Continuing Education Activity
Paget disease is a skeletal growth disorder in which abnormalities such as unusual bone growth can occur in several multifactorial ways. It is the second most frequently diagnosed metabolic bone disease after osteoporosis. It is often manifested by diffuse pain and radiologically visible bone changes throughout the musculoskeletal system. The disease can affect any bone in the body but is more often seen in the spine, pelvis, and skull. It does not spread to other bones but can deteriorate in the affected area and even progress to a sarcoma, which may be a fatal bone cancer. The most common biochemical finding is elevated levels of alkaline phosphatase, bone-specific. It can be treated very effectively with the use of bisphosphonates. This activity reviews the etiology, presentation, evaluation, and management of Paget disease of the bone and examines the role of the interprofessional team in evaluating, diagnosing, and managing the condition.
Objectives:
Assess the hypothesized etiologies of Paget disease of the bone and its associated complications, such as fractures, nerve compression syndromes, and secondary osteoarthritis.
Implement evidence-based treatment strategies for Paget disease of the bone, including pharmacological interventions, to manage symptoms and reduce disease progression.
Assess the response to treatment and monitor disease activity through regular clinical evaluations and appropriate imaging techniques.
Select strategies to improve care coordination among interprofessional team members to improve outcomes for patients affected by Paget disease of the bone.
Introduction
Paget disease is a skeletal growth disorder in which abnormalities such as unusual bone growth can occur in several multifactorial ways. This is often manifested by diffuse pain throughout the musculoskeletal system.[1][2][3][4]
The condition presents with excess osteoclastic activity followed by a compensatory increase in osteoblastic activity, leading to the formation of disorganized bone, which is less compact, mechanically weaker, highly vascular, and more susceptible to fracture. Fortunately, more than three-fourths of patients with Paget disease are asymptomatic. It is the second most commonly seen metabolic bone disorder in older individuals after osteoporosis. The condition can affect 1 or more bones, but the axial skeleton is most often involved (spine, pelvis, and skull). The condition does not spread to other bones but can progress in the preexisting site. A deadly complication of Paget disease is the development of pagetic sarcoma, a tumor that can be fatal.
The cause of Paget disease remains unknown, but there are genetic and environmental associations. The disorder is most common in Europe, North America, and Australia but rare in Asia and Africa. Several viruses have been identified in the diseased bone, but their role in the disease pathology remains a mystery.
Etiology
Some literature sources suggest that the family of paramyxoviruses solely causes Paget disease of the bone.[5] However, many studies have determined that the osteoclast generation of a unique cytokine found exclusively in the bone marrow of patients diagnosed with Paget disease may be the primary insult. This cytokine is known as IL-6.
A strong genetic predisposition to the disorder has been determined based on population studies.[6][7] Besides finding an association between HLA markers, siblings are at high risk for developing the disorder.
Epidemiology
Paget disease is usually seen in individuals older than 50 years of age. Around the world, it is reported that the prevalence of the disease has decreased during the past 2 decades, currently estimated between 1.5% to 8.3%.[8] It is common in Caucasians of northern European descent.[9] Paget disease is equally common in males and females. In the US, it is said to affect 1 to 3 million people, but most of the patients are asymptomatic. The disorder is slightly more common in white males. The disorder usually presents in the fourth to fifth decade of life, but the diagnosis is often made a decade later.
Pathophysiology
Paget disease of the bone occurs with an increase in bone resorption, leading to a decrease in bone mass and lytic structures. This process gives rise to osteoblasts from the bone utilizing a sensing system that allows them to increase their activity.
Paget disease's pathological process occurs in 4 stages. It begins with osteoclastic activity, followed by a hybrid osteoclastic/osteoblastic process. In the third stage, osteoblastic activity is observed and culminates in the final stage, where malignant degeneration is seen.
The disease occurs in isolated pockets but is usually progressive. There is often erythema and warmth over the involved bone due to hypervascularity, which can lead to high-output heart failure.
The disease can affect almost every bone in the skeleton but has an affinity for the long bones, axial skeleton, and the skull. Involvement of the feet and hands is rare.
