[1]
Aydin F, Turgay Yildirim O, Dagtekin E, Huseyinoglu Aydin A, Aksit E. Acute Inferior Myocardial Infarction Caused by Lightning Strike. Prehospital and disaster medicine. 2018 Dec:33(6):658-659. doi: 10.1017/S1049023X18000705. Epub 2018 Aug 29
[PubMed PMID: 30156178]
[2]
Lévy S. Bundle branch blocks and/or hemiblocks complicating acute myocardial ischemia or infarction. Journal of interventional cardiac electrophysiology : an international journal of arrhythmias and pacing. 2018 Aug:52(3):287-292. doi: 10.1007/s10840-018-0430-3. Epub 2018 Aug 22
[PubMed PMID: 30136134]
[3]
Balasubramanian K, Ramachandran B, Subramanian A, Balamurugesan K. Combined ST Elevation in a Case of Acute Myocardial Infarction: How to Identify the Infarct-related Artery? International journal of applied & basic medical research. 2018 Jul-Sep:8(3):184-186. doi: 10.4103/ijabmr.IJABMR_365_16. Epub
[PubMed PMID: 30123751]
Level 3 (low-level) evidence
[4]
Bouhuijzen LJ, Stoel MG. Inferior acute myocardial infarction with anterior ST-segment elevations. Netherlands heart journal : monthly journal of the Netherlands Society of Cardiology and the Netherlands Heart Foundation. 2018 Oct:26(10):515-516. doi: 10.1007/s12471-018-1147-8. Epub
[PubMed PMID: 30105594]
[5]
Aguiar Rosa S, Timóteo AT, Ferreira L, Carvalho R, Oliveira M, Cunha P, Viveiros Monteiro A, Portugal G, Almeida Morais L, Daniel P, Cruz Ferreira R. Complete atrioventricular block in acute coronary syndrome: prevalence, characterisation and implication on outcome. European heart journal. Acute cardiovascular care. 2018 Apr:7(3):218-223. doi: 10.1177/2048872617716387. Epub 2017 Jun 15
[PubMed PMID: 28617040]
[6]
Roshdy HS, El-Dosouky II, Soliman MH. High-risk inferior myocardial infarction: Can speckle tracking predict proximal right coronary lesions? Clinical cardiology. 2018 Jan:41(1):104-110. doi: 10.1002/clc.22859. Epub 2018 Jan 29
[PubMed PMID: 29377172]
[7]
Albulushi A, Giannopoulos A, Kafkas N, Dragasis S, Pavlides G, Chatzizisis YS. Acute right ventricular myocardial infarction. Expert review of cardiovascular therapy. 2018 Jul:16(7):455-464. doi: 10.1080/14779072.2018.1489234. Epub 2018 Jun 27
[PubMed PMID: 29902098]
[8]
Albaghdadi A, Teleb M, Porres-Aguilar M, Porres-Munoz M, Marmol-Velez A. The dilemma of refractory hypoxemia after inferior wall myocardial infarction. Proceedings (Baylor University. Medical Center). 2018 Jan:31(1):67-69. doi: 10.1080/08998280.2017.1401347. Epub 2018 Feb 1
