[1]
Toueg CW, Mac-Thiong JM, Grimard G, Parent S, Poitras B, Labelle H. Prevalence of spondylolisthesis in a population of gymnasts. Studies in health technology and informatics. 2010:158():132-7
[PubMed PMID: 20543413]
[3]
Bydon M, Alvi MA, Goyal A. Degenerative Lumbar Spondylolisthesis: Definition, Natural History, Conservative Management, and Surgical Treatment. Neurosurgery clinics of North America. 2019 Jul:30(3):299-304. doi: 10.1016/j.nec.2019.02.003. Epub
[PubMed PMID: 31078230]
[4]
Wiltse LL, Newman PH, Macnab I. Classification of spondylolisis and spondylolisthesis. Clinical orthopaedics and related research. 1976 Jun:(117):23-9
[PubMed PMID: 1277669]
[5]
Beutler WJ, Fredrickson BE, Murtland A, Sweeney CA, Grant WD, Baker D. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine. 2003 May 15:28(10):1027-35; discussion 1035
[PubMed PMID: 12768144]
[6]
DeWald CJ, Vartabedian JE, Rodts MF, Hammerberg KW. Evaluation and management of high-grade spondylolisthesis in adults. Spine. 2005 Mar 15:30(6 Suppl):S49-59
[PubMed PMID: 15767887]
[7]
McCleary MD, Congeni JA. Current concepts in the diagnosis and treatment of spondylolysis in young athletes. Current sports medicine reports. 2007 Jan:6(1):62-6
[PubMed PMID: 17212915]
[8]
NATHAN H. Spondylolysis; its anatomy and mechanism of development. The Journal of bone and joint surgery. American volume. 1959 Mar:41-A(2):303-20
[PubMed PMID: 13630966]
[9]
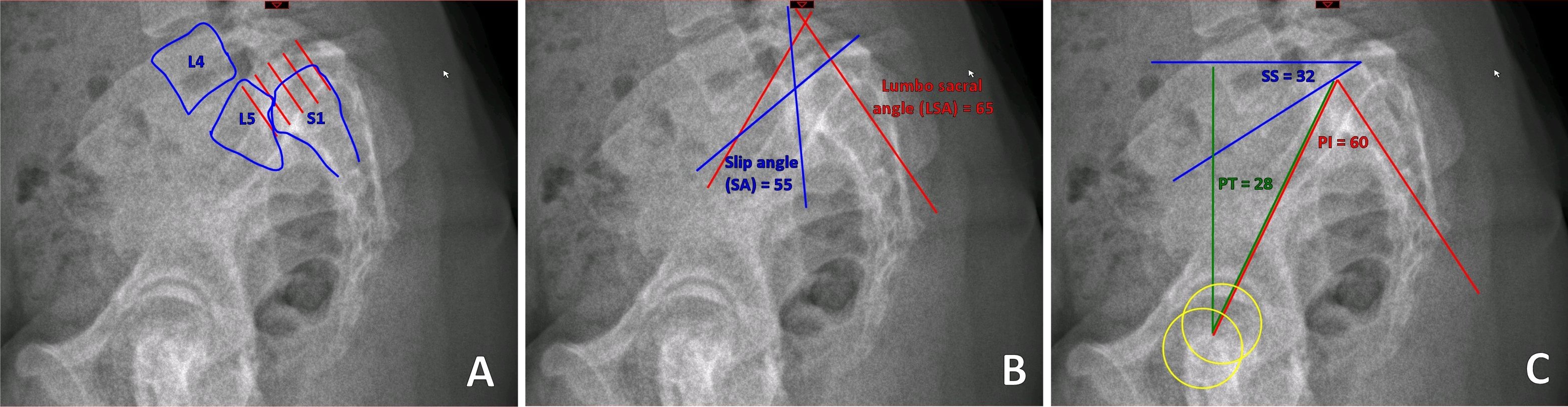
Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O'Brien M. The importance of spino-pelvic balance in L5-s1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine. 2005 Mar 15:30(6 Suppl):S27-34
[PubMed PMID: 15767882]
[10]
Sairyo K, Nagamachi A, Matsuura T, Higashino K, Sakai T, Suzue N, Hamada D, Takata Y, Goto T, Nishisho T, Goda Y, Tsutsui T, Tonogai I, Miyagi R, Abe M, Morimoto M, Mineta K, Kimura T, Nitta A, Higuchi T, Hama S, Jha SC, Takahashi R, Fukuta S. A review of the pathomechanism of forward slippage in pediatric spondylolysis: the Tokushima theory of growth plate slippage. The journal of medical investigation : JMI. 2015:62(1-2):11-8. doi: 10.2152/jmi.62.11. Epub