Histopathology
The key histopathological feature of Paget disease involves bone architecture and includes the 3 phases of the disease: mixed, osteolytic, and osteosclerotic. These phases may occur at the same time or separately. The osteolytic phase has areas of resorption due to a significant increase in the number of abnormal osteoclasts that contain dozens of nuclei. The osteoblastic phase that follows is disorganized. The bone development is fragmented and irregular. The presence of irregularly shaped bone particles appears like jigsaw-puzzle pieces and is the hallmark feature of Paget disease. As the disorder advances, the osteoblastic phase becomes dominant, resulting in excessive bone formation, which is fibrous and coarse. The marrow space is filled with vascularized fibrous tissue, which accounts for the persistent warmth and fever.
The bone in Paget disease does not have centralized blood vessels or Haversian systems. Once the osteoblastic phase subsides, the new bone is poorly mineralized and lacks structural integrity.[10][11][12]
History and Physical
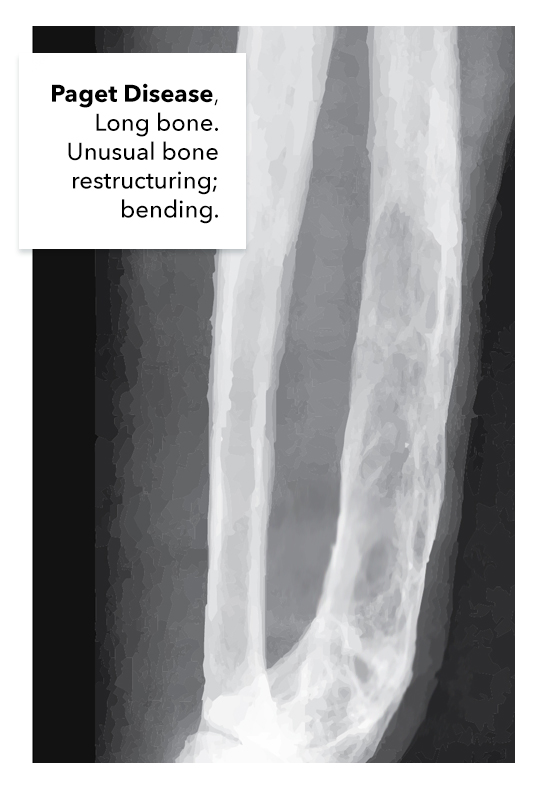
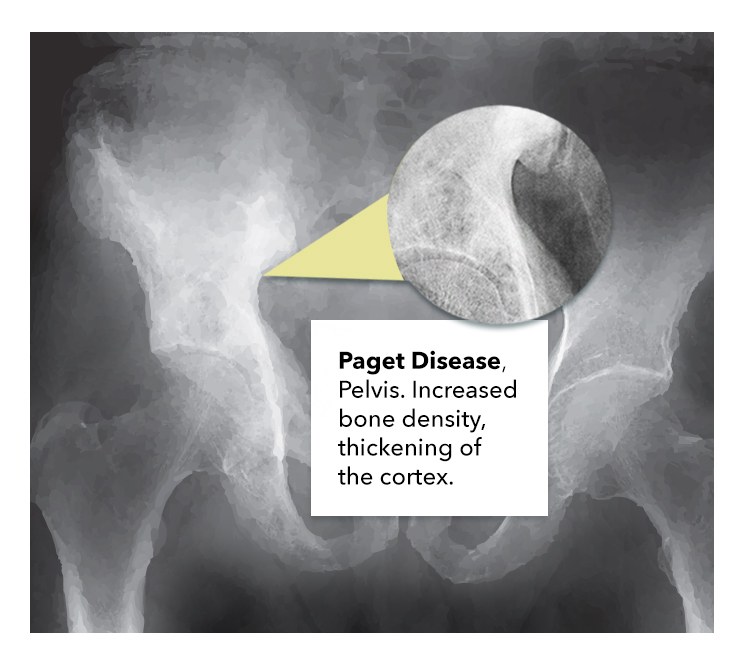
Many patients who present to the clinic with pathognomonic features associated with Paget disease are usually asymptomatic. Most patients with the condition are often diagnosed by an incidental finding on an x-ray study. The disease will present with 1 bone affected