Continuing Education Activity
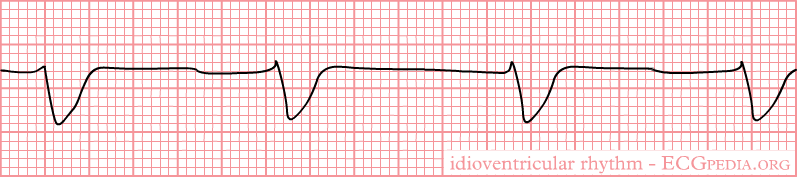
Idioventricular rhythm is a slow regular ventricular rhythm with a rate of less than 50 bpm, absence of P waves, and a prolonged QRS interval. When the sinoatrial node is blocked or depressed, latent pacemakers become active to conduct rhythm secondary to enhanced activity and generate escape beats that can be atrial itself, junctional or ventricular. When ventricular rhythm takes over, it is essentially called Idioventricular rhythm. Idioventricular rhythm is very similar to ventricular tachycardia, except the rate is less than 60 bpm and is alternatively called a "slow ventricular tachycardia." When the rate is between 50 to 100 bpm, it is called accelerated idioventricular rhythm. This topic reviews the evaluation and management of idioventricular rhythm. This activity highlights important etiologies and correlating factors contributing to idioventricular rhythms and their management by an interprofessional team.
Objectives:
- Identify the characteristic features of an idioventricular rhythm.
- Review the clinical context leading to idioventricular rhythm and differentiate from ventricular tachycardia and other similar etiologies.
- Describe the management principles and treatment modalities.
- Summarize how the interprofessional team can improve outcomes for patients with idioventricular rhythms.
Introduction
Idioventricular rhythm is a slow regular ventricular rhythm, typically with a rate of less than 50, absence of P waves, and a prolonged QRS interval. When the sinoatrial node is blocked or suppressed, latent pacemakers become active to conduct rhythm secondary to enhanced activity and generate escape beats that can be atrial itself, junctional or ventricular. When ventricular rhythm takes over, it is essentially called Idioventricular rhythm.
Idioventricular rhythm is similar to ventricular tachycardia, except the rate is less than 60 bpm and is alternatively called a 'slow ventricular tachycardia.' When the rate is between 50 to 110 bpm, it is referred to as accelerated idioventricular rhythm.[1]
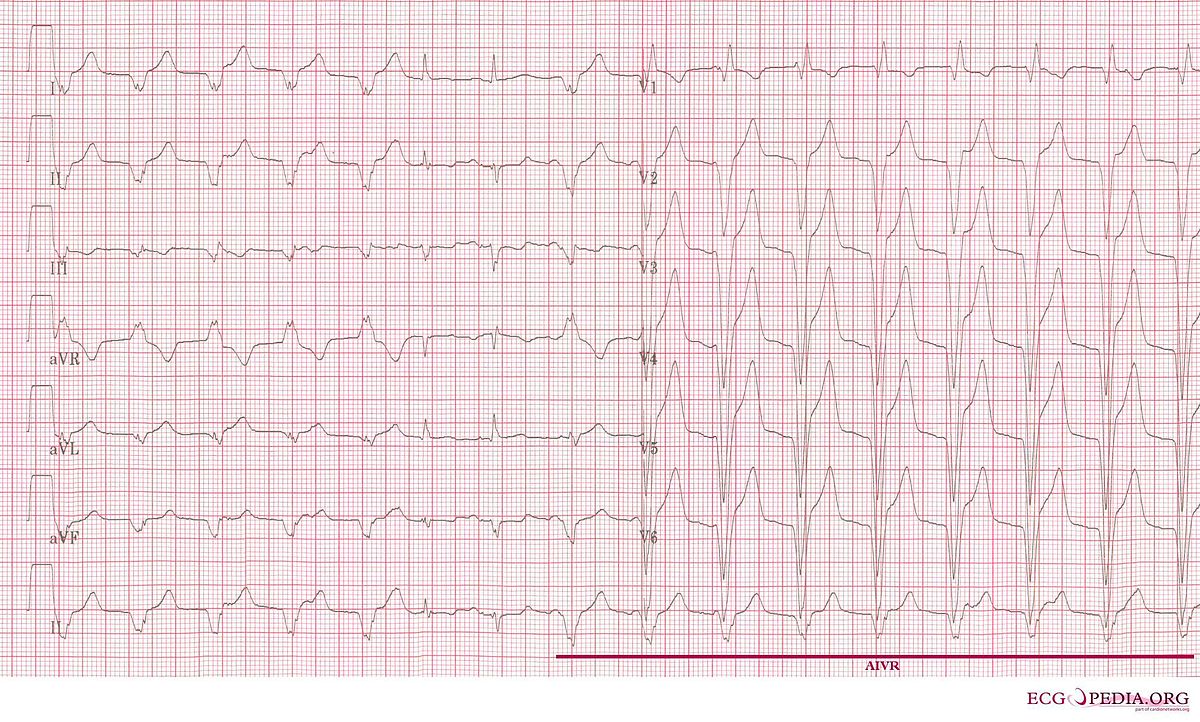
Accelerated idioventricular rhythm (AIVR) results when the rate of an ectopic ventricular pacemaker exceeds that of the sinus node with a rate of around 50 to 110 bpm and often associated with increased vagal tone and decreased sympathetic tone. It is a hemodynamically stable rhythm and can occur after a myocardial infarction during the reperfusion phase.[2]
Etiology
Idioventricular rhythm can be seen in and potentiated by various etiologies.
It commonly presents in atrioventricular (AV) dissociation due to an advanced or complete heart block or when the AV junction fails to produce 'escape' rhythm after a sinus arrest or sinoatrial nodal block.
