Continuing Education Activity
Melasma is a common skin problem caused by brown to gray-brown patches on the face. Most people get it on their cheeks, chin, nose bridge, forehead, and above the upper lip. It is more common in women than men. Pregnancy is a common cause of melasma. It also affects women taking oral contraceptives and hormones. This activity reviews the evaluation of melasma and highlights the role of the interprofessional team in managing patients with this condition.
Objectives:
Identify the etiology of melasma.
Describe the presentation of a patient with melasma.
Outline the treatment and management options available for melasma.
Explain interprofessional team strategies to improve care coordination and communication to advance the diagnosis of melasma and improve outcomes.
Introduction
Melasma is a common skin problem caused by brown to gray-brown patches on the face. Most people get it on their cheeks, chin, nose bridge, forehead, and above the upper lip. It is more common in women than men. Pregnancy is a common cause of melasma. It also affects women taking oral contraceptives and hormones.[1][2][3][4]
Etiology
Etiologic factors include genetic influences, ultraviolet (UV) radiation, pregnancy, hormonal therapies, cosmetics, phototoxic drugs, and antiseizure medications.
Melasma stimulates melanocytes by the female sex hormones estrogen and progesterone, producing more melanin pigments when the skin is exposed to the sun.[5][6][7]
Genetic
Genetic predisposition may be a major factor in the development of melasma.
- Melasma is more common in females than in males.
- Persons with light-brown skin types from regions of the world with high sun exposure are more prone to the development of melasma.
- Approximately 50% report a positive family history of the condition. Identical twins have been reported to develop melasma.
Sunlight Exposure
UV radiation can cause lipids peroxidation in cellular membranes, resulting in free radicals which could stimulate melanocytes to produce excess melanin.
- Sunscreens that block UV-B radiation (290-320 nm) do not block the longer wavelengths of UV-A and visible radiation (320-700 nm), which also stimulate melanocytes to produce melanin.
Hormonal Influences
Hormones may play a role in developing melasma in some individuals.
- The mask of pregnancy is known to occur in obstetric patients. The exact mechanism is unknown. Estrogen, progesterone, and melanocyte-stimulating hormone levels are normally increased during the third trimester of pregnancy and may be a factor.
- Patients with melasma who are nulliparous have no increased levels of estrogen or MSH but show elevated levels of estrogen receptors within the lesions. In addition, melasma with estrogen- and progesterone-containing oral contraceptive pills and diethylstilbestrol treatment for prostate cancer have been observed.
- A woman who is postmenopausal and given progesterone may develop melasma, while those who are given estrogen alone do not; this implicates progesterone as playing a primary role in the development of melasma.
Thyroid Disease
There is a four-fold increase in thyroid disease in melasma patients.
- There is an association between the development of melasma and the presence of melanocytic nevi and lentiginous nevi.
- This would indicate a relationship between the development of melasma and the presence of pigmentation.
Epidemiology
Persons of any race can be affected. Melasma is more common in darker skin types than in lighter skin types, and it is particularly more common in light brown skin types. Women are affected nine times more than men. Melasma is rare before puberty and more common in reproductive years. Melasma is present in 15% to 50% of pregnant patients. The prevalence varies between 1.5% and 33%, depending on the population.
Pathophysiology
The most important factor is exposure to sunlight. UV radiation induces the production of alpha-melanocyte-stimulating hormone and corticotropin, as well as interleukin 1 and endothelin 1, which contributes to increased melanin production by intraepidermal melanocytes. Prolonged UV exposure-induced dermal inflammation and fibroblast activation upregulate stem cell factors in the melasma dermis, resulting in increased melanogenesis.
Histopathology
Melanin is increased in the dermis, epidermis, or both. Epidermal melanin is located in the keratinocytes in the basal and suprabasal areas. Dermal melanin is also found in the superficial and mid-dermis within the macrophages congregating around small, dilated vessels. Inflammation is sparse or absent.
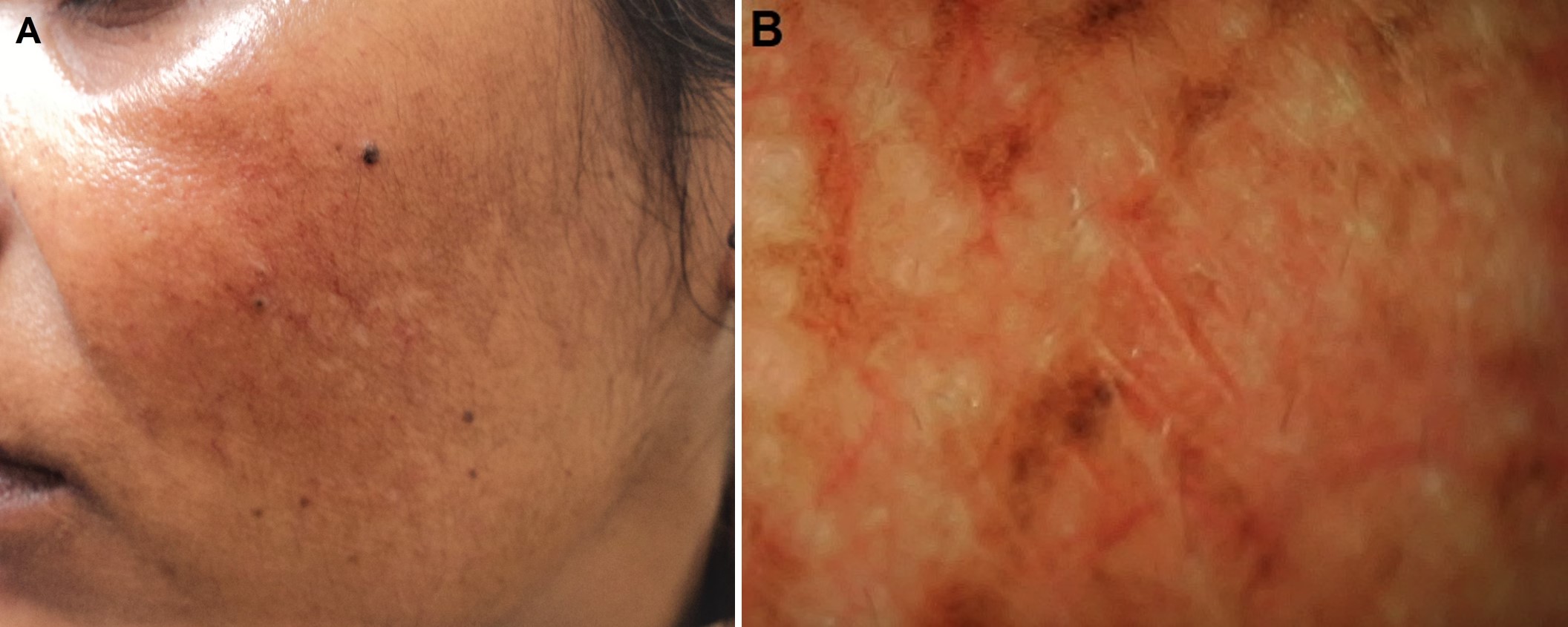
History and Physical
Melasma occurs in sun-exposed areas as an acquired hypermelanosis, presenting as symmetrically distributed hyperpigmented macules that can be confluent or punctate. It is worse in areas that receive excessive sun exposure, including the cheeks, the upper lip, the chin, and the forehead.
