Introduction
Respiration is a complex process that requires both respiratory mechanics and ventilation/perfusion matching to move air into/out of the lungs and exchanging gases between the air and blood at the level of the alveoli, respectively. If either process is not functioning correctly, respiration may be hindered or fail entirely, ultimately exposing the patient to increased morbidity and mortality. Breathing relies on interactions from central and peripheral nervous systems, with voluntary input via the corticospinal tract and autonomic subcortical input at the level of the pons and medulla within the brainstem via the reticulospinal tract.[1]
The diaphragm relies on respiratory rhythm generating neurons (stimulated by carbon dioxide) that reside within the ventral lateral medulla to send signals to the rostral/caudal premotor neurons of the nucleus ambiguous, which regulate inspiratory/expiratory signals, respectively.[2] These signals then descend through the cervical spinal cord before traversing the grey matter at C3 to C5 and synapsing directly onto motor neurons near the phrenic nucleus.[2] Phrenic afferent signals are also suspected to play a significant role in the physiological modification of diaphragmatic function through monitoring breathing mechanisms, conscious perception of breathing, level of ventilation, and sympathetic outputs.[3]
Although the diaphragm and other primary and accessory muscles of respiration provide much of the force necessary to generate a functional pressure gradient, the larynx operates as the gatekeeper of the airway. Utilizing intricate movements of altering airway diameter, the larynx precisely controls pressure, resistance, and airflow for phonation, respiration, and protection of the tracheobronchial tree from aspiration and particulates. The larynx assists in the modification of normal ventilatory patterns, controlling airflow during the process of phonation.
This article reviews the anatomy of the larynx and cricoarytenoid muscles with the goal of understanding the role of these structures on three primary functions: phonation, respiration, and protection of the airway.
Structure and Function
The airway begins at the nasal and oral vestibules, continuing into the nasopharynx and oropharynx, respectively, transitioning into the laryngopharynx before reaching the larynx. Located at the levels of C3 to C6, the larynx is the most superior section of the lower respiratory tract; existing as a cartilaginous, hollow opening to form a continuous connection between the pharynx and trachea.
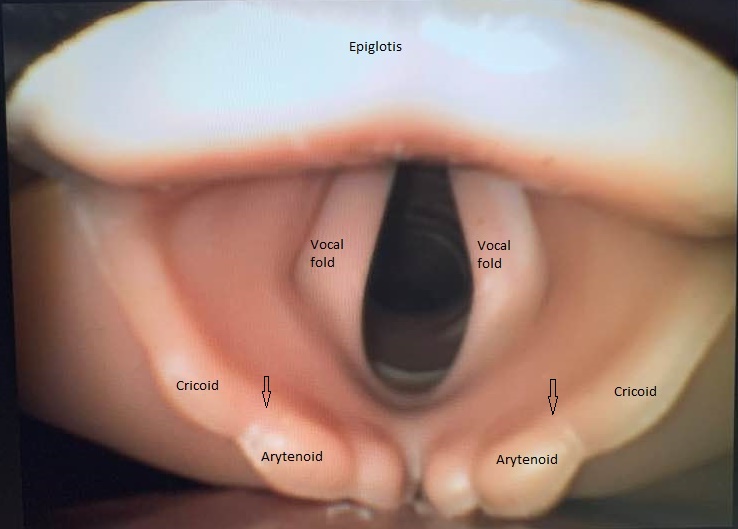
The larynx is a vital structure, providing functions that are often overlooked, despite its multifaceted importance. The larynx functions as a mechanical barrier to protect the lungs from aspiration, vibrates vocal folds to produce sound, fine-tunes ventilation, assists in the cough reflex, and provides a closed valve to facilitate the production of a voluntary Valsalva maneuver. During respiration, the larynx widens the diameter of the airway via abduction of the true vocal folds, exponentially decreasing airway resistance while maximizing flow.