Idioventricular rhythm can also be seen during the reperfusion phase of myocardial infarction, especially in patients receiving thrombolytic therapy.[3]
Electrolyte abnormalities can increase the chances of idioventricular rhythm.
Various medications such as digoxin at toxic levels, beta-adrenoreceptor agonists like isoprenaline, adrenaline, anesthetic agents including desflurane, halothane, and illicit drugs like cocaine have reported being etiological factors in patients with AIVR.[4][5]
Idioventricular rhythm can also infrequently occur in infants with congenital heart diseases and cardiomyopathies such as hypertrophic cardiomyopathies and arrhythmogenic right ventricular dysplasia.[6]
Accelerated Idioventricular rhythm is also be rarely seen in patients without any evidence of cardiac disease. The mechanism involves a decrease in the sympathetic but an increase in vagal tone. It can also present in athletes.[7]
Pathophysiology
Idioventicular rhythm has two similar pathophysiologies described leading to ectopic focus in the ventricle to take the role of a dominant pacemaker.
Ectopic automaticity generated by abnormal calcium-dependent automatism that affects the diastolic depolarization, i.e., phase 4 action potential, is the main electrophysiological mechanism affecting the AIVR. The trigger activity is the main arrhythmogenic mechanism involved in patients with digitalis toxicity.[6]
Sinoatrial node and the atrioventricular node may get suppressed with structural damage or functional dysfunction potentiated by enhanced vagal tone. Subsequently, the ventricle may assume the role of a dominant pacemaker. With the slowing of the intrinsic sinus rate and ventricular takeover, idioventricular rhythm is generated. The idioventricular rhythm becomes accelerated when the ectopic focus generates impulses above its intrinsic rate leading to a heart rate between 50 to 110 beats per minute.
Isorhythmic dissociation, fusion or capture beats can occur when sinus and ectopic foci discharge at the same rate.[2]
The rhythm has variable associations relative to bundle branch blocks depending on the foci site.
An incomplete left bundle branch block pattern presents if ventricular rhythm arises from the right bundle branch block. An incomplete right bundle branch block is seen when the pacemaker is in the left bundle branch. Rhythms arising in the anterior or posterior fascicle of the left bundle branch exhibit a pattern of incomplete right bundle branch block with left posterior fascicular block and left anterior fascicular block, respectively.[8]
Ventricular rhythm arising more distally in the Purkinje plexus of the left ventricular myocardium displays the pattern of right bundle branch block, and those of right ventricular origin display the pattern of left bundle branch block.
