Continuing Education Activity
Pneumatoceles are air-filled cavitary lesions usually seen in the lung after infection, trauma, or as a part of more extensive cystic disease of the lung. This article will focus on pulmonary pneumatoceles, its etiologies, the underlying pathophysiological processes leading to the formation, clinical presentation, complications, diagnostic imaging, and treatment options. This activity also highlights the role of the interprofessional team in evaluating and treating patients with this condition.
Objectives:
- Identify the etiology of pulmonary pneumatocele.
- Review the appropriate evaluation of pulmonary pneumatocele.
- Outline the management options available for pulmonary pneumatocele.
- Describe interprofessional team strategies for improving care coordination and communication regarding treatment modalities, diagnostic and therapeutic challenges and improve patient outcomes.
Introduction
Pulmonary pneumatoceles also referred to as pseudocysts in the literature, are air-filled thin-walled cysts that are formed in lung interstitium. They can be single but are more often multiple. The term “pseudocyst” signifies a lack of an epithelial lining. Size can vary from greater than 1 cm in diameter to occupying entire hemithorax, with walls less than 4 mm and are of uniform thickness. Pneumatocele may or may not contain air-fluid levels. The lung apices are usually spared, but pneumatocele can occur anywhere in the thoracic cavity. In 1977, Fraser and Pare defined pneumatoceles are air-filled cavity occupying one-third of the lung volume. In trauma, it can be associated with pulmonary contusion, pneumothorax, and pneumomediastinum.
There is no such thing as para mediastinal pneumatocele or gas in the pulmonary ligament. Analysis of 4 case reports showed that it represent medial pneumothorax behind pulmonary ligament or posterior pneumomediastinum.[1][2]
Heamatopneumatocele is characterized by air-fluid levels in post-traumatic settings and contains air and blood.[3][4]
Cervical pneumatoceles are rare but been reported in the literature in infants and could mimic laryngocele resulting in diagnostic challenges.[5]
Desquamative interstitial pneumonia can result in the formation of multiple pulmonary cysts. A resolution of the pneumatocele after treatment with cyclophosphamide is seen in a case report.[6]
Etiology
Pneumatoceles can be formed as a result of either or a combination of the following process.
- Infectious: Tuberculosis, Staphylococcus aureus, Streptococcus pneumoniae, Proteus mirabilis, Escherichia coli, or Acinetobacter calcoaceticus, IV heroin users.[7]
- Noninfectious: Trauma, surgery, mechanical ventilation, hydrocarbon inhalation[7][8], Endobrocheal valve associated pneumatocele[9], kerosine ingestion[10][11], burns [12], persistent interstitial pulmonary emphysema, diffuse interstitial pulmonary emphysema, positive pressure ventilation secondary to a ventilator or continuous positive airway pressure (CPAP).[13][14]
Epidemiology
Pneumatoceles are common among infants, children, adolescents, and immunocompromised individuals, e.g., AIDS
Traumatic pneumatoceles are most often seen in children and young adults. They are rare, developing in less than 3% of patients with pulmonary parenchymal injuries. A tertiary center in Milan, Italy, reported 10 cases over 9 years. Swank and Wolf reported a case of pneumatocele in 1977 in a revolving restaurant.[15] Around 85% of cases involved patients below the age of 30 years. As men are involved more often in motor vehicle accidents and falls, they are affected more than women.[16][17][18][19] Pneumonia complicated with pneumatocele has been reported in 2.4% to 8.3% of all hospitalized children with pneumonia.[20]
The incidence of pneumatoceles was 9.5% in a Brazilian study. The high incidence was attributed to the high level of undernutrition in those children. It was hypothesized that undernutrition delayed development of Kohn’s pores and undernourished children would then have lungs similar to a newborn. When valvular obstruction occurs, air continues to enter with no way out due to the absence of Kohn’s pores, thus forming pneumatocele.[20]
Traumatic pneumatoceles occur primarily in children and young adults. They are usually caused by non-penetrating chest trauma, mostly resulting from car accidents or by continuous positive airway pressure during mechanical ventilation. In literature, 85% of patients were younger than 30 years. Children and adolescents have a more compressible bony thorax than adults, and the elastic recoil of the lungs results in increased negative intrathoracic pressure leading to laceration of lung parenchyma. Only 20% of patients have associated rib fractures. The formed cavities filled with fluid, blood, or air continue to increase in size until a balance of lung pressures is achieved between the cavities and the surrounding tissue.[21][22][14]