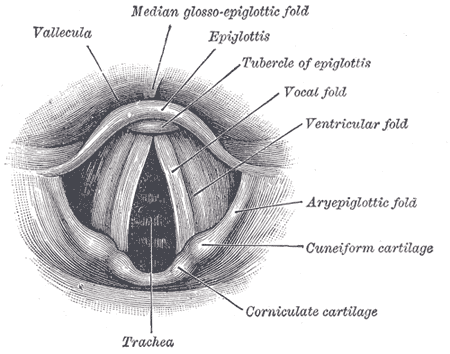
The larynx is sub-divided into three sections: supraglottis, glottis, and subglottis.
The supraglottis comprises the section between the inferior boundary of the hyoid bone, epiglottis, and the vestibular folds, also known as the false vocal cords.
The glottis is the portion of the larynx responsible for phonation; it consists of the true vocal cords, laryngeal ventricle, and the arytenoid cartilages, which adjust the width of the glottis.
The subglottis exists between the inferior boundary of the glottis to the inferior margin of the cricoid cartilage, at which the trachea joins.
Cartilaginous Structures
The larynx comprises of a cartilaginous skeleton conjoined by muscles and ligaments to provide a rigid yet flexible structure. From superior to inferior, the main cartilaginous structures include epiglottis, thyroid cartilage, corniculate cartilage, arytenoid cartilage, and cricoid cartilage.
- Unpaired cartilages: epiglottis, thyroid, cricoid
- Paired cartilages: arytenoid, corniculate, cuneiform
The epiglottis attaches to the larynx inferiorly, angled superior and posteriorly to protect the airway from aspiration during swallowing. During the swallowing reflex, food pushes down the epiglottis, while contracting muscles move the larynx superiorly towards the non-muscular epiglottis, to protect the laryngeal inlet and encourage food particles towards the open esophagus. Although exposed posteriorly, the thyroid cartilage protects the airway externally from anterior trauma; existing as two separate laminae before joining to form the laryngeal prominence, a projection commonly known as Adam’s apple.[4] At the inferior most portion of the thyroid cartilage lies the cricoid cartilage, the only full cartilaginous ring of the airway, creating a fulcrum for the paired arytenoid cartilages and conjoining corniculate cartilages to sit upon posteriorly and trachea to join inferiorly. This relatively loose connection to the cricoid cartilage allows for dynamic motion of the bilaterally symmetrical arytenoid cartilages and their corniculate cartilage horns.
Ligaments and Membranes
The cartilaginous structures of the larynx derive physical support from soft tissue connections in the form of ligaments (folds) and membranes; most easily understood in terms of extrinsic and intrinsic representations. The larynx relies on these fibroelastic tissues to surround its cartilaginous skeleton, to provide support during mechanical movements. The rima glottidis is the potential space between the vocal ligaments contained within these intrinsic ligaments and membranes. Serving as the primary conduit for airflow within the larynx, the rima glottidis may be open or closed secondary to abduction or adduction of the vocal folds, respectively.
Extrinsically, the larynx is bound by the thyrohyoid membrane, hyoepiglottic, and cricotracheal ligaments. Conjoining the anterior aspect of the thyroid cartilage to the hyoid bone superiorly, the thyrohyoid membrane houses the superior laryngeal vessels and nerve, which provides the general somatic afferent signal for the cough reflex.[4] The hyoepiglottic and cricotracheal extrinsic ligaments assist in the stabilization of the larynx, connecting to the hyoid bone superiorly and trachea inferiorly.
Intrinsically, the larynx relies on the quadrangular membrane, cricothyroid ligament for support. The upper and lower portions of the intrinsic laryngeal structures consist of the quadrangular membrane and cricothyroid ligament, respectively. The quadrangular membrane connects each arytenoid cartilage to its respective ipsilateral aspect of the epiglottis, serving as a fibroelastic barrier to prevent the spread of laryngeal cancers.[5] The cricothyroid ligament contains both the cricothyroid membrane and the conus elasticus. The cricothyroid membrane exists as a vertical connection between the cricoid and thyroid cartilages, which thickens anteriorly, creating the median cricothyroid ligament. The conus elasticus, or lateral cricothyroid ligament, is a funnel-shaped collection of elastic tissue, beneath the cricothyroid membrane, running between the thyroid cartilage anteriorly and extending laterally to reach the arytenoid and corniculate cartilage horns posteriorly. The conus elasticus possesses a free upper-edge that is both thickened and horizontally oriented to house the vocal ligament.[6] The curved shape of the conus elasticus is useful in maximizing the efficiency of air flow through the rima glottidis during the production of sound.