[PubMed PMID: 25817277]
[11]
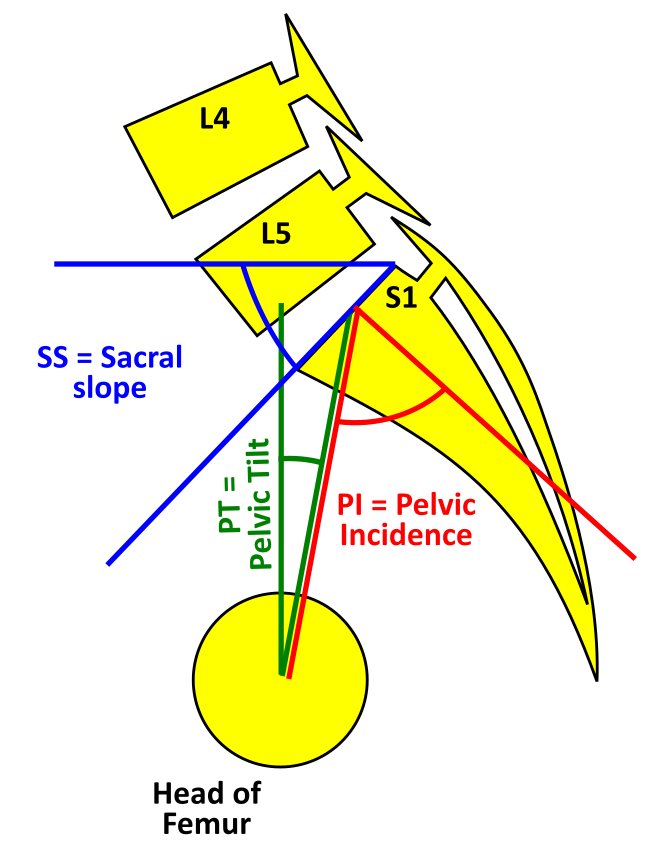
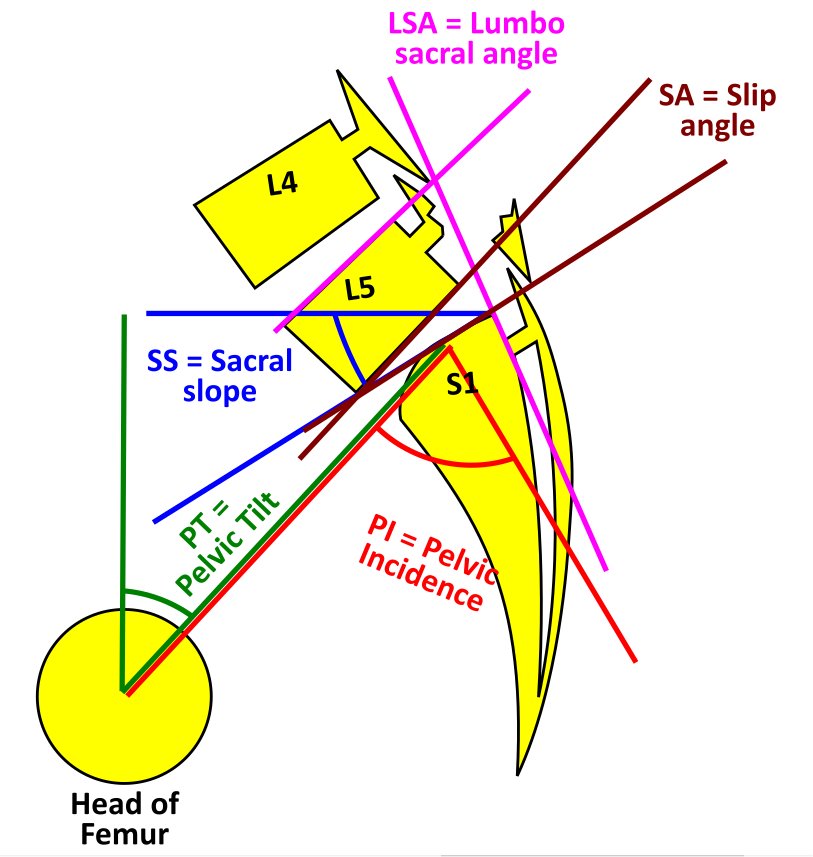
Tebet MA. Current concepts on the sagittal balance and classification of spondylolysis and spondylolisthesis. Revista brasileira de ortopedia. 2014 Jan-Feb:49(1):3-12. doi: 10.1016/j.rboe.2014.02.003. Epub 2014 Feb 18
[PubMed PMID: 26229765]
[12]
Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine. 2002 Sep 15:27(18):2026-9
[PubMed PMID: 12634563]
[13]
Boxall D, Bradford DS, Winter RB, Moe JH. Management of severe spondylolisthesis in children and adolescents. The Journal of bone and joint surgery. American volume. 1979 Jun:61(4):479-95
[PubMed PMID: 438234]
[14]
Dubousset J. Treatment of spondylolysis and spondylolisthesis in children and adolescents. Clinical orthopaedics and related research. 1997 Apr:(337):77-85
[PubMed PMID: 9137179]
[15]
Alvi MA, Sebai A, Yolcu Y, Wahood W, Elder BD, Kaufmann T, Bydon M. Assessing the Differences in Measurement of Degree of Spondylolisthesis Between Supine MRI and Erect X-Ray: An Institutional Analysis of 255 Cases. Operative neurosurgery (Hagerstown, Md.). 2020 Apr 1:18(4):438-443. doi: 10.1093/ons/opz180. Epub
[PubMed PMID: 31381804]
Level 3 (low-level) evidence
[16]
Rush JK, Astur N, Scott S, Kelly DM, Sawyer JR, Warner WC Jr. Use of magnetic resonance imaging in the evaluation of spondylolysis. Journal of pediatric orthopedics. 2015 Apr-May:35(3):271-5. doi: 10.1097/BPO.0000000000000244. Epub
[PubMed PMID: 24978120]
[17]
Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2011 Sep:20 Suppl 5(Suppl 5):641-6. doi: 10.1007/s00586-011-1932-1. Epub 2011 Aug 2
[PubMed PMID: 21809015]
[18]
Steiner ME, Micheli LJ. Treatment of symptomatic spondylolysis and spondylolisthesis with the modified Boston brace. Spine. 1985 Dec:10(10):937-43
[PubMed PMID: 3914087]
[19]
Tawfik S, Phan K, Mobbs RJ, Rao PJ. The Incidence of Pars Interarticularis Defects in Athletes. Global spine journal. 2020 Feb:10(1):89-101. doi: 10.1177/2192568218823695. Epub 2019 Feb 24