History and Physical
The signs and symptoms for the idioventricular or accelerated idioventricular rhythm are variable and are dependent on the underlying etiology or causative mechanism leading to the rhythm. In most cases, the patient remains completely asymptomatic and are diagnosed during cardiac monitoring. Infrequently, patients can have palpitations, lightheadedness, fatigue, and even syncope.
Evaluation
Electrocardiography with clinical correlation is essential for diagnosis.[2]
- Rhythm: ventricular: regular, atrial: absent
- Rate: less than 40 beats per minute for idioventricular rhythm
- Rate 50 to 110 bpm for accelerated idioventricular rhythm
- PR: Not applicable
- QRS complex: Wide (greater than 0.10 seconds)
Treatment / Management
Idioventricular rhythm is mostly benign, and treatment has limited symptomatic or prognostic value.[9]
Management principles of idioventricular rhythm involve treating underlying causative etiology such as digoxin toxicity reversal if present, management of myocardial ischemia, or other cardiac structural/functional problems. [4][5]
Rarely, a patient can present with symptoms and may not tolerate idioventricular rhythm secondary to atrioventricular dyssynchrony, fast ventricular rate, or degenerated ventricular fibrillation of idioventricular rhythm. Medical therapy may also be beneficial in patients with biventricular failure to restore atrial kick with mechanism, including to increase sinus rate and atrioventricular (AV) conduction. Atropine may be trialed in such scenarios.[10]
Antiarrhythmic agents, including amiodarone and lidocaine, may also be potentially used along with medications such as verapamil or isoproterenol. Very rarely, atrial pacing may be an option.[11]
However, in reperfusion post-myocardial ischemia and cardiomyopathy, the use of beta-blockers has not shown to decrease the risk of occurrence of idioventricular rhythm.[12]
Differential Diagnosis
Differential diagnosis[6]:
- Slow ventricular tachycardia
- Complete heart block
- Junctional rhythm with aberrancy
- Supraventricular tachycardia with aberrancy
- Slow antidromic atrioventricular reentry tachycardia
Prognosis
Idioventricular rhythm is a benign rhythm in most settings and usually does not require treatment with a good prognosis. It usually self-limits and resolves when the sinus frequency exceeds that of ventricular foci and arrhythmia requires no treatment.
In occasional scenarios when there is AV dissociation leading to syncope or sustained or incessant AIVR, the risk of sudden death is increased and arrhythmia should be treated.[12]
Pearls and Other Issues
Things to take into consideration when managing the rhythm are pertinent clinical history, which may help determine the causative etiology. Management is clinical monitoring.
Another important thing to consider in AIVR is that over the past many years, data has been variable with regards to Accelerated Idioventricular rhythm as a prognostic marker of complete reperfusion after myocardial infarction.
The more current data correlates the presence of AIVR with reperfusion with myocardial infarction during the acute phase with the suggestion of vessel opening however does not suggest it to be a marker for reperfusion during the acute phase of myocardial infarction.[6]
Enhancing Healthcare Team Outcomes
An interprofessional team that provides a holistic and integrated approach is essential when noticing an idioventricular rhythm.
Care coordination between various patient care teams to determine etiology presenting idioventricular rhythm is very helpful. The patient may have underlying cardiac structural etiology, ischemia as a contributory cause, or it could be secondary to anesthetic type, medication, or an electrolyte disturbance. Therefore, close coordination between teams is mandatory. Cardiology nurses monitor patients, administer medications, and inform the team about patient status. Pharmacists verify medications and check for drug-drug interactions; a board-certified cardiology pharmacist can assist the clinician team in agent selection and appropriate dosing. These interprofessional strategies will drive better patient outcomes. [Level 5]
Idioventricular rhythm is benign in most cases, and appropriate patient education and reassurance are important.