Blood Supply and Lymphatics
The blood supply of the upper limb arises from the arch of the aorta via the left subclavian artery on the left side and the brachiocephalic arterial trunk on the right side. The brachiocephalic arterial trunk gives rise to the right subclavian artery. Branches of the subclavian artery are the thyrocervical trunk which gives rise to the suprascapular artery, the ascending cervical artery, the inferior thyroid artery, and the cervicodorsal trunk. The internal thoracic artery and the dorsal scapular artery are also branches of the subclavian artery.
Both subclavian arteries become axillary arteries after passing over the first rib into the axilla. There are six branches of the axillary artery. The first is the superior thoracic artery, which lies medial to the pectoralis minor. The axillary artery then passes posterior to the pectoralis minor and has two branches. The first is the thoracoacromial arterial trunk, which has four branches: the clavicular, acromial, pectoral, and deltoid arteries. The second branch is the lateral thoracic, which passes posterior to the lateral border of the pectoralis minor.
The third portion of the axillary artery has three branches. The subscapular artery passes along the lateral border of the scapula, giving off (1) the circumflex scapular artery, which anastomoses with the suprascapular artery to supply the dorsum of the scapula and (2) the thoracodorsal artery to supply the latissimus dorsi muscle. The other branches are the posterior circumflex humeral artery which passes through the quadrangular space to anastomose, with the third branch, the anterior circumflex humeral artery. They form an arterial ring around the surgical neck of the humerus.
After the axillary artery crosses the lower border of the teres major muscle, it becomes the brachial artery, the main blood supply to the arm. This vessel gives rise to the deep branch of the brachial artery (profunda brachii artery), which travels with the radial nerve deep to the triceps brachii. The deep branch of the brachial artery supplies the deep muscles of the arm and becomes a network of vessels around the elbow. The brachial artery travels with the median nerve into the cubital fossa, bifurcating into the ulnar and radial arteries.[3]
These arteries provide blood supply to the remainder of the upper limb. Lesions of specific nerves which run with these arteries are of clinical and surgical significance. The following nerves and arteries are of vital importance: (1) the radial nerve, which runs with the deep branch of the brachial artery at the radial groove; (2) the axillary nerve, which runs with the posterior humeral circumflex artery and can be seen at the quadrangular space.[3]
Nerves
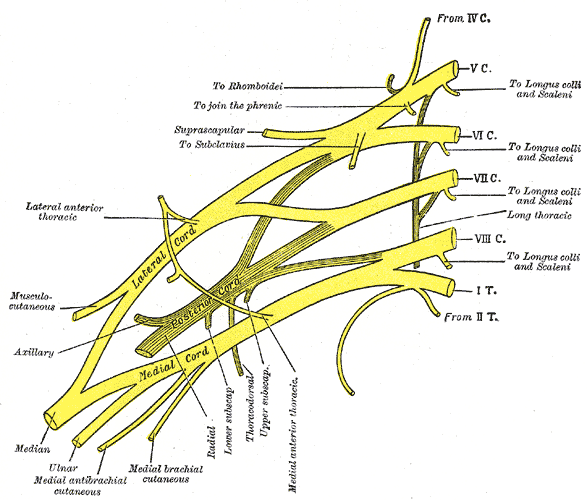
The nerves of the upper limb arise from a network called the brachial plexus, which originates in the neck from the anterior rami of spinal nerves C5-T1.[4] These are termed the roots of the brachial plexus. Note that this use of the term roots does not denote the dorsal and ventral roots of the mixed spinal nerves. The brachial plexus is divided into five sections: roots, trunks, divisions, cords, and branches. A mnemonic is "Randy Travis Drinks Cold Beer" (roots, trunks, divisions cords, branches).[5]
The C5 and C6 roots join to form the upper (superior) trunk. The C7 root forms the middle trunk. The C8 and T1 roots join to form the lower (inferior) root. These trunks pass over the first rib between the scalenus anterior and scalenus medius muscles in the interscalene triangle, where they can be injured in the scalenus anterior syndrome.
