[1]
Michelson J, Moskovitz P, Labropoulos P. The nomenclature for intra-articular vertical impact fractures of the tibial plafond: pilon versus pylon. Foot & ankle international. 2004 Mar:25(3):149-50
[PubMed PMID: 15006336]
[2]
Jacob N, Amin A, Giotakis N, Narayan B, Nayagam S, Trompeter AJ. Management of high-energy tibial pilon fractures. Strategies in trauma and limb reconstruction. 2015 Nov:10(3):137-47. doi: 10.1007/s11751-015-0231-5. Epub 2015 Sep 25
[PubMed PMID: 26407690]
[3]
Rüedi T. Fractures of the lower end of the tibia into the ankle joint: results 9 years after open reduction and internal fixation. Injury. 1973 Nov:5(2):130-4
[PubMed PMID: 4774764]
[4]
Rüedi TP, Allgöwer M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clinical orthopaedics and related research. 1979 Jan-Feb:(138):105-10
[PubMed PMID: 376196]
[5]
Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, Seligson D. Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta orthopaedica Belgica. 2011 Aug:77(4):432-40
[PubMed PMID: 21954749]
[6]
Cole PA, Mehrle RK, Bhandari M, Zlowodzki M. The pilon map: fracture lines and comminution zones in OTA/AO type 43C3 pilon fractures. Journal of orthopaedic trauma. 2013 Jul:27(7):e152-6. doi: 10.1097/BOT.0b013e318288a7e9. Epub
[PubMed PMID: 23360909]
[7]
Ballal A, Rai HR, Shetty SM, Mathias LJ, Shetty V, Shetty A. A Prospective Study on Functional Outcome of Internal Fixation of Tibial Pilon Fractures with Locking Plate using Minimally Invasive Plate Osteosynthesis Technique. Journal of clinical and diagnostic research : JCDR. 2016 Jan:10(1):RC01-4. doi: 10.7860/JCDR/2016/15284.7013. Epub 2016 Jan 1
[PubMed PMID: 26894132]
[8]
Wyrsch B, McFerran MA, McAndrew M, Limbird TJ, Harper MC, Johnson KD, Schwartz HS. Operative treatment of fractures of the tibial plafond. A randomized, prospective study. The Journal of bone and joint surgery. American volume. 1996 Nov:78(11):1646-57
[PubMed PMID: 8934478]
Level 1 (high-level) evidence
[9]
Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. Journal of orthopaedic trauma. 1999 Feb:13(2):92-7
[PubMed PMID: 10052782]
[10]
Chen SH, Wu PH, Lee YS. Long-term results of pilon fractures. Archives of orthopaedic and trauma surgery. 2007 Jan:127(1):55-60
[PubMed PMID: 17004076]
[11]
Korkmaz A, Ciftdemir M, Ozcan M, Copuroğlu C, Sarıdoğan K. The analysis of the variables, affecting outcome in surgically treated tibia pilon fractured patients. Injury. 2013 Oct:44(10):1270-4. doi: 10.1016/j.injury.2013.06.016. Epub 2013 Jul 18
[PubMed PMID: 23871428]
[12]
Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clinical orthopaedics and related research. 1993 Jul:(292):108-17
[PubMed PMID: 8519097]
[13]
Topliss CJ, Jackson M, Atkins RM. Anatomy of pilon fractures of the distal tibia. The Journal of bone and joint surgery. British volume. 2005 May:87(5):692-7
[PubMed PMID: 15855374]
[14]
Schulz AP, Fuchs S, Simon L, Seide K, Paech A, Queitsch C. Severe Fracture of the Tibial Pilon: Results with a Multidirectional Self-locking Osteosynthesis Plate Utilizing a Two-stage Procedure. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2008 Aug:34(4):391-6. doi: 10.1007/s00068-007-2209-6. Epub 2007 Nov 14
