Continuing Education Activity
The mental nerve supplies sensation to the lower lip, buccal mucosa, and skin of the chin ventral to the mental foramen. Mental nerve blocks allow for excellent anesthesia during a variety of procedures, including during dental work and intraoral and lower facial laceration repair. This activity reviews the indications, contraindications, and techniques involved in performing a mental nerve block and highlights the role of the interprofessional team in the care of patients undergoing this procedure.
Objectives:
Outline the indications for a mental nerve block.
Explain the location of the mental foramen and the sensory distribution of the mental nerve.
Summarize the intraoral and percutaneous mental nerve block techniques.
Review the importance of improving coordination among the interprofessional team to enhance care for patients undergoing mental nerve blocks.
Introduction
The mental nerve supplies sensation to the lower lip, buccal mucosa, and skin of the chin ventral to the mental foramen. It excludes the lower teeth, including the premolars, innervated by the incisive nerve (see Image. Mental Nerve).[1] Therefore, local anesthesia to the mental nerve is required for various procedures, including dental treatment and laceration repairs of the lower lip and chin area that are frequently encountered in the emergency department.[2] A nerve blockage is less painful than infiltrating local anesthesia in the surroundings of the laceration site, and it will prevent the distortion of the soft tissues and swelling that local infiltration generates. Many healthcare clinicians widely employ the mental nerve block, especially dentists, dermatologists, plastic surgeons, and emergency room providers. Two approaches to the mental nerve block technique have been described in the literature, percutaneous and intraoral. Although the intraoral approach proves to be less painful than the percutaneous, non-dentist practitioners mostly use the extraoral block.[3]
Anatomy and Physiology
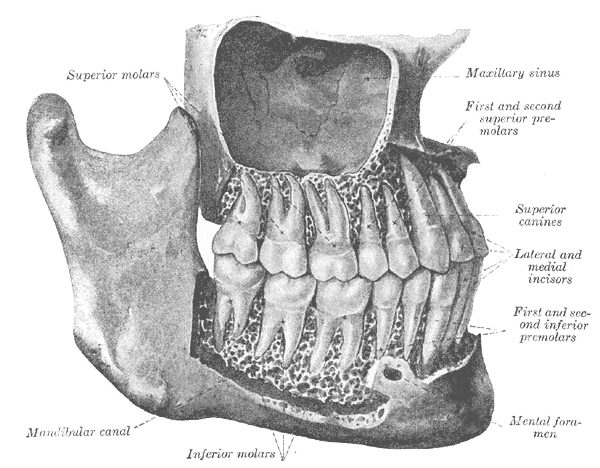
The mandibular branch of the trigeminal nerve (third branch) leaves the cranium through the foramen ovale. Immediately after, it gives rise to two nerves, a nerve to the medial pterygoid muscle and nervus spinosus. The trunk of the mandibular nerve then splits into two branches, anterior and posterior. The anterior branch mostly gives motor innervation, and the posterior branch, mainly sensory, has 3 divisions: auriculotemporal, inferior alveolar, and lingual nerve. The inferior alveolar nerve enters the mandible through the mandibular foramen, traverses the mandibular canal, and exits through the mental foramen, receiving the name of the mental nerve.[4] The incisive nerve continues in the mandibular canal to innervate the premolars, canines, and incisors [1]. See Image. Permanent Teeth, Viewed From the Right.
The mental foramen is most commonly located halfway between the alveolar crest and the inferior border of the mandible in direct line with the second premolar or between the two premolars [5]. However, it is hard to determine its exact position since it varies for every individual. On the horizontal plane, the foramen can localize mesial, distal, or between the apices of the premolar roots. On the vertical plane, it can be found above, at, or below the apices of the premolars. The variations are influenced by gender, age, race, and technique used for assessment (ie, palpation, Panorex, computed tomography scan). Furthermore, the alveolar bone resorption, typical of edentulous patients, makes the location of the mental foramen closer to the alveolar crest [6]. Despite its variability, multiple studies have demonstrated complete anesthesia when localizing the foramen with palpation and landmarks.