These trunks then give off anterior and posterior divisions. In general, the nerves derived from the anterior division innervate the flexor muscles of the upper limb. The nerves derived from the posterior division derivatives innervate the extensor muscles of the upper limb.
The anterior divisions of the upper and middle trunks join to form the lateral cord of the brachial plexus (C5, C6, C7). The anterior divisions of C8 and T1 form the medial cord. All 5 posterior divisions join to form the posterior cord of the brachial plexus. The lateral cord forms the musculocutaneous nerve (C5, C6, C7) and the C5, C6, and C7 portions of the median nerve. The medial cord forms the ulnar nerve (C8, T1) and contributes these roots to the median nerve (C5-T1).
There are a number of branches of the plexus proper in addition to the five terminal nerves. (1) branches from the roots of the brachial plexus; (2) branches from the trunks of the brachial plexus; and (3) branches from the cords of the brachial plexus. The five branches are the last segments of the brachial plexus. The terminal branches include the following nerves: musculocutaneous, axillary, radial, median, and ulnar. Each nerve has a distribution that coincides with the muscles they innervate.[3]
Lesions of Roots of the Brachial Plexus
The phrenic nerve (C3, C4, C5) innervates the diaphragm; a mnenonic device is "C3, C4, C5 keep your diaphragm alive." The diaphragm is critical for respiration.[6]
The long thoracic nerve of Bell (C5, C6, C7) innervates the serratus anterior. This muscle rotates the scapula allowing abduction above 90 degrees. Lesion of this superficial nerve (as in a knife fight) can cause a winged scapula (see clinical section).
The dorsal scapular nerve (C5) innervates the rhomboid major and minor, which are adductors of the scapula. They stabilize the scapula. Loss of these muscles can also contribute to developing a winged scapula. The dorsal scapular also contributes to the innervation of the levator scapulae muscle.
Lesions of the Cords of the Brachial Plexus
Other anterior division derivatives are the lateral pectoral nerve (C5, C6, C7) and the medial pectoral nerve (C8, T1). The lateral pectoral nerve arises from the lateral cord, and the medial pectoral nerve from the medial cord. The lateral pectoral nerve innervates the clavicular head of the pectoralis major. The medial pectoral nerve innervates the pectoralis minor and the sternocostal head of the pectoralis major.
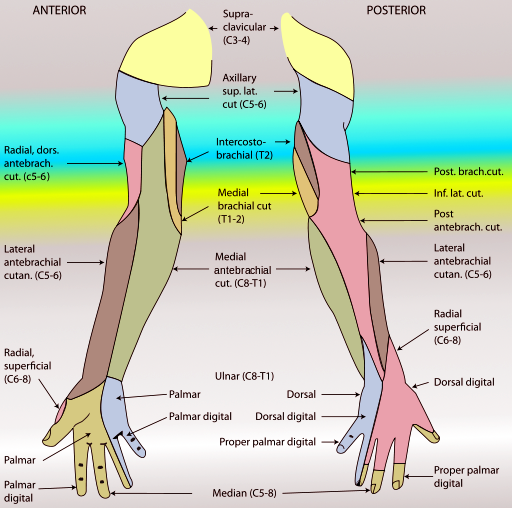
The medial cord also supplies the sensory medial cutaneous nerve of the arm (C8, T1) and the medial cutaneous nerve of the forearm.
The posterior cord gives rise to the upper subscapular nerve (which supplies the subscapularis), the thoracodorsal nerve (which supplies the latissimus dorsi), and the lower subscapular nerve (which supplies the rest of the subscapularis and the teres minor).[7]
Terminal Branches of the Brachial Plexus
Anterior division derivatives of the brachial plexus are the musculocutaneous, median, and ulnar nerves. The anterior division muscles are generally flexors of the upper limb. Posterior division derivatives are the axillary nerve and the radial nerve. The posterior division derivatives are generally extensors of the upper limb.[8]
The lateral cord is formed from the anterior division derivatives of C5, C6, and C7, and the medial cord from the anterior division derivatives of C8 and T1. The lateral cord gives rise to the musculocutaneous nerve and half the median nerve.
The medial cord gives rise to the other half of the median nerve and the ulnar nerve.
