Introduction
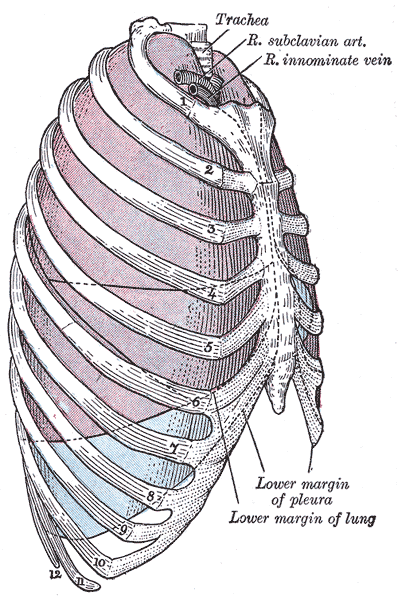
The lungs' primary function is to facilitate gas exchange. Oxygen enters the bloodstream from the environment through the alveoli. Carbon dioxide from tissue metabolism leaves the body through the lungs. The lung vasculature is organized to support these functions.[1] The lungs are shielded by the rib cage within the thoracic cavity, flanking the heart on either side. Double-layered pleural membranes cover each lung (see Image. Relationship Of Thoracic Contents And Thoracic Cage Linings). The lung parenchyma forms from the complex branching of the air passageways. The intricate neural control in the lungs ensures proper regulation of respiratory function, including airway caliber, ventilation, and protective reflexes.
Knowledge of lung anatomy is essential for understanding pulmonary disease pathophysiology, interpreting diagnostic tests, and performing surgical procedures. A deeper grasp of lung anatomy is essential for healthcare professionals diagnosing, treating, and managing respiratory conditions.
Structure and Function
Anatomy
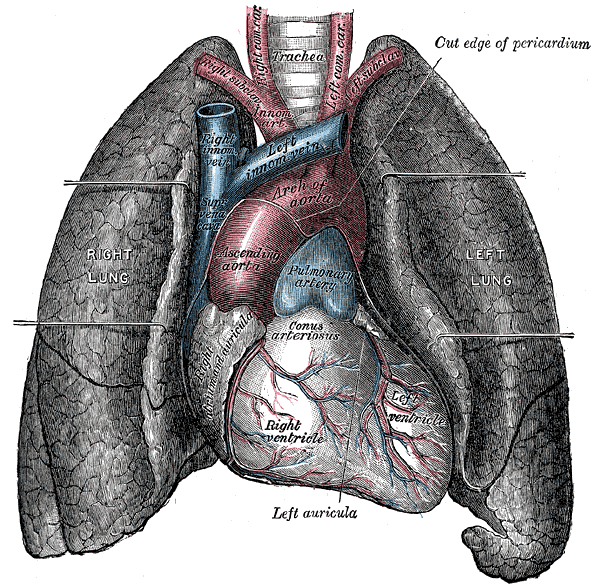
Grossly, the lungs have a spongy texture and a pinkish-gray hue. The lung has an apex, base, 3 surfaces, and 3 borders. The apex lies above the 1st rib and is covered by the cervical pleura. The base is the lung's concave inferior surface resting on the diaphragm. The lung has costal, mediastinal, and diaphragmatic surfaces. The costal surface is related to the costal pleura, sternum, and ribs. The costal surface also joins the mediastinal surface anteriorly and posteriorly and the diaphragmatic surfaces inferiorly. The mediastinal surface is on each lung's medial side, where it is related to the middle mediastinum, which contains the pericardium and heart (see Image. The Lungs and the Mediastinum). The diaphragmatic surface (base) is concave and rests on the diaphragm dome. The right dome is higher than the left because of the liver.
The 3 borders include the anterior, posterior, and inferior borders. The lung's anterior border corresponds to the pleural reflection and has a cardiac notch—a concavity accommodating the left cardiac ventricle—in the left lung. The thin inferior border separates the lung base from the costal surface. The thick posterior border extends from the C7 to T10 vertebrae, from the lung's apex to the inferior border.
The right and left lungs' structural organization is similar, though asymmetrical. The right lung is comprised of the right upper (RUL), middle (RML), and lower (RLL) lobes. The left lung consists of the left upper (LUL) and lower (LLL) lobes. Oblique and horizontal fissures separate the right lung's 3 lobes. The oblique fissure divides the RML and RLL, while the horizontal fissure divides the RUL and RML. The left lung only has an oblique fissure, separating LUL and LLL.