A survey result of 10,229 trauma admission showed that 204 children had a pulmonary contusion, 25 of whom (12.3%) were diagnosed with a pneumatocele. Their mean age was 13 years (3 to 17). Seventy-six percent were male. The most common mechanism of injury was a motor vehicle collision (10), followed by falls (6), and sports (5). The pneumatocele was identified on chest CT alone in 15 (60%), on chest CT and chest radiograph in 3 (12%), the upper portions of an abdominal CT in 6 (24%), and chest X-ray alone in 1 (4%). Seven patients were found to have a solitary pneumatocele, and 18 patients had 2 or more. The largest pneumatocele was 3.7 cm in diameter. No child underwent intervention specific to the pneumatocele. Seventeen (68%) patients were seen in follow-up in the clinic from 1 week to 6 months after injury and showed spontaneous resolution.[18]
A case report after treatment of recurrent metastatic cervical cancers with pulmonary metastasis treated with palliative paclitaxel results in the regression of pulmonary nodules and transformation into multiple pneumatoceles.[23]
H7N9 influenza pandemic follow-up study at 12 months in survivors showed that 9.8% (4/41) population develop pneumatocele, which was evident on chest X-ray.[24]
Pathophysiology
After pneumonia, inflammation, and narrowing of the bronchus leads to the formation of an endobronchial ball valve that leads to the distal dilatation of the bronchi and alveoli. The obstruction is believed to be caused by inflammatory exudates within the airway lumen or wall, allowing air to enter the cystic space but not to leave it. Subsequent enlargement of the pneumatocele occurs either due to pressure from the adjacent pneumatocele or intraluminal inflammatory exudates.
After trauma, pseudocysts are produced by shearing forces causing pulmonary laceration accompanied by the escape of air or fluid into the tissue.
Regarding traumatic pneumatocele, the exact mechanism is unknown, but several theories have been proposed.
Some suggest that concussive waves produced by blunt trauma create shearing forces that tear the lung parenchyma. The concussive forces of a high-velocity impact with low displacement of the chest wall result in a peripheral pseudocyst, whereas the compressive forces of a low-velocity impact with high displacement of the chest wall resulting in a central pseudocyst. An intraparenchymal pulmonary laceration with airway disruption and leaking of air into the pulmonary parenchyma occurs in both mechanisms.[25]
Others are of the opinion that traumatic pneumatocele follows sudden, severe compression of a segment of the peripheral bronchial tree, which obstructs the bronchus and transmits an explosive pressure distally. This creates a "bursting lesion."
These theories led to the proposal of a two-step mechanism.
First, compressive traumatic forces increase intrapulmonary pressure until the parenchyma bursts, thus producing lacerations.
Second, decompression of the chest and increased negative intrathoracic pressure allow the elastic tissue of the lung to recoil, permitting the formation of small cavities filled with air or fluid.
Each cavity then continues to grow in size until the pressure within the cavity is equal to that of the surrounding parenchyma.
Following penetrating trauma, "one-way" or "check-valve" mechanism where air enters a laceration in the pulmonary parenchyma, but the defect seals quickly, the air becomes trapped and is unable to escape the pleural space resulting in pneumatocele formation. Continuous positive airway pressure in mechanically ventilated patients is thought to result in pneumatocele formation in a similar way.[14]
Traumatic pneumatocele after a chest injury requires a violent impact directed on a pliable chest wall so that kinetic energy is transmitted to the underlying pulmonary parenchyma. The significance and behavior of the pneumatocele depend on the impact velocity, the degree of chest wall displacement, and the elasticity of the chest wall in blunt chest trauma. It is believed that the more elastic and pliable chest wall of young people and children permits the transmission of kinetic energy more efficiently to the underlying lung parenchyma. The condition is characterized by the appearance of pulmonary cavities with no epithelial lining, filled with air, fluid, or blood, which can be observed on radiological imaging. Pneumothorax or pneumomediastinum might coexist. The presence of a traumatic pneumatocele indicates that tissue disruption is more extensive, and the injury is more severe than a simple contusion.[26][27][16]
It is important to note that the lesion may not be located in the immediate region of chest wall injury. In some cases of traumatic pneumatocele, the traumatic force is transmitted in a contra-coup manner. The velocity of impact and degree of chest wall displacement may also contribute to the location of pneumatocele.