The principal branches of the posterior cord are the axillary nerve and the radial nerve.[9]
Lateral Cord Branches
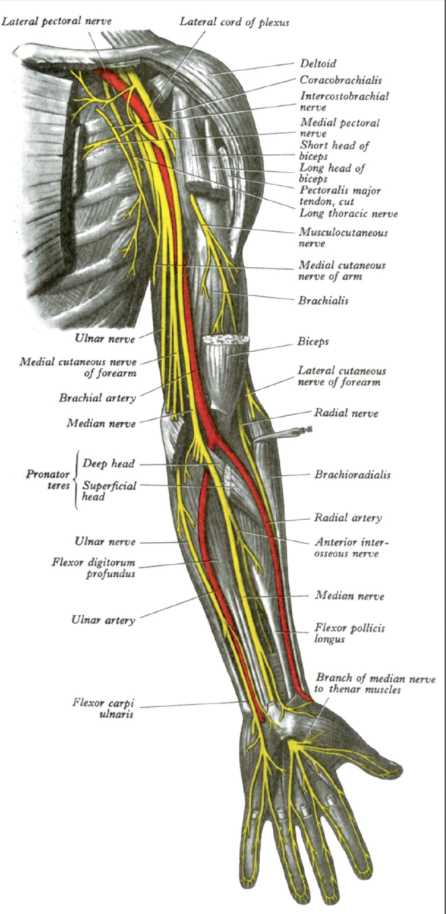
Musculocutaneous nerve - The musculocutaneous nerve (C5, C6, C7) innervates three muscles of the anterior group of the arm – the biceps brachii, brachialis, and coracobrachialis; it then forms the lateral cutaneous nerve of the forearm, which supplies sensory function of the lateral forearm as far as the wrist. However, none of the sensory nerves of the forearm (the lateral cutaneous nerve of the forearm, the medial cutaneous nerve of the forearm, and the posterior cutaneous nerve of the forearm) cross the wrist joint. The biceps brachii is a powerful flexor and supinator of the forearm at the elbow. The brachialis is a pure flexor of the forearm. The coracobrachialis is a small muscle that serves to adduct the arm at the shoulder and helps to prevent dislocation of the shoulder.[3][10]
Damage to the musculocutaneous nerve will cause loss of flexion of the forearm at the elbow and great weakness of supination of the forearm at the elbow. The biceps brachii is by far the most powerful supinator, but the continued function of the supinator prevents the complete loss of supination. The arm hangs loosely at the elbow, the function of flexion of the forearm at the elbow is lost, and supination is significantly weakened. The sensory function of the lateral forearm is lost in musculocutaneous neuropathy.
High Median nerve (elbow joint and above) - The median nerve arises from both the lateral and medial cords of the brachial plexus (C5-T1). This nerve has no branches in the arm, where it is in proximity to the brachial artery. The median nerve passes into the antecubital fossa. The superficial layer of the anterior compartment of the forearm contains the pronator teres, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris. The first three muscles of this layer are innervated by the median nerve, which passes between the two heads of the pronator teres, where it may become compressed by hypertrophy of the pronator teres (pronator syndrome – see clinical section). The nerve passes beneath the flexor digitorum superficialis, which it innervates.
The median nerve then gives off the anterior interosseous nerve, which supplies the lateral half of the flexor digitorum profundus, the flexor pollicis longus, and ends in the pronator quadratus. There are no sensory branches of the anterior interosseous nerve. The median nerve then passes beneath the flexor retinaculum into the carpal tunnel. The palmar cutaneous branch of the median nerve arises before the carpal tunnel, so it may not be involved in carpal tunnel syndrome.[11]
Low median neuropathy – wrist joint and hand - The median nerve passes through the carpal tunnel underneath the flexor retinaculum. Once past the carpal tunnel, the median nerve breaks into several branches. The recurrent branch of the median nerve passes to the thenar eminence to innervate the OAF complex: opponens pollicis, abductor pollicis brevis, and the superficial head of the flexor pollicis brevis. Sensory function is supplied by three common palmar digital branches. The first supplies the adjacent surfaces of the thumb and index finger. This nerve also supplies the first lumbrical. The second supplies the adjacent surfaces of the index and middle fingers and the second lumbrical muscle. The third supplies the adjacent surfaces of the middle and ring fingers.