The lobes are further divided into segments associated with specific segmental bronchi. Segmental bronchi are the 3rd-order branches off the 2nd-order branches (lobar bronchi) that arise from the main bronchus.
The right lung consists of 10 segments. The RUL has 3 segments: apical, anterior, and posterior. The RML has medial and lateral segments, while the RLL has superior, medial, anterior, lateral, and posterior segments. The left lung has 8 to 9 segments, depending on lobar division. Generally, the LUL has 4 segments: anterior, apicoposterior, inferior, and superior lingular. The LLL has 4 or 5, but more often has lateral, anteromedial, superior, and posterior segments.
The hilum is a depressed area at the center of the lung's mediastinal surface, lying anteriorly to the 5th through 7th thoracic vertebrae. The hilum is the region where various structures forming the lung root pass to enter and exit the lung. The hilum is surrounded by the pleura, which extends inferiorly and forms a pulmonary ligament. The hilum contains the main bronchi, pulmonary vasculature, phrenic nerve, lymphatics, nodes, and bronchial vessels. From anterior to posterior, the order in the hilum is the vein, artery, and bronchus.
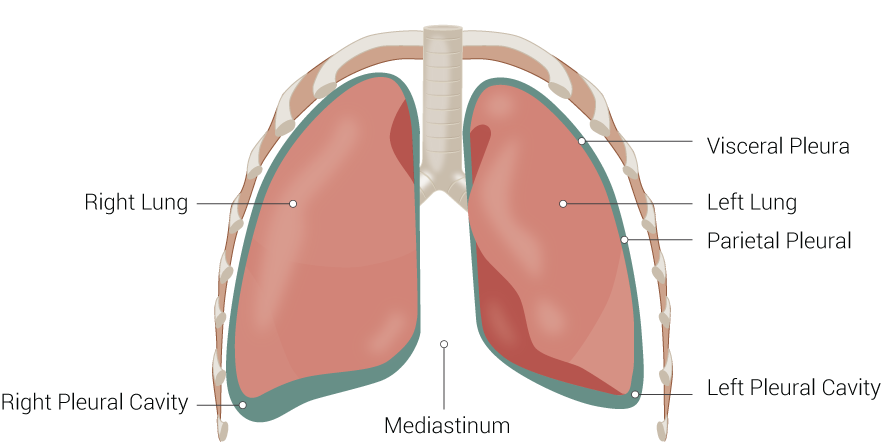
The pleural space is a thin, fluid-filled cavity located between the lungs and the chest wall's inner surface. This potential space is lined by 2 serous membrane layers: the visceral pleura, which covers the lung surfaces, and the parietal pleura, which lines the chest wall's interior surface (see Image. Lung Anatomy). These membranes secrete a small amount of pleural fluid, which lubricates the pleural surfaces and reduces friction during breathing.
Histologically, the important cells in the alveoli are the types I and II pneumocytes and alveolar macrophages. Type I pneumocytes are thin, flat cells that form most of the alveolar epithelium. Type II pneumocytes are cuboidal cells found interspersed among type I pneumocytes. Alveolar macrophages are specialized immune cells that reside within the alveoli. The blood-air barrier is a thin membrane comprised of the alveolar epithelium, capillary endothelium, and their shared basement membrane. The pores of Kohn are small openings in the alveolar walls.
Function
The lungs' chief function is to promote gas exchange, which occurs mainly in the alveoli. Some pharmacologic agents, eg, volatile anesthetics and inhaled bronchodilators, may also be metabolized and cleared in the lungs.
Type I pneumocytes are involved in gas exchange by facilitating oxygen and carbon dioxide diffusion between the alveoli and the bloodstream. Type II pneumocytes secrete pulmonary surfactant, a mixture of proteins and lipids that minimizes surface tension inside the alveoli, preventing their collapse during expiration and facilitating lung expansion during inspiration. Type II pneumocytes also serve as progenitor cells that replace injured type I cells. Alveolar macrophages phagocytose and eliminate foreign particles, pathogens, and cellular debris and are thus vital in maintaining lung homeostasis and defense against respiratory infections.