The true vocal folds modify the frequency and amplitude of vibrational forces sustained during phonation through rotational and abduction/adduction movements of the arytenoids. At the base of the quadrangular membrane resides a collection of fatty, glandular tissue known as the vestibular (false) vocal folds. Between the true and false folds sits the laryngeal ventricle, a potential space existing as a collapsible outpouching of excess tissue.[4] The aryepiglottic folds run between the arytenoid cartilages and the epiglottis, existing as a ligament of mucosal tissue superior and perpendicular to the vocal folds; housing the cuneiform cartilages and functioning to mechanically protect the airway from aspiration. Lateral to the aryepiglottic folds lies the piriform recess, a section of the larynx often referred to as “no man's land,” secondary to this location’s predisposition to inadvertently catch food particles in elderly patients, ultimately increasing aspiration risk.
Embryology
The larynx is derived from the endoderm and mesoderm. It develops during the fourth week of life. A laryngotracheal groove initially forms from an extension of the foregut, which then becomes an esophagotracheal septum and the laryngotracheal diverticulum. [7]
The third, fourth and sixth pharyngeal arches are the source of many of the muscles of the larynx. The fourth pharyngeal arch forms the constrictors of the pharynx, levator palatini and cricothyroid.[7]
The sixth pharyngeal arch gives rise to the recurrent laryngeal nerve, cricoid cartilage, arytenoid cartilages, corniculate cartilages and the intrinsic musculature of the larynx. [7]
With regards to the intrinsic muscles of the larynx, the recurrent laryngeal brachial of the vagus nerve innervates all muscles, except for the cricothyroid which is innervated by the external branch of the superior laryngeal nerve. This nerve is a derivative of the fourth pharyngeal arch. [6]
Blood Supply and Lymphatics
The larynx receives most of its blood supply via the superior and inferior laryngeal arteries. These arteries exist bilaterally, forming several branches before anastomosing with the contralateral side and opposing artery.
Superior laryngeal artery: originates from the superior thyroid artery branch of the external carotid artery. The superior laryngeal artery travels with the internal branch of the superior laryngeal nerve, piercing the thyrohyoid membranes bilaterally before splitting into several branches. The superior laryngeal artery serves as the main contributor of the larynx, supplying blood to structures located between the peak of the epiglottis to the rima glottidis.
The inferior laryngeal artery branches from the inferior thyroid artery branch of the thyrocervical trunk, which originates from the subclavian artery. The inferior thyroid artery ascends the trachea alongside the recurrent laryngeal nerve, before entering the larynx at the level of cricoid-thyroid cartilage articulation to supply mucosal tissue and laryngeal muscles.
Venous return of the larynx follows paths strikingly parallel to the laryngeal arteries, occurring mostly through the superior and inferior laryngeal branches of the superior and inferior thyroid veins. The internal jugular vein and left brachiocephalic veins serve as the draining vessels for the superior thyroid and inferior thyroid venous tributaries, respectively.