[PubMed PMID: 26815817]
[15]
Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. Journal of orthopaedic trauma. 1999 Feb:13(2):78-84
[PubMed PMID: 10052780]
[16]
Anderson DD, Mosqueda T, Thomas T, Hermanson EL, Brown TD, Marsh JL. Quantifying tibial plafond fracture severity: absorbed energy and fragment displacement agree with clinical rank ordering. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2008 Aug:26(8):1046-52. doi: 10.1002/jor.20550. Epub
[PubMed PMID: 18327811]
[17]
Ibrahim DA, Swenson A, Sassoon A, Fernando ND. Classifications In Brief: The Tscherne Classification of Soft Tissue Injury. Clinical orthopaedics and related research. 2017 Feb:475(2):560-564. doi: 10.1007/s11999-016-4980-3. Epub 2016 Jul 14
[PubMed PMID: 27417853]
[18]
Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. The Journal of trauma. 1984 Aug:24(8):742-6
[PubMed PMID: 6471139]
[19]
Luo TD, Eady JM, Aneja A, Miller AN. Classifications in Brief: Rüedi-Allgöwer Classification of Tibial Plafond Fractures. Clinical orthopaedics and related research. 2017 Jul:475(7):1923-1928. doi: 10.1007/s11999-016-5219-z. Epub 2017 Jan 4
[PubMed PMID: 28054323]
[20]
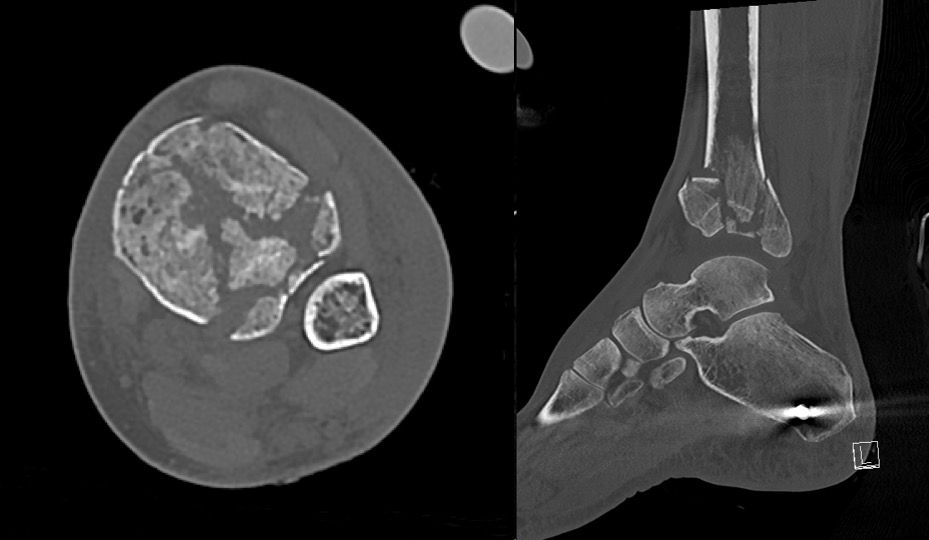
Tornetta P 3rd, Gorup J. Axial computed tomography of pilon fractures. Clinical orthopaedics and related research. 1996 Feb:(323):273-6
[PubMed PMID: 8625591]
[21]
Rüedi T, Matter P, Allgöwer M. [Intra-articular fractures of the distal tibial end]. Helvetica chirurgica acta. 1968 Nov:35(5):556-82
[PubMed PMID: 4974693]
[22]
Helfet DL, Koval K, Pappas J, Sanders RW, DiPasquale T. Intraarticular "pilon" fracture of the tibia. Clinical orthopaedics and related research. 1994 Jan:(298):221-8
[PubMed PMID: 8118979]
[23]
Howard JL, Agel J, Barei DP, Benirschke SK, Nork SE. A prospective study evaluating incision placement and wound healing for tibial plafond fractures. Journal of orthopaedic trauma. 2008 May-Jun:22(5):299-305; discussion 305-6. doi: 10.1097/BOT.0b013e318172c811. Epub
[PubMed PMID: 18448981]
[24]
Kubiak EN, Beebe MJ, North K, Hitchcock R, Potter MQ. Early weight bearing after lower extremity fractures in adults. The Journal of the American Academy of Orthopaedic Surgeons. 2013 Dec:21(12):727-38. doi: 10.5435/JAAOS-21-12-727. Epub
[PubMed PMID: 24292929]
[25]
Ovadia DN, Beals RK. Fractures of the tibial plafond. The Journal of bone and joint surgery. American volume. 1986 Apr:68(4):543-51
[PubMed PMID: 3957978]
[26]
Cutillas-Ybarra MB, Lizaur-Utrilla A, Lopez-Prats FA. Prognostic factors of health-related quality of life in patients after tibial plafond fracture. A pilot study. Injury. 2015 Nov:46(11):2253-7. doi: 10.1016/j.injury.2015.06.025. Epub 2015 Jun 18
[PubMed PMID: 26115581]
Level 2 (mid-level) evidence
[27]
Thordarson DB. Complications after treatment of tibial pilon fractures: prevention and management strategies. The Journal of the American Academy of Orthopaedic Surgeons. 2000 Jul-Aug:8(4):253-65
[PubMed PMID: 10951114]