Ulnar nerve – high (elbow) - The ulnar nerve is formed from the medial cord of the brachial plexus (C8, T1). The ulnar nerve innervates one and one-half muscles in the forearm: the flexor carpi ulnaris and the ulnar half of the flexor digitorum profundus (ring and little fingers). The ulnar nerve descends in the forearm beneath the flexor carpi ulnaris to pass through Guyon's canal (pisiform and hook of the hamate) at the wrist. Loss of the flexor carpi ulnaris weakens flexion of the hand at the wrist and causes radial deviation when the hand is flexed at the wrist. Flexion of the ring and little fingers is weakened due to loss of innervation of the ulnar half of the flexor digitorum profundus. The symptomatic presentation due to a loss of the ulnar nerve in the hand is described below.
There is no sensory function of the ulnar nerve in the arm and forearm. These are provided by the medial cutaneous nerve of the arm (C8, T1) and the medial cutaneous nerve of the forearm (C8, T1). Both of these sensory nerves arise from the medial cord of the brachial plexus. The fact that the medial cutaneous nerve of the forearm does not cross the wrist joint is of clinical importance.[12][13][14]
Ulnar nerve – low (Guyon's canal and hand) - The ulnar nerve passes through Guyon's canal between the hook of the hamate, the pisiform, and the pisohamate ligament. The ulnar nerve can be injured here by a fracture of the hook of the hamate. There are three branches of the ulnar nerve in the hand. The dorsal sensory branch of the ulnar nerve arises from the ulnar nerve and supplies sensation to the dorsal surface of the ulnar side of the hand. The ulnar nerve divides into motor and sensory branches within the Guyon canal.
The superficial branch of the ulnar nerve innervates the palmaris brevis and divides into a common palmar digital branch that provides sensory innervation to the adjacent sides of the ring and little fingers and a separate proper palmar digital branch that innervates the medial side of the little finger. The deep branch of the ulnar nerve innervates the abductor digiti minimi, flexor digiti minimi, opponens digiti minimi, all seven (3 palmar, 4 dorsal) interossei, and the third and fourth lumbricals. The deep head of the flexor pollicis brevis is innervated by the deep branch of the ulnar nerve, which ends by innervating the adductor pollicis muscle.
Lesions of the Posterior Divisions of the Brachial Plexus
Axillary nerve - The axillary nerve is one of the terminal branches of the posterior division of the brachial plexus, which is formed from the posterior cord that carries C5-T1. The axillary nerve passes through the quadrangular space with the posterior humeral circumflex artery to innervate the deltoid and teres minor, which then forms the upper lateral cutaneous nerve of the arm. The axillary nerve can be injured by a fracture of the surgical neck of the humerus. Lesion of the axillary nerve causes weakness of the abduction of the arm at the shoulder. The supraspinatus can initiate abduction of the arm at the shoulder, but it is not strong enough to reach the horizontal level. The deltoid can extend and laterally rotate the arm at the shoulder and has some action in flexion and medial rotation.[9]
Radial nerve - The radial nerve (C5-T1) is the larger terminal branch of the posterior cord of the brachial plexus. Even though the axillary nerve (C5, C6) is also derived from the posterior cord, it is derived from far fewer roots. The structures it innervates are located very proximally on the upper limb. This is an illustration of the proximal-distal myotome rule. A myotome is an area of muscle innervated by a single anterior (ventral) root.
The radial nerve gives off the posterior cutaneous nerve of the arm, then descends between the long and lateral heads of the triceps brachii. The radial nerve innervates all three heads (long, lateral, and medial) of the triceps brachii. The nerve then passes in the musculospiral (radial spiral) groove of the humerus between the long and medial heads of the triceps brachii. The posterior cutaneous nerve and the lower lateral cutaneous nerve of the arm are radial nerve branches.