A high-velocity impact produces peripheral alveolar injury while a low velocity, high displacement impact produces central parenchymal injury. All patients with traumatic pneumatoceles involved in a study of high-speed accidents developed pneumatocele lesions peripherally.
In literature, a case of extrathoracic pneumatocele in untreated tuberculosis patients has been described where communication between extrathoracic pneumatocele with the lung parenchyma was thought to be established by an old scar for cold abscess drainage.[28][29][30]
Hydrocarbons induced lung injuries are characterized by rapid progression of respiratory difficulty without causative factors and the presence of ground-glass opacities, spontaneous air leak syndrome resulting in pneumatoceles, and consolidation with later diffuse centrilobular nodular opacity on chest computed tomography (CT).[8]
Hydrocarbons contain polyhexamethylene guanidine (PHMG), oligo (2-[2-ethoxy]ethoxyethyl) guanidinium chloride (PGH), 5-chloro-2-methyl-4-isothiazolin-3-one (CMIT), or 2-methyl-4-isothiazolin-3-one (MIT). PHMG and PGH are commonly thought to caused hydrocarbon associated lung injuries. Animal studies have not established definitive links between exposure to hydrocarbons containing CMIT and/or MIT despite the fact that patients exposed to hydrocarbons containing only CMIT and/or MIT showed clinically similar lung injury to that of hydrocarbons containing PHMG and/or PGH.[31][32]
Persistent interstitial pulmonary emphysema (PIPE) when diffuse can be associated with pneumatocele formation. PIPE is a rare entity that is related to mechanical ventilation-induced lung damage in premature infants with respiratory distress syndrome. Although PIPE localized in one lobe has the potential for curative resection, diffuse PIPE (DPIPE) affecting both lungs carries a poor prognosis.
Kohn's pores theory is explained in a Brazilian study as a cause of pneumatocele formation. It is speculated that undernutrition delayed development of Kohn's pores and undernourished children would then have lungs similar to a newborn when valvular obstruction occurs, air continues to enter with no way out of the segment due to the absence of Kohn's pores; this forms the pneumatocele. Kohn's pores importance in pneumatocele development may account for the scarcity of pneumatoceles in adults where the Kohn's pores are already developed.[25]
Infectious agents associated with pneumatocele formation are as follows:
- Streptococcus pneumoniae[33]
- Staphylococcus aureus, 60% cases result in pneumatocele, more common in children, less common pneumatocele in adults( Egyptian int med) r they related. In an analysis of burns patients, a patient who develops staphylococcal pneumonia develops pneumatocele as well.[34][35] A case report of S. aureus and Candida colonization leading to multiple pneumatoceles is also reported. Pneumatocoeles were identified in 37 out of 100 S. aureus pneumonia cases, patients most of these were only noted on radiographs taken some days after admission
- Pneumocystis carinii in HIV[35][36][37][38]
- Pseudomonas aeruginosa
- Group A streptococci
- Klebsiella pneumoniae[39]
- Adenovirus
- Mycobacterium TB, pneumatoceles can develop during or after treatment of TB[29]
- Proteus mirabilis and ESBL Proteus mirabilis[40][41]
- Ecoli cavitary pneumonia has been associated with the formation of pneumatocele.[42]
- Acinetobacter calcoaceticus[43]
- Hemophilus influenzae B[44]
- Bacteroid species, Peptostreptococcus asaccharolyticus, and Fusobacterium species[45]
Histopathology
Traumatic pneumatocele is a walled-off cavity entrapping air with no proper epithelial lining. A case of pneumonectomy performed for multiple pneumatoceles showed cystic adenomatoid malformation, characterized by the presence of various cysts lined by epithelium in different sizes in a patient with hyper IgE syndrome.[46]
History and Physical
Most traumatic pulmonary pseudocysts present within 24 to 48 hours following blunt chest trauma. The clinical presentation is variable and ranges from asymptomatic to acute respiratory distress requiring ventilatory support.[47]
Patients present with hemoptysis 56% of cases, chest pain, and cough. These symptoms are attributable to the pulmonary parenchymal injury but not to the traumatic pneumatocele itself.
Mild fever or leukocytosis usually occurs 12 to 36 hours after trauma. It occurs as a result of the absorption of damaged lung tissue or blood clots; this should not be misinterpreted as infection.[16]
Toxic shock syndrome toxin associated with staph.aureus can present with rash, fever, chills, mucositis, and result in pneumatocele formation during the disease course.
