[1]
Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, Tsang TS. Left atrial size: physiologic determinants and clinical applications. Journal of the American College of Cardiology. 2006 Jun 20:47(12):2357-63
[PubMed PMID: 16781359]
[2]
Cuspidi C, Negri F, Sala C, Valerio C, Mancia G. Association of left atrial enlargement with left ventricular hypertrophy and diastolic dysfunction: a tissue Doppler study in echocardiographic practice. Blood pressure. 2012 Feb:21(1):24-30. doi: 10.3109/08037051.2011.618262. Epub 2011 Oct 13
[PubMed PMID: 21992028]
[3]
Cuspidi C, Rescaldani M, Sala C. Prevalence of echocardiographic left-atrial enlargement in hypertension: a systematic review of recent clinical studies. American journal of hypertension. 2013 Apr:26(4):456-64. doi: 10.1093/ajh/hpt001. Epub 2013 Feb 6
[PubMed PMID: 23388831]
Level 1 (high-level) evidence
[4]
Patel DA, Lavie CJ, Milani RV, Shah S, Gilliland Y. Clinical implications of left atrial enlargement: a review. Ochsner journal. 2009 Winter:9(4):191-6
[PubMed PMID: 21603443]
[5]
Kizer JR, Bella JN, Palmieri V, Liu JE, Best LG, Lee ET, Roman MJ, Devereux RB. Left atrial diameter as an independent predictor of first clinical cardiovascular events in middle-aged and elderly adults: the Strong Heart Study (SHS). American heart journal. 2006 Feb:151(2):412-8
[PubMed PMID: 16442908]
[6]
Rusinaru D, Bohbot Y, Kowalski C, Ringle A, Maréchaux S, Tribouilloy C. Left Atrial Volume and Mortality in Patients With Aortic Stenosis. Journal of the American Heart Association. 2017 Oct 31:6(11):. doi: 10.1161/JAHA.117.006615. Epub 2017 Oct 31
[PubMed PMID: 29089338]
[7]
Thomas L, Muraru D, Popescu BA, Sitges M, Rosca M, Pedrizzetti G, Henein MY, Donal E, Badano LP. Evaluation of Left Atrial Size and Function: Relevance for Clinical Practice. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2020 Aug:33(8):934-952. doi: 10.1016/j.echo.2020.03.021. Epub
[PubMed PMID: 32762920]
[8]
Stritzke J, Markus MR, Duderstadt S, Lieb W, Luchner A, Döring A, Keil U, Hense HW, Schunkert H, MONICA/KORA Investigators. The aging process of the heart: obesity is the main risk factor for left atrial enlargement during aging the MONICA/KORA (monitoring of trends and determinations in cardiovascular disease/cooperative research in the region of Augsburg) study. Journal of the American College of Cardiology. 2009 Nov 17:54(21):1982-9. doi: 10.1016/j.jacc.2009.07.034. Epub
[PubMed PMID: 19909880]
[9]
Pińska M, Sorysz D, Frączek-Jucha M, Kruszec P, Róg B, Myć J, Krawczyk-Ożóg A, Sobień B, Stopyra-Pach K, Sarnecka A, Stąpór M, Olszanecka A, Golińska-Grzybała K, Nessler J, Gackowski A. The Prognostic Significance of Atrial Fibrillation and Left Atrium Size in Patients with Aortic Stenosis. Kardiologiia. 2023 Dec 27:63(12):66-71. doi: 10.18087/cardio.2023.12.n2608. Epub 2023 Dec 27
[PubMed PMID: 38156492]
[10]
Cioffi G, Stefenelli C. Comparison of left ventricular geometry and left atrial size and function in patients with aortic stenosis versus those with pure aortic regurgitation. The American journal of cardiology. 2002 Sep 15:90(6):601-6
[PubMed PMID: 12231084]
[11]