in one-third of cases. The spine and pelvis are commonly affected (see Image. Paget Disease Pelvis), and among the long bones, the femur is often involved (see Image. Paget Disease of the Long Bone). Symptomatic patients can present with the following:
- Pain involving the bones and joints
- Diffuse joint stiffness
- Abnormally enlarged skull
- Musculoskeletal deformities
- Loss of hearing (due to the involvement of the petrous temporal bone)
- Migraines
- Fractures
- Heart failure
- Cranial nerve neuropathies
- Headaches
- Skull and jaw deformity
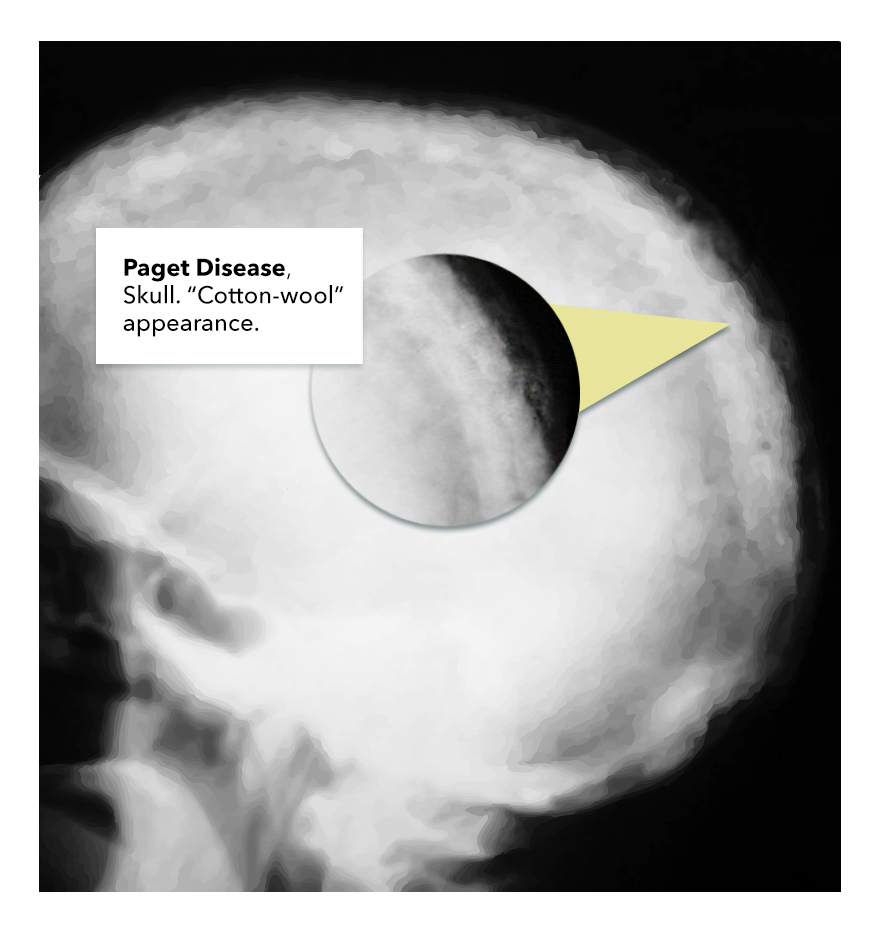
The lumbar spine, sacrum, and skull are involved in most cases (see Image. Paget Disease Skull). Pain is a common feature and is worse with weight-bearing.
The patient's physical exam may show bone deformity or angulation, localized pain to palpation, and increased warmth. The patient's gait may be altered, and there may be balance problems.
Incomplete fractures are common in Paget disease and are seen in the tibia and femur. Even mild injuries can result in fractures. Femur fractures often involve the subtrochanteric region.
Osteosarcoma is a rare complication but should be suspected in a patient with a sudden increase in swelling or bone pain. This disorder can be fatal. Giant cell tumors may also arise in pagetic bone and involve the facial bones. With vertebral fractures, acute spinal cord compression may occur.