[PubMed PMID: 32002353]
[20]
O'Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997 Dec 15:22(24):2959-67
[PubMed PMID: 9431633]
[21]
Sinaki M, Lutness MP, Ilstrup DM, Chu CP, Gramse RR. Lumbar spondylolisthesis: retrospective comparison and three-year follow-up of two conservative treatment programs. Archives of physical medicine and rehabilitation. 1989 Aug:70(8):594-8
[PubMed PMID: 2527488]
Level 2 (mid-level) evidence
[22]
Kraiwattanapong C, Wechmongkolgorn S, Chatriyanuyok B, Woratanarat P, Udomsubpayakul U, Chanplakorn P, Keorochana G, Wajanavisit W. Outcomes of fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar spondylolisthesis patients. Asian spine journal. 2014 Apr:8(2):119-28. doi: 10.4184/asj.2014.8.2.119. Epub 2014 Apr 8
[PubMed PMID: 24761192]
[23]
Karsy M, Bisson EF. Surgical Versus Nonsurgical Treatment of Lumbar Spondylolisthesis. Neurosurgery clinics of North America. 2019 Jul:30(3):333-340. doi: 10.1016/j.nec.2019.02.007. Epub 2019 Apr 19
[PubMed PMID: 31078234]
[24]
Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. The Journal of bone and joint surgery. British volume. 1970 Aug:52(3):432-7
[PubMed PMID: 4916960]
[25]
Tokuhashi Y, Matsuzaki H. Repair of defects in spondylolysis by segmental pedicular screw hook fixation. A preliminary report. Spine. 1996 Sep 1:21(17):2041-5
[PubMed PMID: 8883209]
[26]
Möller H, Hedlund R. Instrumented and noninstrumented posterolateral fusion in adult spondylolisthesis--a prospective randomized study: part 2. Spine. 2000 Jul 1:25(13):1716-21
[PubMed PMID: 10870149]
Level 1 (high-level) evidence
[27]
Arts M, Pondaag W, Peul W, Thomeer R. Nerve root decompression without fusion in spondylolytic spondylolisthesis: long-term results of Gill's procedure. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2006 Oct:15(10):1455-63
[PubMed PMID: 16676154]
[28]
Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. Instructional course lectures. 2008:57():431-45
[PubMed PMID: 18399601]
[29]
Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. The spine journal : official journal of the North American Spine Society. 2006 Jul-Aug:6(4):435-43