Hanif W, Alex L, Su Y, Shinde AV, Russo I, Li N, Frangogiannis NG. Left atrial remodeling, hypertrophy, and fibrosis in mouse models of heart failure. Cardiovascular pathology : the official journal of the Society for Cardiovascular Pathology. 2017 Sep-Oct:30():27-37. doi: 10.1016/j.carpath.2017.06.003. Epub 2017 Jun 21
[PubMed PMID: 28759817]
[12]
COHEN AI, McINTOSH HD, ORGAIN ES. The mimetic nature of left atrial myxomas. Report of a case presenting as a severe systemic illness and simulating massive mitral insufficiency at cardiac catheterization. The American journal of cardiology. 1963 Jun:11():802-7
[PubMed PMID: 14021991]
Level 3 (low-level) evidence
[13]
Padalino MA, Basso C, Moreolo GS, Thiene G, Stellin G. Left atrial myxoma in a child: case report and review of the literature. Cardiovascular pathology : the official journal of the Society for Cardiovascular Pathology. 2003 Jul-Aug:12(4):233-6
[PubMed PMID: 12826294]
Level 3 (low-level) evidence
[14]
Iwashima Y, Horio T, Takami Y, Inenaga T, Nishikimi T, Takishita S, Kawano Y. Effects of the creation of arteriovenous fistula for hemodialysis on cardiac function and natriuretic peptide levels in CRF. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2002 Nov:40(5):974-82
[PubMed PMID: 12407642]
[15]
Aoyagi S, Tobinaga S, Saisho H. Enlargement of the Excluded Left Atrial Appendage With Thrombus. International heart journal. 2017 Feb 7:58(1):144-146. doi: 10.1536/ihj.16-113. Epub 2017 Jan 11
[PubMed PMID: 28077818]
[16]
Bombelli M, Cuspidi C, Facchetti R, Sala C, Tadic M, Brambilla G, Re A, Villa P, Grassi G, Mancia G. New-onset left atrial enlargement in a general population. Journal of hypertension. 2016 Sep:34(9):1838-45. doi: 10.1097/HJH.0000000000001022. Epub
[PubMed PMID: 27379539]
[17]
Ou Q, Chen Y, Yu S, Guo X, Zhao H, Sun Y. Prevalence of left atrial enlargement and its risk factors in general Chinese population. BMC cardiovascular disorders. 2016 Mar 5:16():53. doi: 10.1186/s12872-016-0229-z. Epub 2016 Mar 5
[PubMed PMID: 26944401]
[18]
Pelliccia A, Maron BJ, Di Paolo FM, Biffi A, Quattrini FM, Pisicchio C, Roselli A, Caselli S, Culasso F. Prevalence and clinical significance of left atrial remodeling in competitive athletes. Journal of the American College of Cardiology. 2005 Aug 16:46(4):690-6
[PubMed PMID: 16098437]
Level 3 (low-level) evidence
[19]
Pape LA, Price JM, Alpert JS, Ockene IS, Weiner BH. Relation of left atrial size to pulmonary capillary wedge pressure in severe mitral regurgitation. Cardiology. 1991:78(4):297-303
[PubMed PMID: 1889048]
[20]
Appleton CP, Galloway JM, Gonzalez MS, Gaballa M, Basnight MA. Estimation of left ventricular filling pressures using two-dimensional and Doppler echocardiography in adult patients with cardiac disease. Additional value of analyzing left atrial size, left atrial ejection fraction and the difference in duration of pulmonary venous and mitral flow velocity at atrial contraction. Journal of the American College of Cardiology. 1993 Dec:22(7):1972-82
[PubMed PMID: 8245357]
[21]
Aljizeeri A, Gin K, Barnes ME, Lee PK, Nair P, Jue J, Tsang TS. Atrial remodeling in newly diagnosed drug-naive hypertensive subjects. Echocardiography (Mount Kisco, N.Y.). 2013 Jul:30(6):627-33. doi: 10.1111/echo.12119. Epub 2013 Jan 30
[PubMed PMID: 23360480]