Indications
The mental nerve block is particularly useful in lacerations of the skin of the lower lip or chin, avoiding injecting in the injured site that may bring complications such as edema and distortion of the soft tissues [1]. Procedures near the mandibular midline may require a bilateral mental nerve block. The technique can also be applied to dermatologic surgery. For example, it remains an alternative to sedation in elderly patients or with multiple comorbidities when performing Mohs micrographic surgery [7].
Dentists use the mental/incisive nerve block either alone or in addition to an inferior alveolar nerve block [8]. Studies have shown that just under half of patients develop pulp anesthesia in the first molars, 82% to 100% develop pulp anesthesia in the premolars, and almost 40% in the lateral incisors. There is a greater chance of success of incisive nerve block if the injection is given inside the foramen for the second premolar and canine. Injection external to the foramen is typically successful for skin and mucosal procedures [9].
Contraindications
Contraindications to mental nerve block include:
- Allergy to local anesthetics
- Active facial or intraoral infectious lesions (herpes infection, cellulitis)
- Inability to tolerate intraoral injections
Equipment
The following equipment is necessary to perform a mental nerve block:
- Small-bore needle (25 to 30 gauge or smaller)
- Small syringe (2 to 5 mL)
- Local anesthesia (with or without epinephrine)
- Gloves
- Topical anesthesia if using an intraoral approach
- Topical antiseptic if using an extraoral approach [7]
Preparation
The patient should ideally be seated or lying with their head placed back against a firm surface to stabilize the head and prevent movement during the procedure.
Technique or Treatment
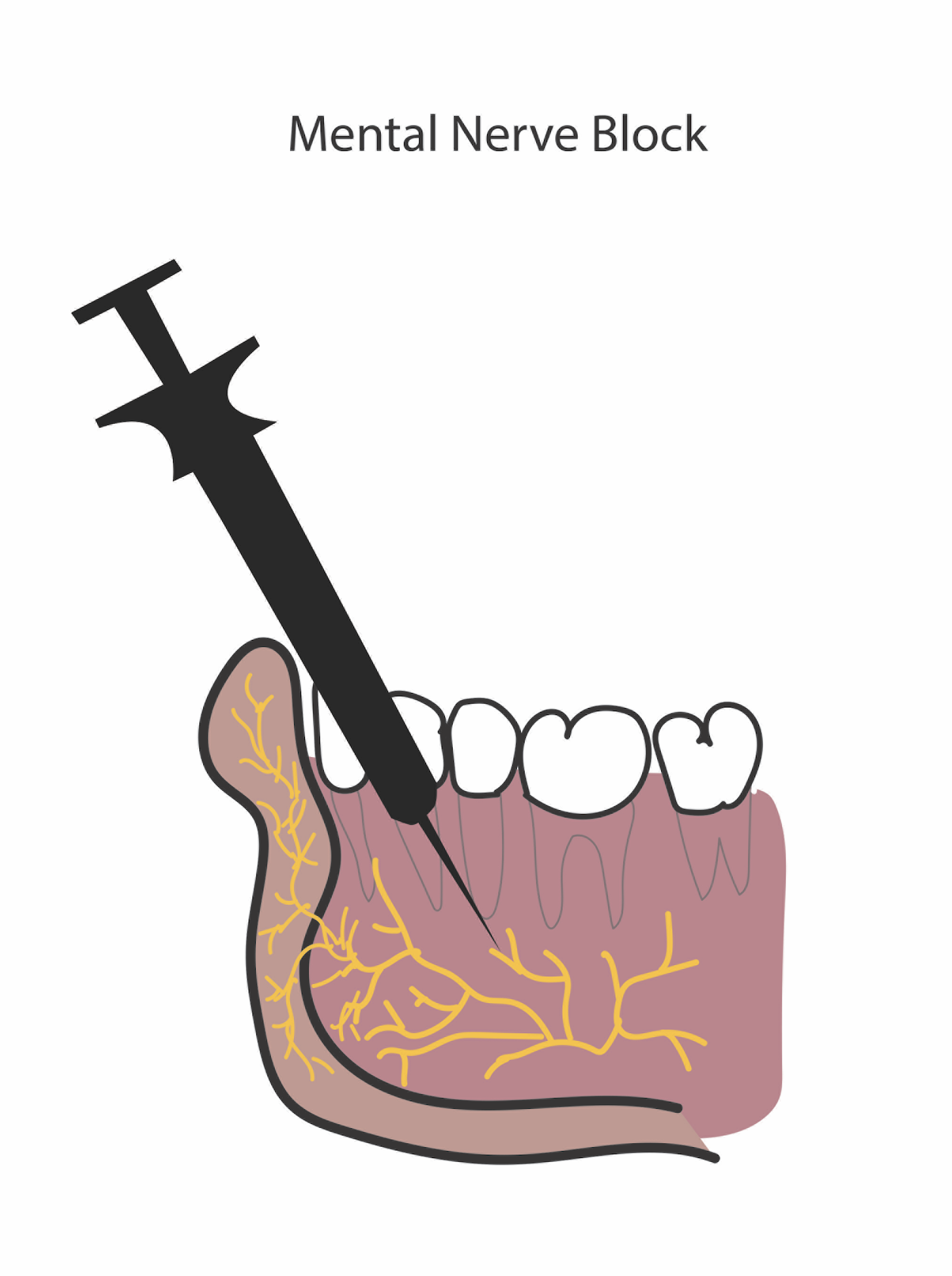
There are two described techniques for performing this nerve block: intraoral and extraoral (percutaneous). See Image. Administration of a Mental Nerve Block. Syverud et al compared these 2 approaches and found that the intraoral block with the application of topical anesthesia was less painful than the percutaneous injection [3]. Intraoral procedures are more successfully anesthetized via an intraoral approach, while skin anesthesia can be achieved with either approach with equal efficacy.
Percutaneous
- Identify the location of the mental foramen with the left index finger (as described above in Anatomy and Physiology)