[PubMed PMID: 16825052]
[30]
Gaines RW, Nichols WK. Treatment of spondyloptosis by two stage L5 vertebrectomy and reduction of L4 onto S1. Spine. 1985 Sep:10(7):680-6
[PubMed PMID: 4071276]
[31]
Min K, Liebscher T, Rothenfluh D. Sacral dome resection and single-stage posterior reduction in the treatment of high-grade high dysplastic spondylolisthesis in adolescents and young adults. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012 Aug:21 Suppl 6(Suppl 6):S785-91. doi: 10.1007/s00586-011-1949-5. Epub 2011 Jul 29
[PubMed PMID: 21800032]
[32]
Schulte TL, Ringel F, Quante M, Eicker SO, Muche-Borowski C, Kothe R. Surgery for adult spondylolisthesis: a systematic review of the evidence. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2016 Aug:25(8):2359-67. doi: 10.1007/s00586-015-4177-6. Epub 2015 Sep 12
[PubMed PMID: 26363561]
Level 1 (high-level) evidence
[33]
Resnick DK, Watters WC 3rd, Sharan A, Mummaneni PV, Dailey AT, Wang JC, Choudhri TF, Eck J, Ghogawala Z, Groff MW, Dhall SS, Kaiser MG. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 9: lumbar fusion for stenosis with spondylolisthesis. Journal of neurosurgery. Spine. 2014 Jul:21(1):54-61. doi: 10.3171/2014.4.SPINE14274. Epub
[PubMed PMID: 24980586]
[34]
Parker SL, Mendenhall SK, Shau DN, Zuckerman SL, Godil SS, Cheng JS, McGirt MJ. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World neurosurgery. 2014 Jul-Aug:82(1-2):230-8. doi: 10.1016/j.wneu.2013.01.041. Epub 2013 Jan 12
[PubMed PMID: 23321379]
Level 2 (mid-level) evidence
[35]
Petraco DM, Spivak JM, Cappadona JG, Kummer FJ, Neuwirth MG. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine. 1996 May 15:21(10):1133-8; discussion 1139
[PubMed PMID: 8727186]
[36]
Cho KT, Lee HJ. Prone position-related meralgia paresthetica after lumbar spinal surgery : a case report and review of the literature. Journal of Korean Neurosurgical Society. 2008 Dec:44(6):392-5. doi: 10.3340/jkns.2008.44.6.392. Epub 2008 Dec 31
[PubMed PMID: 19137086]
Level 3 (low-level) evidence