[22]
Vaziri SM, Larson MG, Benjamin EJ, Levy D. Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation. 1994 Feb:89(2):724-30
[PubMed PMID: 8313561]
[23]
Tsang TS, Barnes ME, Bailey KR, Leibson CL, Montgomery SC, Takemoto Y, Diamond PM, Marra MA, Gersh BJ, Wiebers DO, Petty GW, Seward JB. Left atrial volume: important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clinic proceedings. 2001 May:76(5):467-75
[PubMed PMID: 11357793]
[24]
Ahlberg G, Andreasen L, Ghouse J, Bertelsen L, Bundgaard H, Haunsø S, Svendsen JH, Olesen MS. Genome-wide association study identifies 18 novel loci associated with left atrial volume and function. European heart journal. 2021 Nov 21:42(44):4523-4534. doi: 10.1093/eurheartj/ehab466. Epub
[PubMed PMID: 34338756]
[25]
Barger PM, Kelly DP. Fatty acid utilization in the hypertrophied and failing heart: molecular regulatory mechanisms. The American journal of the medical sciences. 1999 Jul:318(1):36-42
[PubMed PMID: 10408759]
[26]
Verheule S, Sato T, Everett T 4th, Engle SK, Otten D, Rubart-von der Lohe M, Nakajima HO, Nakajima H, Field LJ, Olgin JE. Increased vulnerability to atrial fibrillation in transgenic mice with selective atrial fibrosis caused by overexpression of TGF-beta1. Circulation research. 2004 Jun 11:94(11):1458-65
[PubMed PMID: 15117823]
[27]
Chung MK, Martin DO, Sprecher D, Wazni O, Kanderian A, Carnes CA, Bauer JA, Tchou PJ, Niebauer MJ, Natale A, Van Wagoner DR. C-reactive protein elevation in patients with atrial arrhythmias: inflammatory mechanisms and persistence of atrial fibrillation. Circulation. 2001 Dec 11:104(24):2886-91
[PubMed PMID: 11739301]
[28]
Psychari SN, Apostolou TS, Sinos L, Hamodraka E, Liakos G, Kremastinos DT. Relation of elevated C-reactive protein and interleukin-6 levels to left atrial size and duration of episodes in patients with atrial fibrillation. The American journal of cardiology. 2005 Mar 15:95(6):764-7
[PubMed PMID: 15757607]
[29]
Kallergis EM, Manios EG, Kanoupakis EM, Mavrakis HE, Arfanakis DA, Maliaraki NE, Lathourakis CE, Chlouverakis GI, Vardas PE. Extracellular matrix alterations in patients with paroxysmal and persistent atrial fibrillation: biochemical assessment of collagen type-I turnover. Journal of the American College of Cardiology. 2008 Jul 15:52(3):211-5. doi: 10.1016/j.jacc.2008.03.045. Epub
[PubMed PMID: 18617070]
[30]
Chahine Y, Chamoun N, Kassar A, Bockus L, Macheret F, Akoum N. Atrial fibrillation substrate and impaired left atrial function: a cardiac MRI study. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2024 Nov 1:26(11):. doi: 10.1093/europace/euae258. Epub
[PubMed PMID: 39523754]
[31]
Lu S, Liu H, Sun J, Zhang J, Li L, Tang Q, Liu Y, Deng Y. Evaluation of left atrial and ventricular remodeling in atrial fibrillation subtype by using speckle tracking echocardiography. Frontiers in cardiovascular medicine. 2023:10():1208577. doi: 10.3389/fcvm.2023.1208577. Epub 2023 Aug 10
[PubMed PMID: 37636311]
[32]
Casaclang-Verzosa G, Gersh BJ, Tsang TS. Structural and functional remodeling of the left atrium: clinical and therapeutic implications for atrial fibrillation. Journal of the American College of Cardiology. 2008 Jan 1:51(1):1-11. doi: 10.1016/j.jacc.2007.09.026. Epub
