regurgitation, and VSDs. They can be different kinds, like the left ventricle to the aorta, the left atrium to the aorta, the right ventricular assist device, etc.
Ultrafiltration (UF) is the most effective approach for sodium, and water removal effectively improves hemodynamics in patients with heart failure. UF is the process of abstracting plasma water from the whole blood across a hemofilter because of the transmembrane pressure gradient. It is preferred over diuretics because it removes sodium and water more effectively and does not stimulate neurohormonal activation through macula densa. UF is used in patients with HF as it decreases PCWP, restores diuresis, reduces diuretic requirements, corrects hyponatremia, improves cardiac output, and thus improves congestion.[22] In some patients with heart failure, UF was associated with improved cardiac index and oxygenation capacity, decreased PCWP, and less need for inotropes.[23] Several types of UF are isolated, intermittent, and continuous. The continuous type can work in an arterio-venous or veno-venous mode, which is the most common type.
UF can be crucial in patients with heart failure and resistance to diuretic therapy and can serve to optimize the volume status. Many questions regarding UF require examination in further studies, and the evidence does not support its widespread use as a substitute for diuretics.[24]
Enhancing Healthcare Team Outcomes
Pulmonary edema can be a very life-threatening condition, and specialized consultation is a requirement for diagnosis and management. Considering a very high short-term mortality rate, an Interprofessional team approach is recommended in the management of these patients to improve outcomes.
Starting from the diagnosis, etiological factor, and management of the patient, a well-coordinated team needs to work for better patient care involving all the related departments. All the available treatment options need to be discussed to avoid any complications and improve the outcome. The use of non-invasive positive pressure ventilation has a significant benefit in acute cardiogenic pulmonary edema.[26] [Level-2]
While the physician is involved primarily in the management of the patient, consultation is also necessary from a team of specialists involving cardiologists, pulmonologists, and cardiothoracic surgeons. The nurses are also vital members of the interprofessional group, as they will monitor the patient's vital signs and communicate back to the team with results. The nurse practitioner, like the primary care provider, follows these patients in an outpatient setting and should try and reduce the risk factors for ischemic heart disease. Patients should be urged to quit smoking, enroll in cardiac rehabilitation, maintain a healthy body weight, become physically active, and remain compliant with follow-up appointments and medications. A dietary consult should be obtained to educate the patient on a healthy diet and what foods to avoid.
Since most patients with heart failure are no longer able to work, social work assistance is crucial so that the patient can get the much-needed medical support.
The role of pharmacists will be to ensure that the patient is on the right medication and dosage. The radiologist can also play a vital role in determining the cause of dyspnea. A mental health nurse should consult with the patient because depression and anxiety are common morbidities, leading to poor quality of life.
As shown above, cardiogenic pulmonary edema requires an interprofessional team approach, including physicians, specialists, specialty-trained nurses, other ancillary therapists (respiratory, social worker), and pharmacists, all collaborating across disciplines to achieve optimal patient results. [Level V]
If the patient is deemed to be a candidate for a ventricular assist device or heart transplant, the transplant nurse should be involved early in the care. With a shortage of organs, one also has to be realistic with patients.
At the moment, the role of morphine and nesiritide remains questionable and requires further evaluation.[27][28]
Outcomes
Unfortunately, despite optimal treatment, the outcomes for cardiogenic pulmonary edema/heart failure are abysmal. There is no cure for this disorder, and the key is to prevent the condition in the first place.