In traumatic pneumatocele, acute respiratory failure is related to the presence of an associated pulmonary contusion.[48]
Risk factors for developing pneumatocele:
- Young age, in children high risk
- Post-infection
- Post-traumatic
- Post pneumonic[49][20]
- HIV[20][50]
- IV drug use
- Hyper IgE syndrome[50][51]
Evaluation
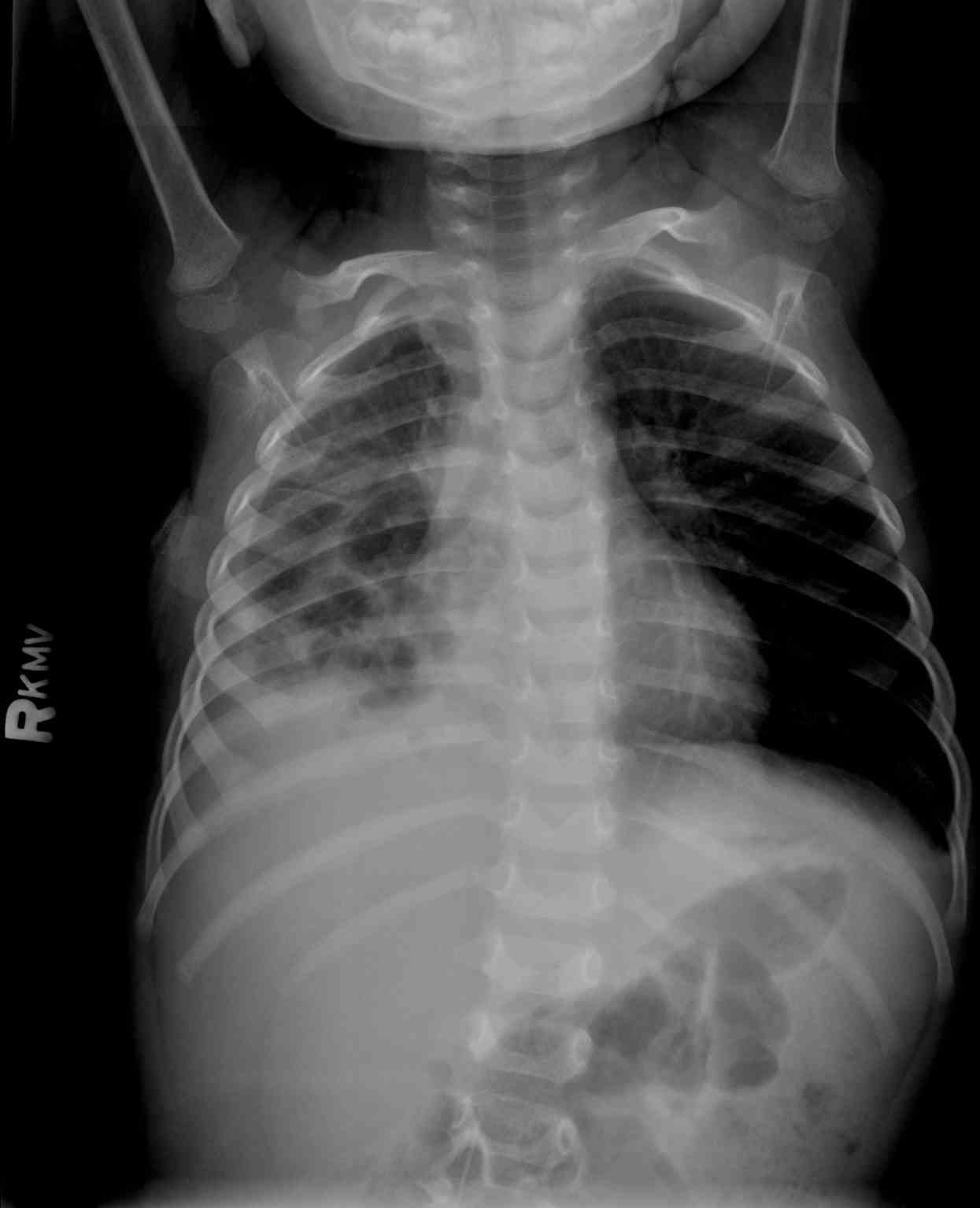
Chest x-ray: in children, 90% are visible on the first chest x-ray after pneumonia. Radiologic evidence, most of the time, occurs on the fifth to the sixth day of hospitalization.
