Continuing Education Activity
Phalanx fractures of the hand are some of the most common fractures occurring in humans. They are often noted to be in the more common of all upper extremity fractures and present with a long list of post-injury complications regardless of treatment, most commonly in relation to finger and hand function. Nonetheless, they generally heal well with either conservative or surgical treatment. This article highlights the key points of diagnosing and treating patients with phalanx fractures of the hand by an interprofessional team.
Objectives:
Identify the common presentation of a patient with phalanx fractures of the hand.
Outline the classic physical exam findings associated with phalanx fractures of the hand.
Review the management options available for phalanx fractures of the hand.
Describe the importance of collaboration and communication among the interprofessional team to improve outcomes for patients affected by phalanx fractures of the hand.
Introduction
Phalanx fractures are some of the most common fractures occurring in humans.[1][2][3][4][5][6][7][8] They are often noted to be in the more common of all upper extremity fractures and present with a long list of post-injury complications regardless of treatment, most commonly in relation to finger and hand function.[4][5][6][8][9][10][11][12][13][14][15][16] Nonetheless, they generally heal well with either conservative or surgical treatment.[8][14][17][18]
Phalanx fractures are most often classified using a descriptive pattern noting location, angulation, and displacement. They are often divided in location to the base, shaft, or condyle of their respective phalanx.[19] Therefore, understanding of proper diagnosis and treatment of phalanx fractures starts with a knowledge base of the intricate anatomy.
Each thumb (first digit) contains a proximal and distal phalanx, while the index (second digit), long (third digit), ring (fourth digit), and small (fifth digit) fingers all contain a proximal, middle, and distal phalanx. The proximal and middle phalanges can be subdivided into a base, shaft, and head from proximal to distal. The heads of the middle and proximal phalanges are formed by two condyles separated by an intercondylar notch. The proximal and middle phalanges tend to have a slight palmar concavity, while the distal phalanx is relatively straight. The distal phalanx is divided into a base, shaft, and tuft and is protected dorsally by the nail plate with dense fibrous connections to the surrounding soft tissue.[20][21]
The base of each proximal phalanx articulates with its respective metacarpal forming the metacarpophalangeal (MCP) joints. The base of the middle phalanx in digits 2 to 5 articulates with the head of the respective proximal phalanx to form the proximal interphalangeal (PIP) joint. The base of the distal phalanx in digits 2 to 5 articulates with the head of the respective middle phalanx to form the distal interphalangeal (DIP) joint. The articulation between the head of the proximal phalanx and the base of its respective distal phalanx forms the interphalangeal (IP) joint of the thumb.[21] Collateral ligaments lie on radial and ulnar borders of each of these joints and are most taut at about 90 degrees of flexion.[22] The volar plate is a strong ligamentous structure overlying the volar aspect of the joints that resists hyperextension.[21]
The soft tissue anatomy surrounding the phalanges is intricate with distinct flexor and extensor mechanisms that contribute to motion and overall stabilization of fracture fragments. The flexor digitorum superficialis (FDS) tendon passes over the volar surface of the MCP joint, proximal phalanx, PIP joint, where it splits into two slips, and inserts on the junction of the proximal and middle one-third of the middle phalanx. The flexor digitorum profundus (FDP) tendon passes dorsal to the FDS tendon over the volar aspect of the MCP joint, proximal phalanx, PIP joint passing between the two slips of the FDS tendon, middle phalanx, DIP joint, and inserts on the base of the proximal phalanx. A complex network of vincula acts as a tether between the flexor tendons and the proximal and middle phalanges. The extensor hood is the complex expansion of the extensor tendons on the dorsal aspect of the finger. The central slip of the extensor mechanism attaches to the base of the middle phalanx dorsally while lateral bands proceed to a terminal slip, which attaches to the base of the distal phalanx. Intrinsic muscles of the hand (lumbricals and interossei) attach to the lateral bands of the extensor mechanism. Sagittal bands on each side of the finger attach the extensor hood to the volar plate and flexor tendon sheath near the PIP joint.
A single digital nerve and artery lie on both the radial and ulnar aspects of the finger slightly volar to midline with small branches and capillaries supplying the surrounding soft tissue and superficial structures.