The blood-air barrier facilitates efficient pulmonary gas exchange. Oxygen diffuses from the alveolar air into the capillary blood, while carbon dioxide moves in the opposite direction. The pores of Kohn allow for collateral ventilation between adjacent alveoli. These interalveolar connections provide a pathway for air movement and distribution, particularly in cases of regional lung collapse or obstruction. Collateral ventilation helps equalize pressure within the alveoli, promoting more uniform lung inflation and improving gas exchange. The Kohn pores contribute to lung function and may play a role in maintaining respiratory efficiency, especially in conditions such as chronic obstructive pulmonary disease or pneumonia. The Kohn pores are poorly developed in young children.[2]
Diaphragm and intercostal muscle contractions facilitate respiration. In respiratory distress or failure, the sternocleidomastoid and scalene muscles act as accessory respiratory muscles. Thoracic muscle pull contributes to negative pressure in the thorax during inspiration, allowing lung expansion. Conversely, the muscles' compressive forces against the thorax assist in generating positive pressure during expiration, aiding in lung emptying.[3][4][5]
Embryology
The lower respiratory organs—the larynx, trachea, bronchi, and lungs—begin their development during the 4th week of embryonic life from a median growth of the endodermal caudal pharynx's ventral part, which later forms the laryngotracheal tube or respiratory diverticulum. The diverticulum's endodermal lining gives rise to the epithelium and glands in the larynx, trachea, bronchi, and lung alveoli. The surrounding splanchnic mesoderm forms the respiratory organs' cartilages, smooth muscles, and connective tissues. The respiratory diverticulum initially communicates with the foregut. The tracheoesophageal septum appears from the mesoderm and separates the foregut's cranial part into ventral and dorsal segments. The ventral segment gives rise to the laryngotracheal tube, which forms the trachea and lung buds. The dorsal segment forms the esophagus. The respiratory diverticulum elongates cranially to form the trachea and caudally to give rise to the right and left lung buds.
Around the 5th developmental week, the lung buds mature into bronchial buds, which expand to form the right and left main bronchi. The right main bronchus gives rise to 3 secondary or lobar bronchi, while the left main bronchus gives rise to 2. These secondary bronchi grow inferiorly and laterally into the pericardioperitoneal canals and primitive pleural cavity. With further development, the secondary bronchi form 10 tertiary or segmental bronchi in the right lung and 8 to 9 in the left, establishing the adult lungs' bronchopulmonary segments. Around the 24th week, about 17 generations of subdivisions into intrasegmental branches and respiratory bronchioles are formed. An additional 6 to 7 divisions occur during postnatal life.