[PubMed PMID: 18174029]
[33]
Cha TJ, Ehrlich JR, Chartier D, Qi XY, Xiao L, Nattel S. Kir3-based inward rectifier potassium current: potential role in atrial tachycardia remodeling effects on atrial repolarization and arrhythmias. Circulation. 2006 Apr 11:113(14):1730-7
[PubMed PMID: 16585394]
Level 2 (mid-level) evidence
[34]
Kumagai K, Nakashima H, Urata H, Gondo N, Arakawa K, Saku K. Effects of angiotensin II type 1 receptor antagonist on electrical and structural remodeling in atrial fibrillation. Journal of the American College of Cardiology. 2003 Jun 18:41(12):2197-204
[PubMed PMID: 12821247]
[35]
Kokubu N, Yuda S, Tsuchihashi K, Hashimoto A, Nakata T, Miura T, Ura N, Nagao K, Tsuzuki M, Wakabayashi C, Shimamoto K. Noninvasive assessment of left atrial function by strain rate imaging in patients with hypertension: a possible beneficial effect of renin-angiotensin system inhibition on left atrial function. Hypertension research : official journal of the Japanese Society of Hypertension. 2007 Jan:30(1):13-21
[PubMed PMID: 17460367]
[36]
Gard EK, Beale AL, Telles F, Silvestry FE, Hanff T, Hummel SL, Litwin SE, Petrie MC, Shah SJ, Borlaug BA, Burkhoff D, Komtebedde J, Kaye DM, Nanayakkara S. Left atrial enlargement is associated with pulmonary vascular disease in heart failure with preserved ejection fraction. European journal of heart failure. 2023 Jun:25(6):806-814. doi: 10.1002/ejhf.2805. Epub 2023 Mar 15
[PubMed PMID: 36847073]
[37]
Hoit BD. Left atrial size and function: role in prognosis. Journal of the American College of Cardiology. 2014 Feb 18:63(6):493-505. doi: 10.1016/j.jacc.2013.10.055. Epub 2013 Nov 27
[PubMed PMID: 24291276]
[38]
To AC, Flamm SD, Marwick TH, Klein AL. Clinical utility of multimodality LA imaging: assessment of size, function, and structure. JACC. Cardiovascular imaging. 2011 Jul:4(7):788-98. doi: 10.1016/j.jcmg.2011.02.018. Epub
[PubMed PMID: 21757171]
[39]
Kircher B, Abbott JA, Pau S, Gould RG, Himelman RB, Higgins CB, Lipton MJ, Schiller NB. Left atrial volume determination by biplane two-dimensional echocardiography: validation by cine computed tomography. American heart journal. 1991 Mar:121(3 Pt 1):864-71
[PubMed PMID: 2000754]
Level 1 (high-level) evidence
[40]
Hirata T, Wolfe SB, Popp RL, Helmen CH, Feigenbaum H. Estimation of left atrial size using ultrasound. American heart journal. 1969 Jul:78(1):43-52
[PubMed PMID: 5794795]
[41]
Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978 Dec:58(6):1072-83
[PubMed PMID: 709763]
Level 3 (low-level) evidence
[42]
Vasan RS, Larson MG, Levy D, Evans JC, Benjamin EJ. Distribution and categorization of echocardiographic measurements in relation to reference limits: the Framingham Heart Study: formulation of a height- and sex-specific classification and its prospective validation. Circulation. 1997 Sep 16:96(6):1863-73
[PubMed PMID: 9323074]
Level 1 (high-level) evidence
[43]
Tsang TS, Abhayaratna WP, Barnes ME, Miyasaka Y, Gersh BJ, Bailey KR, Cha SS, Seward JB. Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? Journal of the American College of Cardiology. 2006 Mar 7:47(5):1018-23
[PubMed PMID: 16516087]
[44]