Etiology
Phalanx fractures of the hand are often related to blunt, penetrating, or crush trauma; however, pathologic causes such as tumor and infection cannot be overlooked.[13][16][23][24] Hand fractures, in general, are most commonly caused by falls, crush injury, and sports.[1][3][19] Crush injuries, usually by door slam, are the most common mechanism for hand fractures in children younger than eight-years-old, while falls and sports injuries are known to be more common in older children.[1][3] Other common causes of hand fractures in children include crush by machinery, car accident, and injury by a heavy object.[1]
Epidemiology
The incidence of phalanx fractures is about 0.012% of people per year in the United States.[4] They are the second to distal radius and/or ulna fractures as the most common fracture location overall in the upper extremity across most age groups and comprise 23% of the emergency department diagnosed upper extremity fractures.[4][5] The distribution of phalanx fractures amongst all upper extremity fractures appears bimodal, falling between 45- to 85-years-old and then becoming the most common upper extremity fracture among patients older than 85.[5] Phalangeal fractures are noted to decrease in incidence with increasing socioeconomic status.[4]
Hand and finger fractures are more common in male children than female across most age groups.[1][2][3][18] Phalanx fractures are also slightly more common in adult males than females.[4][5][6][7] The right and left hands are equally affected.[1][3][7] The small, ring, and long fingers are more commonly fractured than the thumb or index finger.[1][2][3][7][8][18] The proximal phalanx is the most commonly fractured bone in the hand in most age ranges in children and adults.[1][2][3][7]
Pathophysiology
Phalanx fractures of the hand are often related to blunt, penetrating, or crush trauma; however, pathologic causes such as tumor and infection cannot be overlooked.[13][16][23][24] Hand fractures, in general, are most commonly caused by falls, crush injury, and sports.[1][3][19] Other common causes of hand fractures in children include crushing by machinery, car accident, and injury by a heavy object.[1]
Bending forces to the phalanx shaft tend to produce transverse fractures while torsional and angular forces produce spiral and oblique fractures. In general, crushing injuries produce significant comminution in fractures. Intra-articular fractures are often caused by axial loading but can also be caused by avulsion of tendinous insertion sites causing angular patterns.[20] The deforming forces of the proximal attachment of the central slip combined with the attachment of the intrinsic hand muscles to the extensor mechanism in relation to the more distal FDS tendon insertion cause apex volar angulation of proximal phalanx fractures. Similarly, fractures near the base of the middle phalanx that occur between the two tendinous insertions result in apex dorsal angulation. Fractures of the middle phalanx occurring distal to the insertion of the FDS tendon are often apex volar due to its flexion of the proximal fragment in relation to extension of the distal fragment by the terminal slip of the extensor mechanism.[22]
History and Physical
The mechanism of injury should agree with the magnitude and nature of the injury. If this is not the case, suspicion should be raised for pathologic fracture due to tumor or infection, as well as the potential for physical abuse.[13][16][23][24] Mechanisms typically described include falls, crush injuries, and sports.[1][3][19] Patients may complain about pain, swelling, deformity, decreased range of motion, and/or instability around the injury site.[20]
Gross observation may reveal rotational or angular deformity arising from the phalangeal shaft or near any of the nearby articulations.[16][19][20] Rotational deformity is best assessed with flexion and extension of the digits in which they all should point to the scaphoid tubercle. Overlap or scissoring of digits may signal rotational deformity but should be compared bilaterally when able as anatomical variation can also cause mild forms of this.[13][16][19][20]
Palpation reveals tenderness overlying the fracture site and injured soft tissue structures. Meticulous examination of the soft tissue envelope should be performed about the hand and fingers as soft tissue injury from these mechanisms can be quite robust.[16][19][20]
The active range of motion of the affected finger at nearby articulations is often limited secondary to pain and early swelling. Local anesthetic in the form of a hematoma or digital nerve block can help relieve pain and be beneficial to evaluate alignment, range of motion further, and strength; however, it should not be performed before a careful neurovascular exam.[16][19][20]
Neural status can be evaluated with general sensation, two-point discrimination, and motor function. Findings may range from fully intact to any deficit, pending the soft tissue injury that occurred. Digital nerves on the radial and ulnar aspects of the finger tend to supply sensation from one half the digit; however, some overlap may occur on dorsal and volar surfaces.
Vascular status supplied by digital arteries on the radial and ulnar aspects of the finger can be examined by looking at skin coloration as well as capillary refill of the distal skin and the nail bed. In general, a finger with a single digital artery laceration will still have a brisk capillary refill, though it may be slowed with dusky skin coloration.