An increase in cardiac output is noted in 20% of patients when the axial skeleton is involved. In addition, calcified aortic stenosis is common in this population.
Evaluation
Tests to assist in the diagnosis of Paget disease include the following:
- Bone scan
- Bone x-ray
- Elevated markers of bone breakdown, such as N-telopeptide
The disease may also present with the following findings:
- Elevated alkaline phosphatase (ALP)
- Normal serum calcium and phosphate
Measurement of serum ALP is useful, as are urine levels of hydroxyproline, C-telopeptide, and N-telopeptide.
Procollagen N-terminal peptide is also a sensitive serum marker for bone formation.
Hyperuricemia is common and is due to a high turnover of bone.
Secondary hyperparathyroidism occurs in approximately 10% of patients due to inadequate calcium in the face of increased demand.[13]
Plain x-rays may reveal cortical and trabecular thickening, osteosclerosis that looks like arthritis, bone expansion, or osteolytic areas.[2]
Bone scans can help document the extent of disease and should be used to follow treatment (see Image. Abnormal Uptake in the Left Hemipelvis). In addition, a bone scan can pick up early changes in bone even before the patient develops symptoms.
Treatment / Management
Some patients diagnosed with Paget disease may not require treatment.[14][15][16] This patient cohort includes the following:
- Patients with no abnormal blood tests
- Patients who have no active signs of the disease and those who are asymptomatic
The most commonly treated patients diagnosed with Paget disease include the following:
- Patients with abnormal bone defects
- Patients who have weight-bearing bones involved
- Patients with skull deformities
- Patients with evidence of a rapidly progressing bone change
- Patients with complaints of diffuse pain
Several treatment regimens aid in prophylactically preventing bone breakdown and subsequent bony formation.[17] Some of the more common drug therapies include the following:
- Bisphosphonates have been approved as the first-line treatment option due to their influence on bone remodeling.[18]
- Calcitonin is usually a second-line treatment and can also have an analgesic effect. This drug assists in bone absorption.
- Denosumab has been used off-label in cases of bisphosphonate intolerance or contraindication, with good results.
- Supplements such as calcium and vitamin D have been known to provide some symptomatic benefits.[19]
- Pain management is usually achieved by either NSAIDs or acetaminophen.
Surgery is only offered as an option to patients diagnosed with Paget disease with a progression into osteosarcoma. Most patients diagnosed with osteosarcoma are often offered palliative options such as amputating the affected limb. In many cases, clinicians are tasked with making judgment calls about which treatment options to offer to the wide spectrum of patients diagnosed with Paget disease. For example, younger patients are usually offered a surgical procedure where they could potentially salvage the limb by resecting the tumor with wide margins. This may not be a viable alternative for an older patient with multiple comorbidities and risk factors. Patients may also develop pathological fractures that require radiation and internal fixation to relieve pain. Chemotherapy is an ineffective option for patients diagnosed with sarcoma. It is important to note that surgical failure rates are high in this group of patients. Often, revision surgery is indicated.
Patients with cauda equina and other nerve compression complications will frequently require laminectomy.
Differential Diagnosis
The differential diagnosis of Paget disease includes the following:
- Osteomalacia
- Osteoporosis
- Malignancy of the bone, primary or metastatic
- Renal osteodystrophy
- Osteoarthritis
- Osteopenia
- Fibrous dysplasia
Prognosis
The prognosis for treated patients is good, especially if the disease is in its early stages. Paget disease of the bone has no cure, but the disorder can be controlled by slowing down or even stopping its progression. Patients with polyostotic disease have poorer outcomes than those with monostotic disease. The morbidity is usually due to fractures, chronic pain, bone deformity, and neurological complications. Once the patient develops sarcomatous degeneration, the survival rate may be very poor.