Proximal fractures of the humerus denervate the posterior cutaneous nerve of the arm, the lower lateral cutaneous nerve of the arm, all the heads of the triceps brachii, and the rest of the branches (see below). The radial nerve then passes around the lateral epicondyle of the humerus beneath the brachioradialis and extensor carpi radialis longus, both of which it innervates. The radial nerve divides into the superficial branch of the radial nerve and the deep branch of the radial nerve. The superficial branch of the radial nerve passes beneath the brachioradialis and emerges at the wrist to innervate the hand. Branches of the radial nerve innervate the radial part of the posterior surface of the hand. A branch passes to the thumb. The radial nerve does not innervate the tips of the fingers, which are innervated by the median and ulnar nerves. Compression of this branch is part of the pain of skier's thumb.
A mid-humeral fracture denervates the branches of the radial nerve in the forearm and hand. This injury typically results in wrist drop (see the clinical section).
Fracture of the humerus at the lateral epicondyle damages the radial nerve, causing loss of the extensors of the forearm and hand, extension of the thumb, and weakness of abduction of the thumb. A lesion will result. The innervation to the brachioradialis and extensor carpi radialis longus may be spared, as these nerves are small and arise above the lateral epicondyle.
The deep branch of the radial nerve innervates the extensor carpi radialis brevis and pierces the supinator, also innervating it. The deep branch then appears under the arcade of Frohse to become the posterior interosseous nerve, which has no sensory branches. Eleven muscles are located in the posterior compartment of the forearm. Two are innervated by the radial nerve proper (brachioradialis and extensor carpi radialis longus), two from the deep branch of the radial nerve (supinator and extensor carpi radialis brevis), and seven from the posterior interosseous nerve. Of the latter, three supply the thumb (abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus). The extensor digitorum, extensor indicis, extensor digiti minimi, and extensor carpi ulnaris are also innervated by the posterior interosseous nerve).
The tendon of the extensor pollicis longus passes around the dorsal radial tubercle of Lister. The tendon of this muscle can become subject to arthritic changes and overuse syndromes. This is termed de Quervain tenosynovitis.[15][16][17]
Clinical Significance
Clinical Aspects
Proximal Lesions
Upper Trunk brachial plexus injury (Erb-Duchenne palsy)(C5, C6, C7) - involves the upper portion of the brachial plexus (C5, C6, C7). The condition most commonly occurs in obstetrical delivery and traumatic injury. In the obstetric injury, a baby is undergoing a breech delivery in which the head is abducted by pulling on the head and bending the neck, thus tearing the upper roots of the brachial plexus. In adults riding a motorcycle or a horse in which, the person is thrown to the ground and lands on the head, violently abducting the head and tearing the upper roots on the contralateral side.
A physical examination will reveal the forearm and hand to be extended at the side due to the loss of the biceps brachii and brachialis muscles. The loss of abduction also occurs but is not obvious unless the patient attempts to abduct his arm at the shoulder when the loss of the deltoid muscle becomes obvious. The arm is medially rotated due to the loss of the lateral rotators of the arm at the shoulder (posterior fibers of the deltoid, teres minor, and infraspinatus). This posture is sometimes called "a waiter taking a tip." [18][19]
Lower Trunk brachial plexus injury (Dejerine-Klumpke)(C8, T1) - This injury can occur in a difficult delivery in which the arm is delivered, but the shoulder prevents the passage of the rest of the baby down the birth canal. Thus, the arm is pulled over the head, tearing the lower roots of the brachial plexus on the same side. This injury can also be caused by falling out of a tree when the arms are violently pulled upward as the person catches a limb, or by hypertrophy of the scalenus anterior and scalenus medius muscles (scalenus anterior syndrome or thoracic outlet syndrome) and by pressure from a cervical rib.[19]
Crutch palsy - Injury to the posterior cord of the brachial plexus due to the cross-bar of an ill-fitting crutch causes loss of the extensor muscles of the arm, forearm, and hand. This syndrome involves all the muscles innervated by the axillary and radial nerves. Crutch palsy produces a wrist drop in which the hand cannot be extended at the wrist.