[PubMed PMID: 29686558]
[9]
Sibbing D, Aradi D, Jacobshagen C, Gross L, Trenk D, Geisler T, Orban M, Hadamitzky M, Merkely B, Kiss RG, Komócsi A, Dézsi CA, Holdt L, Felix SB, Parma R, Klopotowski M, Schwinger RHG, Rieber J, Huber K, Neumann FJ, Koltowski L, Mehilli J, Huczek Z, Massberg S, TROPICAL-ACS Investigators. Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): a randomised, open-label, multicentre trial. Lancet (London, England). 2017 Oct 14:390(10104):1747-1757. doi: 10.1016/S0140-6736(17)32155-4. Epub 2017 Aug 28
[PubMed PMID: 28855078]
Level 1 (high-level) evidence
[10]
Bahramali E, Askari A, Zakeri H, Farjam M, Dehghan A, Zendehdel K. Fasa Registry on Acute Myocardial Infarction (FaRMI): Feasibility Study and Pilot Phase Results. PloS one. 2016:11(12):e0167579. doi: 10.1371/journal.pone.0167579. Epub 2016 Dec 1
[PubMed PMID: 27907128]
Level 2 (mid-level) evidence
[11]
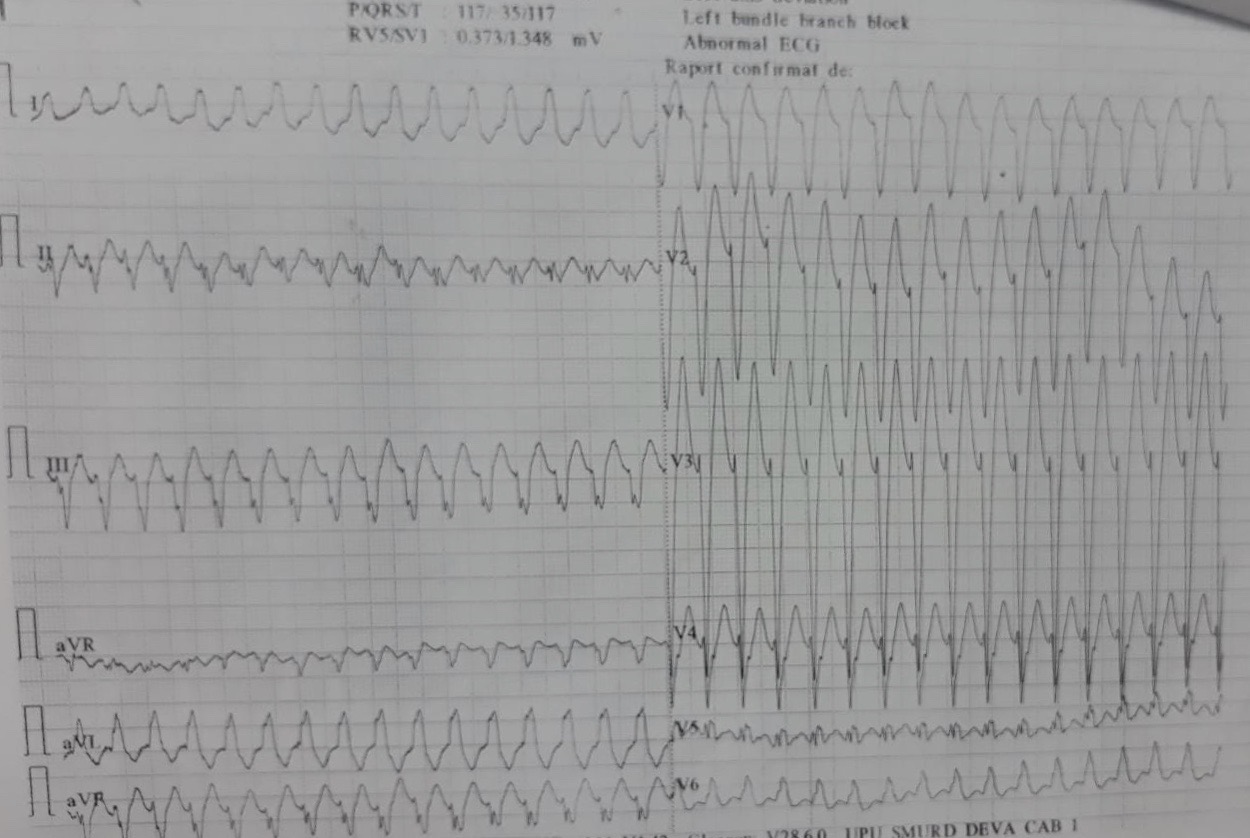
Udroiu CA, Cotoban A, Ursulescu A, Siliste C, Vinereanu D. Interdisciplinary Approach in a Complex Case of STEMI. Maedica. 2014 Dec:9(4):382-6
[PubMed PMID: 25705309]
Level 3 (low-level) evidence
[12]
Martin D, Bekiaris B, Hansen G. Mobile emergency simulation training for rural health providers. Rural and remote health. 2017 Jul-Sep:17(3):4057. doi: 10.22605/RRH4057. Epub 2017 Oct 17
[PubMed PMID: 29040811]
[13]
Kiani F, Hesabi N, Arbabisarjou A. Assessment of Risk Factors in Patients With Myocardial Infarction. Global journal of health science. 2015 May 28:8(1):255-62. doi: 10.5539/gjhs.v8n1p255. Epub 2015 May 28
[PubMed PMID: 26234995]
[14]
Li H, Guo W, Dai W, Li L. Short-versus long-term dual antiplatelet therapy after second-generation drug-eluting stent implantation: a systematic review and meta-analysis of randomized controlled trials. Drug design, development and therapy. 2018:12():1815-1825. doi: 10.2147/DDDT.S165435. Epub 2018 Jun 22
[PubMed PMID: 29970956]
Level 1 (high-level) evidence
[15]
Ginanjar E, Yulianto Y. ST Elevation in Lead aVR and Its Association with Clinical Outcomes. Acta medica Indonesiana. 2017 Oct:49(4):347-350
[PubMed PMID: 29348386]
Level 2 (mid-level) evidence
[16]
Altıntaş B, Yaylak B, Ede H, Altındağ R, Baysal E, Bilge Ö, Çiftçi H, Adıyaman MŞ, Karahan MZ, Kaya I, Çevik K. Impact of right ventricular diastolic dysfunction on clinical outcomes in inferior STEMI. Herz. 2019 Apr:44(2):155-160. doi: 10.1007/s00059-017-4631-9. Epub 2017 Oct 9
[PubMed PMID: 28993840]
Level 2 (mid-level) evidence