- Prepare the skin with topical antiseptic (like isopropyl)
- Insert a 27-gauge needle at the injection point approximately 1 cm toward the foramen
- Aspirate to prevent vascular injection
- Avoid intra-foraminal injection by withdrawing the needle if the patient reports paresthesia
- Instill 1.5 to 3 mL local anesthetic [3]
Intraoral
- Identify the injection site (as described above in Anatomy and Physiology)Apply topical anesthesia on the injection site for approximately 60 seconds
- Retract the lower lip and insert a small-gauge needle parallel to the premolar at about 1 cm depth ( the thumb remains placed just below the mental foramen as palpated previously)
- Avoid intra-foraminal injection by withdrawing the needle if the patient reports paresthesia
- Aspirate to exclude vascular injection
- Instill 1.5 to 3 mL local anesthetic [3]
Slow injection of anesthetic has been proven more comfortable to patients than a brisk one, and anesthesia success is the same with both.[9] Pinprick sensation on the inferior lip and chin and absent light touch signify a successful block.[3]
Complications
Needle entry into the mental foramen is unnecessary for the mental nerve's successful anesthesia and may increase the risk of permanent nerve damage or accidental intravascular injection.[10] Therefore, the extra-foraminal injection is safest and still provides complete anesthesia to the skin and soft tissues anterior to the nerve.
Clinical Significance
Anesthesia via nerve block of the mental nerve just as it exits the mental foramen provides excellent anesthesia to the skin and soft tissues of the ipsilateral chin and the lower lip. This block is relatively easy to perform following the landmarks, is safe, and is simple to teach to operators. It can prevent the need for procedural sedation or the risk of tissue distortion occurring with local infiltration in an outpatient emergency, dermatology, or surgical setting.
Enhancing Healthcare Team Outcomes
The mental nerve block provides excellent anesthesia to the skin and soft tissues of the ipsilateral chin and the lower lip; as a consequence, all members of the healthcare team should be familiar with the procedure and assist in performing this block. Non-dentist clinicians should familiarize themselves with the intraoral approach to the mental block since it has proven to be less painful for the patients than the percutaneous technique [3].