Chest x-ray has a low sensitivity of 24% in diagnosing traumatic pneumatoceles, especially if they are obtained in the supine position and if the lesion is smaller than 2 cm. The diagnostic accuracy of chest radiography ranges from 24% to 50%. Serial chest x-rays taken over several days can be useful to differentiate. The majority of traumatic pneumatocele are found on lower lobes.[16] Only half of the pneumatoceles are detected on radiographs when obtained on the day of injury. Pulmonary contusions can mask the presence for up to 10 days or until the contusion resolves. Despite the yield of false-negative findings, they are still used as the first diagnostic modality in patients with thoracic trauma.[16] The diagnostic utility of chest x-ray improves by post-trauma day five, at which time there is a resolution of the contusion, complete development of the pneumatocele, and a greater possibility of obtaining upright radiographs.
The typical radiographic presentation of traumatic pneumatocele is a round or oval shadow usually surrounded by pulmonary contusion. Air-fluid levels are often present and thought to be related to bleeding into the pneumatocele.
CT scan: CT is much more accurate, with a reported sensitivity of 96%. The thoracic CT scan more precisely defines the location and size of the cyst and provides early detection and differential diagnosis.
In terms of sensitivity evaluated in a study, computed tomography (CT) is superior to radiography in the diagnosis pneumatocele ( 20% vs. 100%).
The main advantages of CT include:
- earlier identification
- visualization of small lesions
- the ability to identify pneumatocele in the presence of pulmonary contusion.
The typical appearance of traumatic pneumatocele on CT is a round or oval thin-walled cavitary lesion with air-fluid levels. More recent studies report an incidence of up to 10%, unlike 3% in comparison to studies prior to 2003. This is attributed to more widespread diagnostic use of CT rather than an increasing occurrence of pneumatoceles.
Lung ultrasound, in combination with chest x-ray, has been found useful in the pediatric population in 2 case reports.
The size of traumatic pseudocysts reported in the literature ranges from 1 to 14 centimeters in diameter Relationships between the size of the lesion and severity of the inciting chest trauma are unclear. Large pseudocysts occurred more frequently in patients with multiple injuries, bilateral pulmonary contusions, or significant respiratory involvement. The risk of developing complications may be higher in patients with large pneumatoceles, posing more risk and complications.[17]
Due to changes in size, shape, and composition of pneumatoceles within days following trauma, serial imaging studies may help differentiate pneumatocele from other lesions.[52]
Treatment / Management
Accurate and early diagnosis is the key to a successful outcome in these patients. The main significance of pneumatocele is that it must be distinguished from other cavitary pulmonary lesions such as abscess, mycosis, malignancy, and others.
Failure to accurately diagnose pulmonary pneumatocele may lead to unnecessary, harmful, and potentially dangerous diagnostic and therapeutic procedures. For example, misidentification of the lesion as a pneumothorax or pneumomediastinum may prompt additional testing or placement of a thoracostomy tube or drainage catheter. Perhaps a more severe error would be confusing an uncomplicated traumatic pneumatocele with a pulmonary abscess. An abscess requires direct intervention, while a true pneumatocele does not. Instrumenting an uncomplicated pneumatocele could potentially seed the sterile space, thus creating an infection.
Treatment Options
Observation
Unilateral ventilation, ventilation with high-frequency oscillation (HFO)
percutaneous drainage, decubitus positioning with the affected side down, selective intubation of the main bronchus on the uninvolved side
Surgical intervention: Injection of intrapleural fibrin sealant, percutaneous catheter placement, chest tube (associated with higher bronchopleural fistula)
Surgical resection: Video-assisted thoracoscopic surgery (VATS), lobectomy, pneumatocele removal/deroofing, pneumonectomy.
The clinical picture should be taken into account and not just the size while treating pneumatocele.
Most pneumatoceles disappear spontaneously within a few weeks to 6 to 12 months without intervention. They rarely persist for more than a year. Enlarging, complicated pneumatoceles can cause cardiorespiratory instability. It is unclear if coinfection with multiple organisms increased the risk of developing pneumatocele or is responsible for a more severe clinical presentation. Conservative management of pneumatocele is paramount for typically occurring cases along with the use of appropriately dosed antimicrobials to known infectious agents. Conservative management alone is unlikely to benefit the patient in situations of cardiorespiratory instability or extensive disease, as death has been reported.[53][54][55]
In children, 90% of pneumatocele underwent spontaneous resolution. Half of the pneumatocele persists even after drain placement.[56] A report described six children who develop a giant cyst occupying almost all the hemithorax as a part of pneumonia resolution. The air-fluid level was interpreted as a lung abscess. All these children were conservatively treatment with antibiotics and showed gradual improvement and resolution of pneumatocele upon followup.