The lymphatic drainage of the larynx is defined into upper and lower categories, utilizing the vocal cords as the landmark differentiator to predict the lymphatic pathways for each structure.[8]
- Above the vocal folds: deep cervical lymph nodes
- Below the vocal folds: pre/paratracheal lymph nodes
Nerves
As the central origin of sensory and motor innervation to the larynx, the vagus nerve (CN X) divides into two primary branches, the superior and inferior (recurrent) laryngeal nerves. The superior laryngeal nerve then splits into two branches; the external branch provides motor innervation to the cricothyroid muscle. While, the internal branch of the superior laryngeal nerve provides sensory afferent signals to the supraglottis and glottis, influencing the cough reflex.[9] All the intrinsic laryngeal muscles, excluding the cricothyroid muscle, receive their motor innervation from the recurrent laryngeal nerve.[10] The recurrent laryngeal nerve also provides motor innervation to the remaining extrinsic laryngeal muscles.[10]
Muscles
Based on innervation, blood supply, and function, the laryngeal muscles separate into specific groups: extrinsic muscles, intrinsic muscles, and cricothyroid muscles. The respective primary actions offered by each of these muscle groups are elevation/depression of the larynx, abduction/adduction of the vocal folds, and stretch/tension of the vocal folds.
Extrinsic Laryngeal muscles, Primary Actions[8]:
- Stylopharyngeus, palatopharyngeal, thyrohyoid m. – elevate the larynx
- Sternohyoid, omohyoid, sternothyroid m. – depress the larynx
The extrinsic laryngeal muscles control the superior and inferior displacement of the larynx, most useful during the phases of swallowing.
Intrinsic Laryngeal Muscles, Primary Actions:
- Posterior cricoarytenoid m. – Abduction of vocal cords, opening of rima glottidis
- Lateral cricoarytenoid, interarytenoid, and thyroarytenoid m. – Adduction of vocal cords, closing of rima glottidis
- Cricothyroid, vocalis m. – tension of the vocal cords
- Thyroepiglottic m. – opening of the laryngeal inlet
- Aryepiglottic, oblique arytenoid m. – closing of the laryngeal inlet
The intrinsic laryngeal muscles are striated muscles that are classified based on action: abduction/adduction of the rima glottidis, tension of the vocal cords, and opening/closing of the laryngeal inlet.[10] The posterior cricoarytenoid muscle is the only abductor of the true vocal cords, opening the rima glottidis via lateral rotation of the arytenoids, maximizing the passage of air during inspiration and expiration.[11] Primarily the lateral cricoarytenoid muscles, but also the interarytenoid and thyroarytenoid muscles, provide the opposing action, closing the rima glottidis via adduction of the true vocal cords and medial rotation of the arytenoids, in order to alter tone/volume of speech or protect the airway.[12] The thyroarytenoid muscle uniquely functions as independent superior and inferior portions, allowing for intricate alterations in sound intensity and quality through relaxation of the vocal ligaments.[12] The distance between the thyroid and cricoid cartilages is narrowed by the cricothyroid, thyroarytenoid, and vocalis muscles, tensing/stretching the true vocal cords foto increasehe pitch of phonation.[12] The vocalis muscle modules the pitch of phonation by simultaneously tensing and relaxing the anterior and posterior aspects of the vocal ligaments, respectively. Vocalis muscles alter the tone of phonation via alterations in the mass of the vocal folds. The diameter of the laryngeal inlet is controlled by the thyroepiglottic, aryepiglottic, and oblique arytenoid muscles; contraction of former muscle causes opening of the inlet, while the latter muscles are responsible for closing the inlet.
