Continuing Education Activity
Idiopathic guttate hypomelanosis (IGH) is a benign, acquired skin condition characterized by small, round-to-oval, hypopigmented spots, typically 2 to 5 mm in diameter. These common lesions primarily appear on sun-exposed areas, such as the forearms, shins, and face. IGH results from a reduction in melanocytes or melanin within the skin, often due to UV radiation, leading to localized loss of pigmentation. IGH is idiopathic, appearing without a known underlying disease. This condition is most frequently observed in fair-skinned individuals, particularly with advancing age.
IGH is generally asymptomatic, without associated pain or itching. Histologically, the lesions exhibit reduced melanin and melanocytes in the epidermis. IGH is primarily a cosmetic concern and typically does not require treatment, though topical therapies or cosmetic camouflage may be used for aesthetic purposes. No significant risk of malignancy or progression is associated with IGH.
This activity for healthcare professionals is designed to enhance learners' proficiency in evaluating and managing IGH. Participants will deepen their understanding of the condition's etiology, epidemiology, pathophysiology, clinical presentation, and best diagnostic and therapeutic practices. Improved skills will empower interprofessional teams to make well-informed clinical decisions, improving care for individuals with this complex and prevalent condition.
Objectives:
Identify the clinical and dermoscopic features indicative of idiopathic guttate hypomelanosis.
Implement individualized management approaches for idiopathic guttate hypomelanosis.
Apply effective communication strategies to educate patients about the benign nature of idiopathic guttate hypomelanosis, set realistic expectations for treatment outcomes, and provide recommendations on available therapeutic options, including their benefits, limitations, and potential risks.
Collaborate with the interprofessional team to educate, treat, and monitor patients with idiopathic guttate hypomelanosis to improve health outcomes.
Introduction
Idiopathic guttate hypomelanosis (IGH) is a benign, typically asymptomatic leukodermic dermatosis of unclear etiology, classically seen in older adults with fair skin, and often goes unrecognized or undiagnosed.[1] Occasionally, IGH is aesthetically displeasing. However, this condition is not dangerous. Once present, lesions do not remit. Treatment aims to improve cosmesis.
Etiology
The etiology of IGH remains unknown. Proposed theories suggest it may result from the skin's natural aging process, cumulative chronic sun exposure, or repeated microtrauma.[2] However, none of these hypotheses have been confirmed.
Epidemiology
IGH occurs in all races and skin types but is more common in fair-skinned individuals. The condition may also affect darker skin types, and lesions may be more noticeable in such patients. Women's heightened perception of cosmetic concerns may have contributed to the previous belief that IGH is more common in this patient group. However, recent studies indicate equal prevalence between the sexes. Regardless of sex, prevalence and incidence increase with age. IGH may appear in young adults in their 20s and 30s, but a recent study found that 87% of individuals aged 40 and older had at least 1 lesion, while up to 80% of people older than 70 are affected.
Pathophysiology
Given its extremely high overall incidence, the pathogenesis of IGH appears complex, likely involving both genetic and environmental factors. Many studies highlight sun exposure as a central factor, though a definitive causal relationship remains unproven. Interestingly, lesions are uncommon on the face and neck—typical sites for other actinic processes—suggesting a multifactorial pathophysiology.
Small studies have reported a higher prevalence of these lesions among relatives of patients with IGH compared to controls, implying at least a partial hereditary component. A recent study supported this theory, noting a statistically significant increase in IGH incidence among renal transplant patients with the human leukocyte antigen DQ3 haplotype and a negative association with the human leukocyte antigen DR8 haplotype.[3]
Histopathologic findings have been inconsistent in identifying underlying mechanisms. Some studies attribute IGH to a reduction in melanocyte numbers, while others suggest structural abnormalities, such as fewer melanosomes, decreased dendrites, reduced tyrosinase activity, or defective keratinocyte uptake rather than a melanocytic process.[4] Additionally, some studies propose a role for senescent fibroblasts in IGH development.[5]
Histopathology
As diagnosis is typically based on history and physical examination alone, histopathologic evaluation of IGH lesions is usually unnecessary. If a biopsy is performed, pathology findings classically show a reduced number of epidermal melanocytes containing 3,4-dihydroxyphenylalanine (DOPA) within the basal layer, though not completely absent as in vitiligo. Furthermore, melanin pigmentation is decreased, best appreciated when compared with the adjacent normal epidermis, as isolated lesions without neighboring normal tissue may be difficult to assess.