The presence of central location( retrocardiac) makes percutaneous or surgical intervention inappropriate choice. In such cases, High-frequency oscillatory ventilation (HFOV) and selective intubation and ventilation of the main bronchus are appropriate non-invasive treatment strategies.[13][57][13]
Percutaneous needle decompression is considered when the pneumatocele has the following characteristics:
- Occupying greater than 50% of the hemithorax[58]
- Creating significant atelectasis
- Bronchopleural fistulae development
- Tension pneumatocele[59]
- Persistent signs of chest infection
- Infection within the cyst
- Bronchopleural fistula
- Risk of unable to followup outpatient
Percutaneous needle decompression risks: the development of bronchopleural fistulae[60]
The pneumatocele is also successfully managed by the injection of fibrin sealant via a pigtail catheter.[61] A biodegradable material is a preferred choice for plugging the air leak. Sclerosants used for pleurodesis include talc, antibiotics, antineoplastic drugs, and autologous blood. A study by Andres et al. treated six patients with persistent air leaks by using autologous blood infusion, with 100% success after 24 hours. Fibrin sealant is a surgical hemostatic and adhesive material used in procedures including cardiac, vascular, hepatic, and maxillofacial surgery to achieve natural adhesion for defective tissues and viscera. Using CT-fluoroscopy, real-time catheter manipulation, and precise placement of the fibrin sealant, allowing for accurate closure of the fistula was possible. This procedure is rapid and safe and may decrease the length of hospitalization.
Decompression by percutaneous pigtail catheter placement in children who develop pneumatoceles as a result of a complication of pulmonary interstitial emphysema with superimposing Respiratory syncytial virus (RSV) infection has been described in a preterm infant in a case report.[62][63][64][65]
Sometimes, patients are not suitable for earlier intervention with percutaneous drainage of the pneumatoceles due to the extent of lung disease and high risk of complications associated with full heparinization and Extracorporeal membrane oxygenation (ECMO) support.
Lobectomy is considered a form of definitive management and has been shown to quickly improve the clinical stability of some patients though mortality following this procedure has been reported. There is evidence to suggest that lobectomy is associated with lower postsurgical risk of infection, parenchymal necrosis, and need for further surgery. Lobectomy is not suitable if the amount of salvageable lung tissue is negligible and risked leaving necrotic tissue within the hemithorax.
VATS lobectomy in non-trauma settings has been demonstrated to have a reduction of postoperative morbidity. A major advantage of VATS is it avoids rib displacement. The patient should be stable enough to tolerate a double-lumen tube and video-assisted thoracic surgery exploration. In unstable patients, those with massive chest wall disruption, and/or major air loss and hemoptysis, a single lumen tube is preferred, and thoracotomy is more appropriate.[66]
Pneumonectomy is performed to obtain adequate source control of the proinflammatory and necrotic lung tissue and to evacuate the large pneumatoceles affecting ventilation. Removal of as little lung parenchyma as possible is ideal; however, extensive disease may necessitate pneumonectomy to improve cardiorespiratory status. Pediatric pneumonectomy has previously been described in the literature for enlarging pneumatoceles and bronchopulmonary fistula secondary to pneumonia; however, preoperative care was not well described.[67]
Long-term complications following pneumonectomy in children are infrequently reported. Reports suggest most complications are relatively mild and include scoliosis and changes in spirometry values though most children have no marked impairment in exercise or breathing difficulties.
V-V ECMO and possible pneumonectomy as a salvage procedure in those patients with extensive disease involving multiple lobes.[67]
Post-traumatic pulmonary pneumatoceles usually resolve spontaneously but can be complicated and can require surgery. Complete resolution of traumatic pneumatoceles varies and depends on the size and nature of the lesion. The literature has reported that time to radiological resolution averages 3 months but ranges from 4 weeks to 6 months. Larger pneumatoceles require significantly greater time for resolution. A study by Chon et al. found that lesions filled with blood or greater than 2 cm in diameter have an average resolution time of approximately 5 months.[17][68] Some pneumatoceles may enlarge in the first two weeks following trauma. This observation may prompt a search for alternative diagnoses, many of which require invasive testing and treatment. This exploration may lead to more harm than good by increasing the risk of complications.