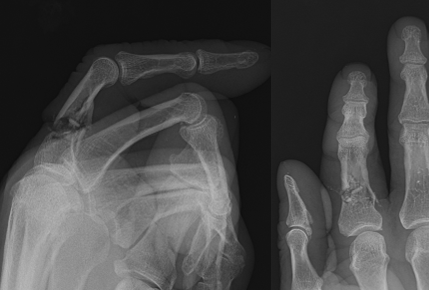
Evaluation
Plain radiographs of the hand with standard anteroposterior, oblique, and lateral views are often necessary to aid in the diagnosis of most phalanx fractures.[13][19][20] Similar views of the specific anatomic region under suspicion could also be obtained for further detail.[19][20] The contralateral hand can be used for comparison if unclear but suspicious findings are noted, especially in skeletally immature patients.[19] Radiographs reveal fracture lines with malalignment and angulation as well as overlying soft tissue edema and any degenerative, oncological, rheumatological, or metabolic changes to the rest of the hand visualized.[16]
Musculoskeletal ultrasound is an emerging modality proving useful for the diagnosis of phalanx fracture as well as associated soft tissue injury.[25] Computed tomography may be helpful further to delineate the anatomy of severely comminuted or intra-articular fractures as well as further delineate pathologic fracture.[13][19][26] MRI is rarely indicated but can help assess associated soft tissue injury and pathologic fractures.[16][19][26]
Treatment / Management
The aim of treatment for phalanx fractures of the hand is to appropriately heal the fracture while avoiding complications such as stiffness and deformity, which decrease function.[12][13] Treatment should consider the additional soft tissue injury that occurred at the time of injury with a plan for adequate rehabilitation.[13] Ideal treatment follows the principles of obtaining fracture stability and allowing for early range of motion.[13][19] Nonsurgical treatments typically have the advantage of preventing scar tissue formation from soft tissue damage related to dissection but require periods of immobilization for adequate fracture stability and healing. Surgical treatments typically allow for improved stability and earlier range of motion at the cost of increased soft tissue damage and scar formation leading to tissue adhesion and contracture.[12][13][20]
Nonsurgical treatment of phalangeal fractures typically involves closed reduction if indicated, buddy taping to adjacent finger for stabilization and/or splinting versus casting for a short period of immobilization, and then progressive motion and rehabilitation.[16][19][27] Extra-articular distal phalanx fractures rarely require surgical fixation due to the inherent stability of surrounding soft tissue envelope, including the nail plate. However, lacerations to the nail bed or germinal matrix should be treated with nail removal and laceration repair to avoid future nail deformity.[19][20]
Seymour fractures involve the physis of the distal phalanx in pediatric patients with a concomitant nail bed laceration effectively, making it an open fracture. These fractures often trap surrounding soft tissue within the fracture site[28]. They, therefore, require nail plate removal, irrigation and debridement of the laceration, reduction, laceration repair, and antibiotic treatment (generally initialed intravenous and followed by oral) to achieve healing while reducing the inherently high risk of physeal arrest and infection.[28][29][30][31] Small incisions may be necessary at the junction of the paronychial and eponychial folds on either side of the nailbed to adequately expose the laceration.[28][29][30] The acceptable reduction can sometimes be maintained with splinting, although further operative fixation may be necessary and typically involves Kirschner wire percutaneous pinning.[28][30][31] Pediatric fractures, in general, should be considered for surgical treatment to minimize further physeal trauma if attempts at closed reduction have failed.[32] Fixation techniques should minimize injury to the physis.[32]
Surgical treatment is typically recommended for extra-articular fractures when they are associated with an open wound which requires irrigation and excisional debridement to prevent osteomyelitis, instability which if left would lead to deformity (including angular, rotational, and shortening) or decreased hand function, and in cases of multiple displaced hand fractures.[12][13] Transverse extra-articular fractures are typically stabilized with closed reduction and percutaneous pinning with the use of Kirschner wires or open reduction with internal fixation.[6][8][11][12][14][15] The use of percutaneous pinning usually has the advantage of limited soft tissue disturbance but also carries the disadvantage of usually requiring a period of immobilization to augment construct stability. Different techniques for percutaneous pinnings, such as parallel pinning, cross pinning, and transverse pinning, have been described and used in various fracture patterns.[6][11][14][11][15]
Open fixation methods allow for early motion by providing increased stability but require more dissection and soft tissue disruption.[12] Methods for open treatment typically use plate and screw constructs, though interfragmentary screw fixation alone has also shown promise in spiral and long oblique extra-articular fractures.[6][9][14][33] Intramedullary screw fixation methods have also been described.[17][34] Approaches for open reduction and internal fixation vary widely by fracture location and pattern. Dorsal longitudinal approaches are typically used to treat most proximal and middle phalanx fractures, although lateral approaches have also been described.[6][10][14]
Intra-articular fractures are typically treated surgically when associated with joint subluxation or dislocation and in cases in which articular step-off would lead to reduced function by having a bony block to motion or increase risk of development of post-traumatic osteoarthritis.[12][13][35] A 2015 study polling hand surgeons on the appropriate treatment of intra-articular middle phalanx base fractures found agreement on articular step-off or gap of two millimeters or greater, likelihood of joint subluxation or dislocation, and unstable fractures as indicators for operative treatment while other fracture characteristics lacked interobserver agreement. Recommendations for appropriate treatment type for these fractures showed weak interobserver agreement and therefore proved a lack of consensus on best treatment options.[36] A wide number of techniques have been described, including Kirschner wire fixation with extension blocking, Kirschner wire fixation as joysticks, interfragmentary screws, dynamic external fixation, and hemi-hamate arthroplasty.[18][19][37][38][39][40]
Differential Diagnosis
Phalanx fractures in the adult are often not misdiagnosed when appropriate imaging is combined with the physical examination. However, a recent study showed an 8% misdiagnosis rate in pediatric patients with emergency medicine and primary care provider referral to hand surgeons.[3] This is likely related to inexperience with and the subtleties of physeal closure. In this study, fractures were both under- and over-diagnosed. Several other injuries and underlying disorders may be mistaken for phalanx fracture or simultaneously involved, including the following:
- Pathologic fracture – Enchondromas and other underlying tumors in the hand are common and can result in pathologic fracture on initial presentation to the emergency department or office.[13][16][23][24] Similarly, osteomyelitis can weaken the bony structure and initially present with a fracture.