Takeuchi M, Kitano T, Nabeshima Y, Otsuji Y, Otani K. Left ventricular and left atrial volume ratio assessed by three-dimensional echocardiography: Novel indices for evaluating age-related change in left heart chamber size. Physiological reports. 2019 Dec:7(23):e14300. doi: 10.14814/phy2.14300. Epub
[PubMed PMID: 31814325]
[45]
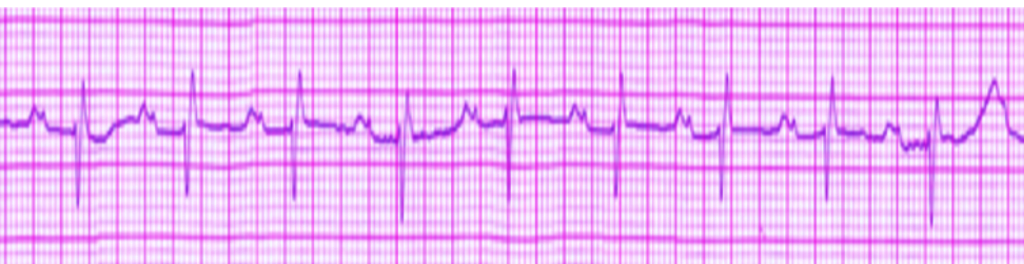
Hazen MS, Marwick TH, Underwood DA. Diagnostic accuracy of the resting electrocardiogram in detection and estimation of left atrial enlargement: an echocardiographic correlation in 551 patients. American heart journal. 1991 Sep:122(3 Pt 1):823-8
[PubMed PMID: 1831587]
[46]
Munuswamy K, Alpert MA, Martin RH, Whiting RB, Mechlin NJ. Sensitivity and specificity of commonly used electrocardiographic criteria for left atrial enlargement determined by M-mode echocardiography. The American journal of cardiology. 1984 Mar 1:53(6):829-32
[PubMed PMID: 6230922]
[47]
Waggoner AD, Adyanthaya AV, Quinones MA, Alexander JK. Left atrial enlargement. Echocardiographic assessment of electrocardiographic criteria. Circulation. 1976 Oct:54(4):553-7
[PubMed PMID: 134852]
[48]
Ikram H, Drysdale P, Bones PJ, Chan W. The non-invasive recognition of left atrial enlargement: comparison of electro- and echocardiographic measurements. Postgraduate medical journal. 1977 Jul:53(621):356-9
[PubMed PMID: 142246]
[49]
Almufleh A, Marbach J, Chih S, Stadnick E, Davies R, Liu P, Mielniczuk L. Ejection fraction improvement and reverse remodeling achieved with Sacubitril/Valsartan in heart failure with reduced ejection fraction patients. American journal of cardiovascular disease. 2017:7(6):108-113
[PubMed PMID: 29348971]
[50]
Oparil S, Schmieder RE. New approaches in the treatment of hypertension. Circulation research. 2015 Mar 13:116(6):1074-95. doi: 10.1161/CIRCRESAHA.116.303603. Epub
[PubMed PMID: 25767291]
[51]
Elbadawi A, Olorunfemi O, Ogunbayo GO, Saad M, Elgendy IY, Arif Z, Badran H, Saheed D, Ahmed HMA, Rao M. Cardiovascular Outcomes With Surgical Left Atrial Appendage Exclusion in Patients With Atrial Fibrillation Who Underwent Valvular Heart Surgery (from the National Inpatient Sample Database). The American journal of cardiology. 2017 Jun 15:119(12):2056-2060. doi: 10.1016/j.amjcard.2017.03.037. Epub 2017 Mar 29
[PubMed PMID: 28438308]
[52]
Waterford SD. Left Atrial Appendage Exclusion in Patients Without Atrial Fibrillation Undergoing Cardiac Surgery. Innovations (Philadelphia, Pa.). 2022 Nov-Dec:17(6):461-462. doi: 10.1177/15569845221146109. Epub 2022 Dec 26
[PubMed PMID: 36571261]
[53]
Bombelli M, Facchetti R, Cuspidi C, Villa P, Dozio D, Brambilla G, Grassi G, Mancia G. Prognostic significance of left atrial enlargement in a general population: results of the PAMELA study. Hypertension (Dallas, Tex. : 1979). 2014 Dec:64(6):1205-11. doi: 10.1161/HYPERTENSIONAHA.114.03975. Epub 2014 Sep 8
[PubMed PMID: 25201892]
[54]
Bouzas-Mosquera A, Broullón FJ, Álvarez-García N, Méndez E, Peteiro J, Gándara-Sambade T, Prada O, Mosquera VX, Castro-Beiras A. Left atrial size and risk for all-cause mortality and ischemic stroke. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2011 Jul 12:183(10):E657-64. doi: 10.1503/cmaj.091688. Epub 2011 May 24
[PubMed PMID: 21609990]