The indications for diagnostic and therapeutic bronchoscopy in traumatic pneumatoceles include:
- Endobronchial bleeding
- Thick sputum
- Large air leak
- Mediastinal emphysema
- Lobar collapse
Urgent thoracotomy and lobectomy may be required in the case of massive hemoptysis, which is usually not life-threatening. The indications for video-assisted thoracoscopic surgery or open surgery include:
- Prolonged persistence of an air leak
- Hemothorax or pneumothorax due to pneumatocele rupture
- Failure of lung expansion
- Progressive enlargement of the pneumatocele
- Compression of functional parenchyma
Traumatic pneumatoceles may enlarge with positive-pressure ventilation leading to hypoxemia and respiratory deterioration because of inadequate ventilation. In such patients, video-assisted thoracoscopic surgery or open thoracotomy with tube decompression is necessary.
In the case of secondary infection and septic course, antibiotic treatment, according to sputum culture, antibiograms is the first step. The approach to an infected pseudocyst is similar to that for a lung abscess. If an infected pseudocyst is larger than 2 cm or there are unremitting signs of sepsis after 72 hours of antibiotics, the pseudocyst should be percutaneously drained.
If there is no clinical improvement, early CT-guided catheter drainage should be considered. If, despite the drainage, there is no observed clinical improvement, clinicians could proceed with thoracotomy or thoracoscopy.
The average spontaneous time for the radiological resolution of traumatic pneumatocele is three months. The prognosis for most traumatic pulmonary pseudocysts (TPPs) is excellent, and most lesions spontaneously disappear in three months. Followup by chest radiography or alternative imaging is recommended until resolution occurs.[17]
Neonatal pneumatoceles have mostly been described with ventilator-induced air leak conditions during the 1970s and 1980s. Surfactant replacement therapy and lung-protective ventilation strategies have resulted in the decreasing incidence of all intrathoracic air leaks including pneumatoceles
Pneumatocoele, as a result of complicated pneumonia in patients with left ventricular assistive devices (LVAD), has been described in the literature, with successful treatment with surgical resection.[69]
Prophylactic antibiotic therapy is not necessary unless other injuries are present or surgical procedures are performed. Sputum cultures should be collected from all patients who have sustained significant blunt chest trauma, especially in those with hemoptysis, pulmonary contusion, or traumatic pneumatocele. Culture results can then be used to guide treatment decisions if infection occurs. Because pneumatocele infection usually manifests late in its clinical course, and thus prolonged antibiotic prophylaxis could encourage resistant strains and promote colonization. Persistent fever, unremitting leukocytosis, or radiographic changes should prompt suspicion of possible infection, and antibiotic therapy started.
Early lobectomy should be considered in cases of:
- Extensive lung abscess surrounded by necrotic tissue
- Failed bronchoscopic treatment of extensive bleeding
- Lack of response to conservative treatment
One study suggested that pseudocysts larger than six cm or those that have failed to improve following conservative treatment, are potential candidates for surgical resection.
Late thoracotomy has been reported up to six months after trauma due to pneumonic infiltration and persistent cavitary size. Romero et al. reported a case of giant hemopneumatocele that resolved spontaneously with conservative treatment. This observation becomes particularly important in patients with multiple thoracic injuries who may not be able to tolerate surgery.
Differential Diagnosis
- Lung abscess
- Bronchial cyst
- Post-inflammatory pneumatocele
- Pulmonary sequestration
- Tuberculosis
- Mycosis
- Herniation of viscera
- Esophageal rupture
- Metastatic neoplasm
- Granulomatosis with polyangiitis
- Hydatid cysts
- Langerhans cell histiocytosis
- Marfan syndrome
- Proteus syndrome
- Neurofibromatosis may give rise to pulmonary cystic changes (giant bulla case) blebs, bullae, congenital cysts
- Coccidioidomycosis
- Pneumonia
- Empyema
- Fungus ball
- Aspergilloma
- Tuberculoma
- Lung cancer
- Cystic fibrosis
- Primary ciliary dyskinesia
- Primary immunodeficiencies.
- Cystic adenomatoid malformation
Cyst: Cysts have variable wall thickness but are usually thin-walled (< 2 mm) and occur without associated pulmonary emphysema on CT scans. Pathologically, a cyst is any round circumscribed space surrounded by an epithelial or fibrous wall of variable thickness.