Other histologic features include flattening of rete ridges, with or without epidermal atrophy. Epidermal atrophy is more commonly observed in non-sun-exposed areas. Orthokeratosis, either in a "basket-weave" pattern or as compact orthokeratosis, may be present in the stratum corneum.
Electron microscopy findings suggest melanocyte degeneration, characterized by a dilated endoplasmic reticulum and mitochondrial swelling. A decrease in melanosomes and dendrites has also been observed, contrasting with vitiligo, where dendritic processes are increased.[6][7]
History and Physical
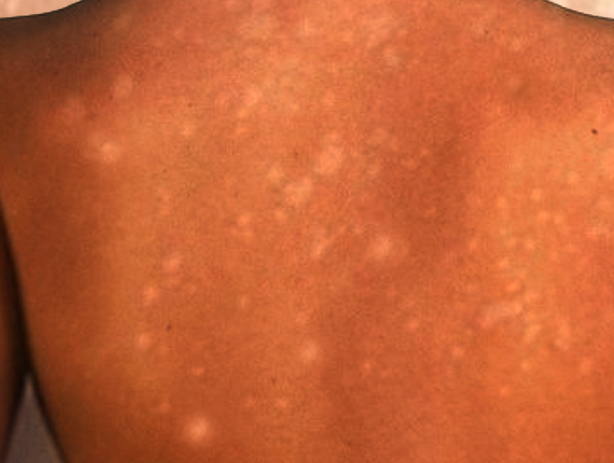
IGH presents as multiple small, scattered, discrete, round or oval, achromic or hypochromic macules, typically 2 to 6 mm in size, that develop gradually over the years (see Image. Guttate Hypomelanosis). Occasionally, larger lesions up to 2.5 cm appear. Lesions are usually smooth, though scaly and hyperkeratotic variants have been reported.[8]
Patterns or groupings do not form, and lesions remain stable in size without regression. Adnexal structures, including hair follicles, appear unaffected, with hairs within lesions retaining their pigment. IGH occurs most commonly in sun-exposed areas, particularly the dorsal upper and lower extremities, with a preference for distal over proximal sites. However, sun-protected areas, including the trunk and, rarely, the face, may also be affected.
Evaluation
Given the benign course of IGH, laboratory, radiographic, or other diagnostic tests are typically unnecessary. However, dermoscopy can be a valuable tool for evaluating IGH lesions. This assessment can reveal the following distinct morphological patterns, listed in order of incidence:
- Amoeboid: Pseudopod-like extensions
- Feathery: Irregular pigmentation with feathery margins and a whitish central area
- Petaloid: Polycyclic margins resembling flower petals
- Nebuloid: Indistinct, smudged borders
The nebulous pattern appears more frequently in early lesions, while amoeboid, feathery, and petaloid patterns are more common in older lesions.[9]
Treatment / Management
Patients should be reassured that IGH lesions are benign and do not require treatment. No universally accepted, effective therapies exist for this condition. However, since sunlight is likely a contributing or even precipitating factor, all patients should use sunscreens and physical barriers.