- Collateral ligament sprain at the MCP, PIP, or DIP joint
- Volar plate injury
- Tendon rupture or laceration
- Bone bruise
- Dislocation/subluxation of the MCP, PIP, or DIP joint
Prognosis
Although the complication rate from surgically managed phalanx fractures is relatively high, the overall prognosis is quite good.[9][10][11] Most fractures go on to heal regardless of the fixation method, although a small percentage of delayed union, malunion, and nonunion has been described. Long-term complications, including decreased range of motion and deformity, are well documented.[6][8][6][9][10][11][13][14][16][17][18] Despite this, most patients have a functional recovery allowing them to return to work with most returning to the same occupation.[14][17] Few will require additional surgery to obtain fracture union or improve function.[8][9][10][11][12][14]
Complications
A moderate to high percentage of patients undergoing surgical treatment for phalangeal fractures have complications[9][10][11]. Stiffness, hardware failure, and infection are among the more common complications described.[6][8][9][10][11][12][13][14][15] Older age at the time of injury correlates with a worse final range of motion following surgical treatment.[15] Issues with healing, including delayed union, malunion, and nonunion as well as persistent pain, are also noted infrequently in the literature.[6][9][10][11][13][14][16][18][16] Although many of these complications are considered minor, a small percentage of them do require repeat surgery, including revision fixation, removal of hardware, tenolysis, and capsulotomy.[8][9][10][11][12][14]
Postoperative and Rehabilitation Care
Early motion is necessary following phalanx fractures to improve function. This generally begins as soon enough healing has occurred to consider the fracture stable and varies depending on operative intervention, often occurring within a few days of surgery.[6][8][10][17] Immobilization techniques often range from 3 to 6 weeks, though it is not uncommon to start range of motion exercise prior to the discontinuation of immobilization.[19][20] Rehabilitation ranges from self-driven home exercise programs to formal hand therapist-led protocols depending on the extent of injury, early motion limitation, and abilities of the patient.[6][10][17] A good rehabilitation program relies on communication, edema control, early motion, and scar desensitization strategies.[12]
Deterrence and Patient Education
Prevention of phalanx fractures and hand injuries, in general, involves limiting exposure and the use of protective equipment. Safety mechanisms should be used when able on doors to help prevent the exposure for children to door slam injuries. Safety equipment such as gloves and rules limiting the exposure of the hands to dangerous situations in sports can also provide for additional prevention.[1] The prevention of falls in the elderly decreases injury incidence of many types, including phalanx fractures. Proper working conditions, including safety mechanisms to ensure limbs are free from machinery with moving parts, helps to avoid crush injury in a variety of occupations. Ensuring proper methods for the involvement of worker’s compensation and open channels of communication can improve early intervention and care in these types of settings as well.
Enhancing Healthcare Team Outcomes
Phalanx fractures are often initially evaluated on sidelines of sports games, training rooms nearby to practice, primary care offices, urgent cares, and emergency departments in addition to the hand surgeon or general orthopedic surgeon’s office. A large portion of phalanx fractures is ultimately treated by primary care and emergency medicine providers.[1][2][3][5][7][16] Imaging modalities to aid in diagnosis requires the assistance and knowledge base of radiology technologists and radiologists. Patients treated both nonoperatively and surgically often require a structured hand therapy program to optimize post-injury function, which can be overseen by occupational and/or physical therapists.
Overall, a knowledgeable multidisciplinary team is necessary to properly diagnose and treat patients with phalanx fractures to optimize outcomes. A recent study showed an 8% misdiagnosis rate from emergency medicine and primary care physician referral in pediatric hand injuries.[3] Enhancing knowledge across all specialties with continued research and communication, along with shared decision making, will decrease misdiagnosis and improve patient care outcomes. [Level 5]