Evaluation
No laboratory tests are indicated, although some studies suggest mild abnormalities in thyroid function are associated, specifically pregnancy- or oral contraceptive pill-associated melasma. In these cases, it is reasonable to consider checking thyroid function tests. Wood lamp examination helps to localize the pigment to the dermis or epidermis.[8][9][10]
Treatment / Management
The best treatment is a topical combination of hydroquinone cream and avoidance of sun or estrogen exposure. In addition to the avoidance of sun exposure, discontinuing the use of high-SPF sunscreens (50 or higher) can prevent the development of melasma. First-line therapy for melasma consists of effective topical therapies, mainly in the form of triple combinations (hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01%) and when triple combinations are unavailable or when patients have hypersensitivity to them, then dual ingredients or single agents be considered.
Chemical peels and lasers may yield unpredictable results and are associated with adverse effects, including epidermal necrosis, postinflammatory hyperpigmentation, and hypertrophic scars. These interventions are second-line therapies and are used only if the topical medication has failed. In experienced hands, chemical peels and lasers are usually safe and may produce results faster than topical medications.
Skin Peels These procedures carry a risk of adverse outcomes. Peels use glycolic or salicylic acid-based compounds, which may increase the turnover of hyperpigmented keratinocytes.
- They often begin as a monthly treatment using low-concentration formulas and progress to weekly applications at higher concentrations.
- Lightening agents are usually used in conjunction with superficial peels for better results.
- Skin peels should only be used after a trial of therapy with at least one skin-lightening agent.
- Close monitoring of skin depigmentation is necessary, and therapy should be halted if alterations in pigmentation in the surrounding skin are noted.
Lasers
The efficacy of lasers for the treatment of melasma has been associated with undesired cosmetic results. Their use should be considered in cases of extensive disease that is refractory to laser use as it may actually worsen the condition.
Differential Diagnosis
The differential diagnoses include:
- Actinic lichen planus
- Acanthosis nigricans
- Discoid lupus erythematosus
- Drug-induced photosensitivity
- Exogenous ochronosis
- Frictional Melanosis
- Mastocytosis
- Nevi of Ito and Ota
- Pigmented contact dermatitis
- Poikiloderma of Civatte
- Postinflammatory hyperpigmentation
Prognosis
Melasma has no associated mortality or morbidity. No cases of malignant transformation or association with the increased risk of melanoma or other malignancies have been reported. Patients with melasma are actually considered to have less risk for melanoma.
The dermal pigment may take longer to resolve than the epidermal pigment because no effective therapy is capable of removing dermal pigment. However, treatment should not be withheld simply because of a preponderance of dermal pigment. The source of the dermal pigment is the epidermis, and if epidermal melanogenesis can be inhibited for long periods, the dermal pigment will not replenish and will slowly resolve.
Resistant cases or recurrences of melasma occur often and are certain if strict avoidance of sunlight is not rigidly heeded.
Pearls and Other Issues
Patients should avoid the routine use of cosmetics on sensitive skin. Vigorously rubbing triple creams on hyperpigmented areas may worsen the situation. Ochronosis can occur with prolonged exposure to creams with potent steroids.
Melasma should be distinguished from post-inflammatory hyperpigmentation, actinic lichen planus, and hydroquinone-induced exogenous ochronosis.
Patient education should include strict sun avoidance as this is essential for resolution and may prevent the recurrence of melasma. Melasma patients should apply bleaching creams to dark areas only. Resolution with strict sun avoidance and topical bleaching creams can take many months; patients should be educated to expect slow but gradual lightening.
Enhancing Healthcare Team Outcomes
Melasma is a benign skin disorder that has no morbidity. The key reason why some patients seek treatment is aesthetic. Fortunately, melasma resolves on its own in most cases. Thus, healthcare workers, including nurse practitioners, dermatologists, and primary care providers, should educate the patient on avoiding the sun and discontinuing the trigger medications. There are dozens of treatments for melasma and none is superior to the other. In fact, some treatments like the laser may worsen the condition.
Patients who seek no treatment and avoid the sun will notice that the rash usually disappears in a few months.[11]