Bullae: A bulla is an airspace measuring more than 1 cm that is sharply demarcated by a thin wall not more than 1 mm thickness. Radiologically, it appears as a rounded focal lucency or decreased attenuation. Bullae are usually located in the subpleural lung rather than within the lung parenchyma. Multiple bullae are usually accompanied by adjacent paraseptal and centrilobular emphysema. Bullae can be distinguished from cysts by their almost imperceptible thin-wall, subpleural location, and accompanying adjacent emphysema.
Cavitary lesion: A cavity is a gas-filled space that is observed as a lucency or low-attenuated area within pulmonary consolidation, a mass, or a nodule. Cavity wall thickness may vary, but the wall is usually relatively thick. Some cavitary lesions may appear as thin-walled cavities or cysts at their end-stage presentation. Many different diseases present as cavitary lesions e.g., acute to chronic infections, chronic systemic diseases, primary or metastatic malignancies. A cavity is differentiated from a cyst by the presence of a thicker wall and a more irregular shape.[70][71]
A history of trauma helps distinguish post-traumatic pneumatocele from these conditions. However, if the lesion does not decrease in size over time, etiologies other than TPP should be sought out. This is particularly true in countries where other causes of cavitary pulmonary lesions are endemic. A previous chest x-ray may help perform the comparison and narrowing differentials.
Ventilator-induced pneumatoceles are a manifestation of intrathoracic air leaks of prematurity. They are markers for ventilator-induced lung injury and are associated with significant mortality. Conservative management with a reduction in mean airway pressure is effective in the resolution of this condition, and surgical intervention is generally not necessary.[14][22][72]
Prognosis
Simple, uncomplicated pneumatoceles have a good prognosis with complete resolution, and the time interval varies from 3 months to 2 years.
If complications happen, early surgical intervention would be beneficial to avoid mortality/morbidity. There is no clear data available regarding the mortality of patients developing complications of pneumatocele.
Complications
- The most important complications of pneumatoceles are related to errors in diagnosis and subsequent interventions, leading to more complications.
- Rupture resulting in pneumothorax or tension pneumothorax with a mediastinal shift. Conventional tube thoracostomy is the treatment of choice.
- Pneumomediastinum[73]
- Infection and empyema/ lung abscess formation. It is the most common complication of traumatic pulmonary pneumatocele. Infected pneumatoceles carry a higher mortality than a typical lung abscess. The risk of secondary infection is increased by pulmonary contusion that impairs bacterial clearance. Treatment of infected TPP is similar to that of a lung abscess.[74]
- Pyopneumothorax
- Fistulous pleural extrathoracic communication from incomplete anti-TB treatment
- Hemothorax, hemopneumothorax
- Continuous positive airway pressure may cause TPP enlargement and compression of adjacent lung tissue, leading to hypoxemia and cardiopulmonary instability.[17]
Consultations
In pediatric cases, a pediatrician and pulmonary pediatrist coordinate among themselves to plan a treatment option. Cardiothoracic surgery is needed for lobectomy, chest tube, pigtail catheter, and fibrin sealant injections.
In adult cases, surgeons (trauma, cardiothoracic), pulmonologists are needed to make a decision in terms of management that varies from case to case. The ICU team is involved in critically ill and hemodynamically unstable patients.
Deterrence and Patient Education
Explain the nature and outcomes of the pneumatocysts in an appropriate setting (trauma/infection). The patient should be educated about the symptoms to monitor for possible complications. Subsequent imaging is necessary and should be emphasized to avoid potentially serious consequences.
Pearls and Other Issues
Pneumatoceles are important complications after trauma, infection, burn, and chemical associated lung injury. It’s important to diagnose and differentiate it from other pathologic conditions as treatment can vary greatly. Failure to recognize can lead to misleading diagnosis and inappropriate treatment, causing more harm than good towards patient care.
Enhancing Healthcare Team Outcomes
It is imperative to recognize pneumatocele in clinical settings and differentiate from many other similar diagnoses. Opinion from radiologists should be taken in uncertain situations, and the final decisions should be made in clinical settings to differentiate pneumatocele from cyst, abscess, bullae, infectious causes.
Complicated cases benefit from an early surgical intervention that varies from minimally invasive to large surgeries such as lobectomy, pneumonectomy, chest tube/ pigtail insertion, and instillation of sealants.