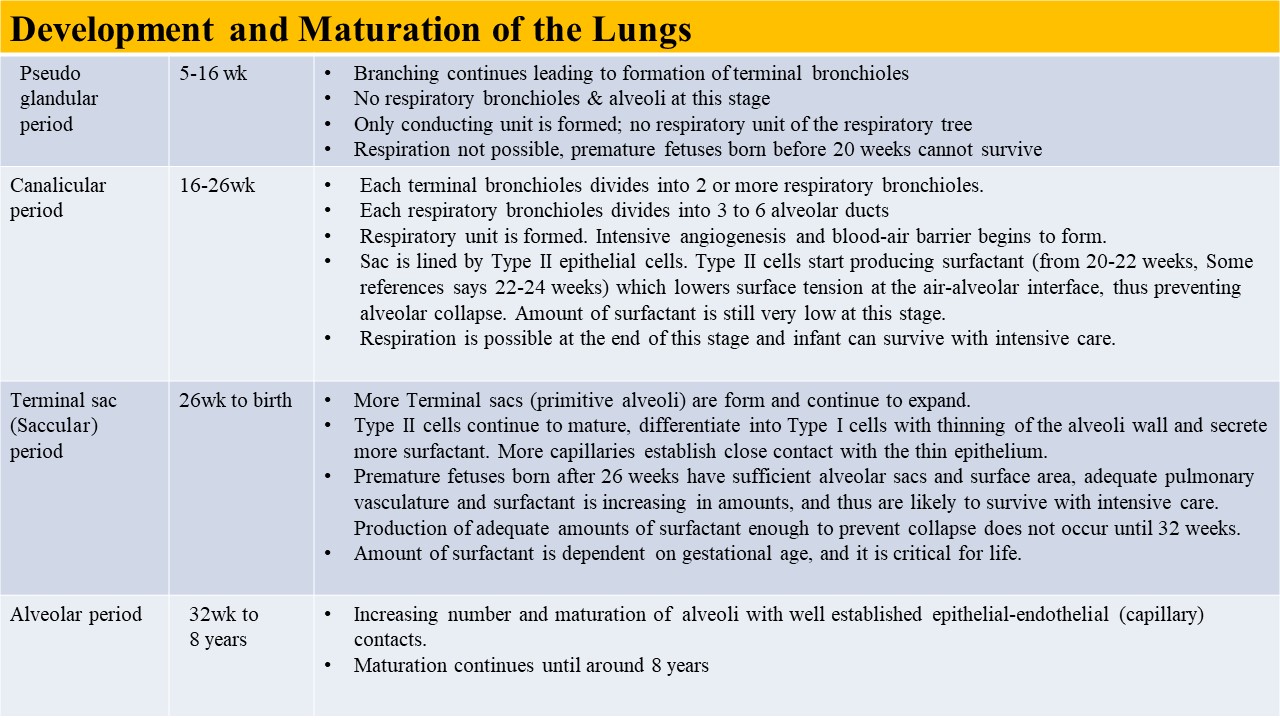
Lung development involves 4 overlapping stages: pseudoglandular, canalicular, saccular or terminal sac, and alveolar (see Image. Embryonic and Fetal Lung Development Table). The pseudoglandular stage is characterized by several branching generations of the respiratory airways, establishing the terminal bronchioles. Respiratory bronchioles or alveoli are absent during this stage. The hallmark features of the canalicular stage are the smaller respiratory bronchioles, alveolar ducts, intensive angiogenesis, blood-air barriers, and minimal surfactant production by type II pneumocytes. Fetal survival is possible when type II pneumocytes produce enough surfactant. In the terminal sac stage, more terminal sacs or primitive alveoli form, and the terminal sacs continue to expand. Type II pneumocytes continue to proliferate and mature, increasing their surfactant production. The alveolar stage involves mature alveolar formation and further surfactant production increase.[6]
The respiratory system's development is complex and coordinated, involving some signaling molecules and transcription factors. The lung bud's appearance and location depend upon the adjacent splanchnic mesoderm's retinoic acid secretion.[7] Retinoic acid elevation upregulates the transcription factor TBX4, expressed in the gut tube endoderm. TBX4 induces lung bud formation and continued growth and differentiation[8].
Blood Supply and Lymphatics
The lungs' vasculature is unique. The pulmonary artery takes deoxygenated blood from the heart to be oxygenated by the lung parenchyma. Meanwhile, the bronchial arteries provide oxygen to the lung parenchyma for survival.
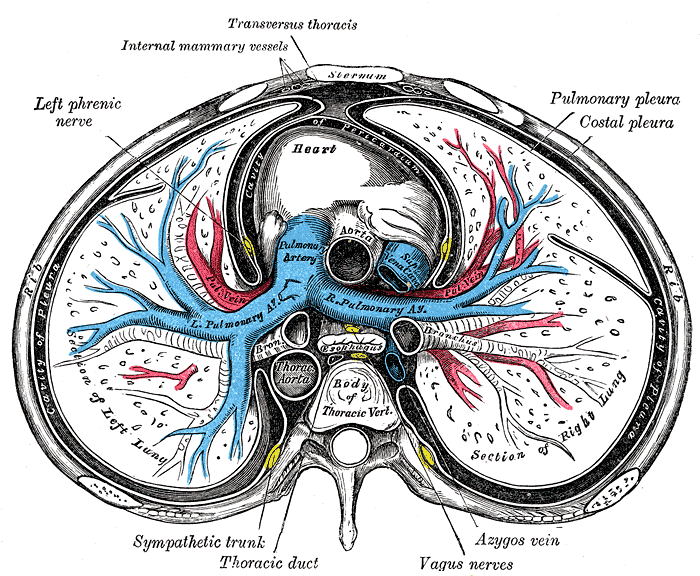
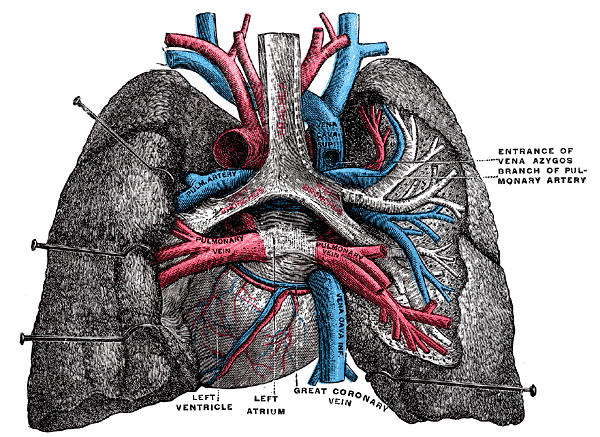
The main pulmonary artery emerges from the right ventricle and bifurcates into the left and right main pulmonary arteries (see Image. Sternum Transverse Section). The pulmonary artery branches usually trail and expand along the bronchial tree branches, eventually becoming alveolar capillaries. The pulmonary veins receive oxygenated blood from the alveolar capillaries and a small volume of deoxygenated blood from the bronchial and visceral pleural veins. This mixing slightly lowers the oxygen saturation of the blood in the pulmonary veins before it returns to the left side of the heart for systemic distribution. Four pulmonary veins come together at the left atrium (see Image. Lungs and Mediastinum, Posterior View).