Complications
Complications include the following:
- Secondary osteoarthritis
- Vertigo
- Deafness
- Dental malocclusion
- Tinnitus
- Cranial nerve compression
- Basilar invagination
- Cauda equina syndrome
- Fractures
- Hashimoto thyroiditis
- Osteopetrosis
- Dupuytren contracture
- Development of osteosarcoma
- High-output cardiac failure
Deterrence and Patient Education
Patients diagnosed with Paget disease of the bone need to be educated on the symptoms and complications of the disease to help with timely diagnosis and progression. With the use of current treatments, there is a high probability of the disease being controlled and avoiding any complications at all. The patient should be made aware of the bones involved in their disease and the relevant complications of each site, including the development of deafness or heart failure. This way, they will be more likely to seek medical assistance for any signs of problems, and they can be treated more effectively.
Pearls and Other Issues
Diet and Activity
- While there is no specific diet for patients with Paget disease of the bone, those prescribed bisphosphonates should ensure adequate calcium and vitamin D intake.
- Aggressive physical activity is not recommended, as fracture risk is high. However, muscle-strengthening exercise at a low level is recommended.
Deterrence
To date, there is no way to prevent Paget disease since the cause remains unknown. For family members of a patient with Paget disease, some physicians recommend monitoring ALP levels every 2 years. If the levels are within the normal range, then imaging of the bone may also be performed.
Guidelines Summary
Current endocrine guidelines for Paget disease:
- Obtain plain x-rays of the affected body part.
- Determine the extent of bone involvement with a radionuclide scan.
- Measure levels of serum ALP to evaluate bone formation/resorption and also assess response to treatment or follow untreated patients.
- Patients at risk for complications like fractures should be started on bisphosphonates, with alendronate 40 mg daily being the first choice in the oral category.
- Another straightforward treatment option is a single 5 mg dose of intravenous zoledronic acid if there are no contraindications.
- If a patient has normal ALP levels, monitor the disease with a specific marker for bone formation.
- One can follow patients with serial bone scans to assess the disease if bone markers are all normal.
- The use of bisphosphonates is effective in slowing down the progression of disease and/or the hearing loss.
- If patients with Paget disease need surgery, one should consider pretreatment with bisphosphonates.[20]
Enhancing Healthcare Team Outcomes
Paget disease is the second most common bone disorder in older individuals and is associated with very high morbidity and mortality. There is no cure for the disorder, and early diagnosis is key. Asymptomatic patients do not require treatment.
Managing Paget's disease of the bone requires a collaborative, patient-centered approach involving physicians, advanced care practitioners, nurses, pharmacists, and other healthcare professionals. The interprofessional team often consists of a rheumatologist or endocrinologist, neurologist, audiologist, internist, nurse practitioner, and a pathologist.
Patients need to be referred to a physical therapist as they will benefit from learning about body mechanics, proper posture, and avoidance of trauma. Because the patients have weak bones, they need to be educated about protected weight-bearing and the use of ambulatory devices. The nurse should reinforce education about safe ambulation to prevent fractures. Immobility should be avoided as it also increases morbidity. The pharmacist should educate the patient on medication compliance and potential adverse effects, and nursing should watch for signs of adverse drug effects and monitor treatment progress on subsequent visits, reporting any findings to the interprofessional team.
Symptomatic patients usually can be managed by bisphosphonates, calcitonin, and vitamin D supplements. The pharmacist should choose the best medication and dosing to optimize the therapeutic effect. A pain specialist should also be involved as these patients have moderate to severe bony pain that is often disabling.
Surgery is usually offered to patients diagnosed with Paget disease when there is a progression into osteosarcoma. Most patients diagnosed with osteosarcoma are usually offered palliative options such as amputating the affected limb. Patients may also develop pathologic fractures needing radiation and internal fixation to relieve the pain. Chemotherapy is an ineffective option for patients diagnosed with sarcoma. It is important to note that surgical failure rates are high in this group of patients.[2][21]
Managing Paget's disease of the bone demands a multidisciplinary team effort. Healthcare professionals must continually update their skills, adopt evidence-based strategies, fulfill their respective responsibilities, communicate effectively, and coordinate care to provide patient-centered care, improve outcomes, enhance patient safety, and optimize team performance. This holistic team approach benefits individual patients and contributes to the overall success of Paget disease management.