Physiologic Variants
One out of 200 individuals, have a non recurrent right inferior laryngeal nerve; instead of the typical course of the recurrent right inferior laryngeal nerve, the variant form branches off the vagus nerve around the level of the cricoid cartilage.[6]
In about 80% of individuals, a connecting branch exists between the inferior laryngeal nerve, a branch of the recuurent laryngeal nerve and the internal laryngeal nerve which is a branch of the superior laryngeal nerve. This is "anastmosis" (although it refers to nerves rather than vessels) is referred to as the anastomosis of Galen and is a very rare one anastomoses between the two nerves. [13]
Surgical Considerations
During both cardiovascular operations, difficult endotracheal intubations and self-extubation by a patient, there is an increased risk for arytenoid cartilage subluxations.[14] In the setting of this type of dislocation, postoperative hoarseness and aspiration may occur secondary to mechanical vocal cord paralysis.[14]
Asphyxiation may occur secondary to immobility of the posterior cricoarytenoid muscles, as the patient will be unable to abduct the vocal cords, preventing them from opening the rima glottidis.[11] This type of injury is possible during thyroidectomy surgery, in which the recurrent laryngeal nerves are susceptible to damage bilaterally, stymying the motor innervation of the posterior cricoarytenoid muscles resulting in neurogenic vocal cord paralysis.[12] Thyroidectomy exposes the external branch of the superior laryngeal nerve to injury, potentially resulting in cricothyroid muscle paralysis and subsequent voice disorders.[15] Intraoperative neuromonitoring may be an effective strategy to alleviate the risk of injury to neurovascular structures during thyroidectomy surgery.[15] Surgical abduction of the arytenoid cartilage has been shown to improve airway function with little secondary impairment of phonation capabilities in patients with bilateral neurogenic laryngeal paralysis.[16]
High-frequency jet ventilation may provide superior hemodynamic stability in comparison to standard endotracheal intubation, specifically during endolaryngeal surgical approaches. Despite the increased frequency of respiratory hazards (such as barotrauma and air entrapment), high-frequency jet ventilation is recommended as the method of airway management during cases involving the posterior aspect of the larynx.[17] This recommendation suggests HFJV improves hemodynamic stability and decreases the likelihood of physically disrupting the desired surgical area, as opposed to convention anesthesia equipment/interventions.[17]
Clinical Significance
If an emergent airway is necessary, an incision is placed through the cricothyroid ligament during a cricothyrotomy. Clinically, the cricoid cartilage serves as a palpable landmark to signify the inferior most portion of the larynx, where the trachea begins; this is vitally important in the circumstance of an emergent airway, in which cricothyroid ligament is incised at the midline between the thyroid and cricoid cartilages.
Under the circumstance of chronic cough in the absence of classical causes, such as chronic bronchitis, there have been suggestions that sensory disturbances of the vagus nerve may be responsible [9]. Hypersensitivity and laryngeal sensory neuropathy may result in a lower sensory threshold for cough reflex activation, resulting in chronic refractory cough (a neurogenic cough). Gabapentin and amitriptyline have been shown to improve these laryngeal hypersensitivities via inhibition of the overactive sensory signals.[9][18]
The 3:3:2 rule can be useful for elective endotracheal intubation where the first "3" is: a measurement of 3 fingers between the upper and lower teeth of the open mouth of a patient indicates the ease of access to the airway through the oral opening. The second "3" is: a measurement of three fingers from the anterior tip of the mandible to the anterior neck provides an estimate of the volume of the submandibular space. The "2" is: a measurement of 2 fingers between the floor of the mandible to the thyroid notch on the anterior neck identifies the location of the larynx relative to the base of the tongue. If its less than two fingers that means the larynx is anteriorly located and in these cases direct laryngoscopy (DL) will be difficult for endotracheal intubation, instead of direct visualization with a bronchoscope or fiberoptics should be attempted.[19]
Cricoarytenoid arthritis (CA) is a feature of rheumatoid arthritis. Symptoms of CA include pharyngeal fullness when swallowing and speaking, hoarseness, and dyspnonea. It can be a cause of recurrent upper airway obstruction in rheumatoid arthritis. On endolaryngoscopy adducted vocal cords are a significant finding. The cricoarytenoid joint can also be affected in dermatomyositis[20]. Thus, pathology of the cricoarytenoid can be a sign of underlying systemic disease.
Other Issues
Disruption of the cervical medullary junction secondary to occipital-cervical instability may result in the inability of voluntary respiration or even complete motor and sensory loss for segments located caudal to the injury [2]. This type of injury may present clinical characteristics ranging from depressed respiratory function to immediate mortality; as such, it is essential to investigate the stability of the cervical spine in those suspected of mechanical injuries.
Similarly, hemisection injuries of the cervical spine, specifically those located rostral to C3 to C5, have been shown to significantly decrease tidal volume with reflexive increased breathing frequency, secondary to ipsilateral hemidiaphragm paralysis.[21]