Bronchial circulation is part of the systemic circulation. The left bronchial artery arises as 2 branches—superior and inferior—from the thoracic aorta. The single right bronchial artery usually comes from either the right posterior intercostal or left superior bronchial artery or directly from the aorta. The bronchial veins collect the deoxygenated blood and empty into the azygos vein.
The superficial and deep lymphatic plexuses drain the lungs. Lung parenchymal lymph first drains into the intraparenchymal nodes and then to the peribronchial nodes. The lymphatics then drain to the tracheobronchial and paratracheal lymph nodes, the bronchomediastinal trunk, and into the thoracic duct.
Nerves
The lung receives innervation from 2 main sources: the pulmonary plexus, which consists of parasympathetic and sympathetic innervation, and the phrenic nerve. The pulmonary plexus surrounds the lung tissue, pulmonary vasculature, and bronchi. Vagal nerve branches within the plexus provide parasympathetic stimulation, while sympathetic trunk branches supply sympathetic innervation. Parasympathetic impulses produce bronchoconstriction, pulmonary vessel dilation, and increased gland secretion. Sympathetic firing causes bronchodilation, pulmonary vessel constriction, and decreased gland secretion. The phrenic nerve comes from the C3 to C5 nerve roots, supplying the fibrous pericardium, portions of the visceral pleura, and the diaphragm.
Physiologic Variants
Accessory fissures, which may be superficial or deep at the hilum, may occur in some variants. These fissures may cause odd imaging patterns when evaluating pulmonary disease. Other variations include agenesis (the absence of one or both lungs), aplasia (rudimentary lung), or accessory lobes. These variants may also produce imaging anomalies.[9]
Surgical Considerations
A lobectomy is the removal of an entire lung lobe, while a segmentectomy is the excision of a lung segment. Lobectomies may be necessary to prevent the spread of a disease affecting an entire lobe. Lung conditions on which lobectomies may be performed include tuberculosis, lung abscess, emphysema, benign tumor, and lung cancer. A segmentectomy may be performed on benign segment masses to preserve the lung. Other conditions that may be treated with a segmentectomy include bronchiectasis, early-stage cancer, lung nodules, and tuberculosis.[10][11][12]
Saddle pulmonary embolism involves pulmonary trunk bifurcation obstruction. This condition is a surgical emergency requiring an embolectomy[13].
Clinical Significance
Different thoracic conditions produce physical examination abnormalities. For example, the chest is ordinarily resonant on percussion, but fluid accumulation can make it dull.[14] Wheezing on auscultation is often due to bronchoconstriction, as in asthma exacerbation, but it may also manifest in patients with congestive heart failure. Crackles or rales result from pulmonary edema, which may arise from diseases like congestive heart failure, interstitial lung disease, and pneumonia. Rhonchi are often due to secretions in the larger airways, causing an obstruction, as in chronic bronchitis and cystic fibrosis.
The lungs are black on x-rays because air is translucent. Asking the patient to inhale optimizes lung visualization, though optimization is usually impossible in patients with altered sensorium or severe respiratory distress.
Thoracentesis is a medical procedure that uses a needle to draw fluid out from the pleural cavity. This procedure may be therapeutic or diagnostic. Thoracentesis can relieve chest pain or shortness of breath arising from pleural space pathology. Diagnostic thoracentesis helps determine the cause of pleural effusion to guide definitive treatment.[15]
Pneumonia is lung infection and inflammation that may cause pleural effusion. Patients may present with fever, cough, chest pain, nausea, and vomiting.