Several treatments have shown variable success, alone or in combination, in improving the condition cosmetically. These treatments include cryotherapy, superficial abrasion, topical steroids, topical retinoids, topical calcineurin inhibitors, dermabrasion, topical 88% phenol, fractional carbon dioxide lasers, nonablative fractional photothermolysis with a fractional 1,550-nm ytterbium/erbium fiber laser, and excimer light treatment.[10] More recently, 50% trichloroacetic acid peels have also been used.[11]
Patients should be counseled on the risk of worsening leukoderma with cryotherapy and the potential for long-standing, though not permanent, erythema and postinflammatory hyperpigmentation with treatments such as fractional carbon dioxide lasers. Promising studies suggest that combining fractional photothermolysis with topical calcineurin inhibitors may enhance outcomes. More recently, research has noted increased melanocyte presence following microneedling combined with microinfusion of 5-fluorouracil via a tattoo machine, presenting a potential treatment option.[12][13][14]
Differential Diagnosis
The differential diagnosis of guttate leukoderma is broad, as similar lesions appear in various generalized dyschromatoses. Distinguishing IGH from vitiligo early in the disease course is crucial since IGH lesions remain stable, whereas vitiligo progresses. Other common dermatologic conditions in the differential diagnosis include pityriasis versicolor, pityriasis alba, café au lait macules, lichen sclerosus, guttate morphea, and post-inflammatory hypopigmentation. Each condition has a characteristic distribution and associated findings.
Less commonly considered but important differential diagnoses include achromic verruca plana, pityriasis lichenoides chronica, disseminated hypopigmented keratoses following psoralen and ultraviolet A (PUVA) therapy, clear cell papulosis, and atrophie blanche. Achromic verruca plana lesions are more susceptible to koebnerization and, histologically, exhibit koilocytes. Pityriasis lichenoides chronica presents with more widespread lesions accompanied by an overlying scale. Disseminated hypopigmented keratoses develop after psoralen and ultraviolet A therapy, appearing as well-demarcated, small, hypopigmented, flat-topped papules uniformly distributed on the trunk and extremities. Histologic findings include variable acanthosis, orthokeratosis or parakeratosis, papillomatosis, and a normal amount of melanin and melanocytes.
Clear cell papulosis, a rare condition in young children, primarily affects the face and trunk and may follow "milk lines." Lesions consist of multiple hypopigmented, barely elevated, small, flat-topped papules and macules. Histologically, large clear cells in the basal layer display an immunohistochemical staining pattern similar to Toker clear cells of the nipple and extramammary Paget disease.
Both IGH and atrophie blanche favor the distal dorsal extremities, such as the dorsal shins. However, atrophie blanche lesions typically arise at sites of previous ulcers, feature more angulated margins, and appear as porcelain-white, depressed atrophic scars with a surrounding rim of telangiectasia.[15]
Prognosis
IGH is a benign condition with an excellent prognosis. However, once present, lesions do not remit without treatment. As such, IGH primarily represents a cosmetic concern. The condition may be an indication of cumulative sun exposure. However, no direct correlation has been made to date.
Complications
While complications are rare, IGH may have cosmetic and psychological effects, especially in individuals with darker skin tones, as contrast with surrounding pigmentation in the skin of these patients is more noticeable. Persistent lesions can cause distress and reduce quality of life, particularly for individuals concerned with aesthetic appearance. Additionally, differentiating IGH from more serious conditions such as vitiligo, post-inflammatory hypopigmentation, and leukoderma-associated malignancies may lead to unnecessary biopsies or interventions. Although generally stable, an increasing number or size of lesions over time can heighten psychosocial concerns, emphasizing the need for patient reassurance and, in some cases, dermatologic intervention.
Deterrence and Patient Education
Deterrence of IGH primarily involves photoprotection, as chronic UV exposure is a significant contributing factor. Patients should be advised regarding the regular use of broad-spectrum sunscreens, protective clothing, and sun avoidance during peak hours to minimize lesion progression. Although IGH is benign and asymptomatic, patient education should focus on differentiating it from more concerning pigmentary disorders, such as vitiligo or post-inflammatory hypopigmentation, to alleviate unnecessary anxiety.
Individuals seeking cosmetic improvement may be counseled on available treatment options, including topical retinoids, fractional laser therapy, and superficial chemical peels, even though the efficacy of these modalities varies. Reassurance regarding the benign nature of IGH is essential, particularly for patients experiencing psychosocial distress due to significantly contrasting skin pigmentation.
Enhancing Healthcare Team Outcomes
Recognizing IGH helps prevent unnecessary treatments. The interprofessional team includes primary care providers, dermatologists, and specialty-trained nurses. Uncertain diagnoses should be referred to dermatology, and dermatology nurses play a key role in patient education.