Winged scapula - Lesions of the long thoracic nerve of Bell cause a "winged scapula" in which the scapula is not stabilized. Lesions of the dorsal scapular nerve can also cause a "winged scapula." To test for this condition, have the patient put both palms against a wall and push hard on the wall. In a "winged scapula," the scapula will protrude from the posterior wall of the upper thorax.
Median Nerve Lesions
Pronator syndrome - This injury involves compression of the median nerve as it passes between the two heads of the pronator teres. This injury will involve sensory losses over the thumb, index, middle, and lateral half of the ring finger. Pain will also be felt in the proximal forearm over the pronator teres. This injury is seen primarily in athletes, particularly those involved in weight lifting and resistance training, which cause hypertrophy of the pronator teres. Pain is felt over the pronator teres and in the digits. The condition could produce muscle atrophy, but usually, the pain is sufficient to cause a lessening of the activity. In the most determined patients who refuse to discontinue weight lifting, one could surgically sever one of the heads of the pronator teres.[20][21]
Loss of ability to flex the middle and distal phalanges of the index and middle fingers - This condition also typically presents with weakness in flexing the ring and little fingers due to loss of all the flexor digitorum superficialis, and half the flexor digitorum profundus is consistent with injury of the median nerve in the proximal forearm.
Ape hand - Loss of the short thenar muscles due to atrophy from a lesion of the recurrent branch of the median nerve causes the thumb to appear to lie in the plane of the hand (ape hand).
Carpal tunnel syndrome. The median nerve passes through the carpal tunnel. Inflammation of the tendons from an overuse syndrome can cause loss of the innervation of the thenar muscles of the hand. In the hand, the median nerve has a recurrent branch given off to the thumb, innervating the abductor pollicis brevis, flexor pollicis brevis (superficial head), and opponens pollicis.
The median nerve gives off three common palmar digital nerves. The first nerve branch innervates the first lumbrical and sensory function to the adjacent sides of the thumb and index finger. The second innervates the second lumbrical and provides sensation to the adjacent sides of the index and middle fingers. The third provides sensation to the adjacent sides of the middle and ring fingers. The tips of the three and-one-half digits also supply the pads of the digits.
One can have the patient attempt to oppose the pads of the little finger and thumb ("OK" sign). Both the recurrent branch of the median nerve (oppositions pollicis) and ulnar nerve (opponens digiti minimi are required for this maneuver. Loss of the ability to oppose the thumb is consistent with carpal tunnel syndrome. This can also be produced by a rather superficial cut in the hand about halfway up the thenar eminence. There are no sensory losses in a lesion of the recurrent branch of the median nerve, so it is imperative to determine whether the thumb can be opposed to the little finger.[22][23][24][25]
A superficial lesion can produce lesions of the recurrent branch of the median nerve. Have the patient demonstrate opposition of the thumb by placing the pad of the thumb against the pad of the little finger (OK sign). Sensory function to the midportion of the thenar eminence may be spared because the palmar branch of the median nerve arises before the flexor retinaculum and is, therefore, not involved in carpal tunnel syndrome.
Hand of papal benediction (preacher's hand) - When the patient attempts to make a fist, the index and ring fingers remain extended. This is due to loss of innervation from the anterior interosseous nerve of the median nerve and the median nerve proper (high median neuropathy). Alternatively, a lesion of the median nerve proximal to the origin of the anterior interosseus nerve will produce the same result. A supracondylar fracture of the humerus can produce this result as well. Some weakness of pronation may also occur due to loss of the pronator quadratus (anterior interosseous nerve), and pronator teres (high median neuropathy) due to a high median neuropathy before the anterior interosseous nerve is given off.
Radial Nerve Lesions
Wrist drop - The hand is flexed at the wrist and cannot be extended. To test for a wrist drop, have the physician support the forearm in the flexed position and ask the patient to extend the hand at the wrist. A radial nerve lesion at any level above or in the forearm will cause an inability to extend the hand at the wrist. If the posterior interosseous nerve alone is damaged, there will be a weak extension of the hand accompanied by radial deviation.[26]
de Quervain's tenosynovitis - This condition involves pain over the tendon of the extensor pollicis longus. The test for this condition is termed the Finkelstein maneuver. Have the patient flex the thumb and flex the fingers to cover the thumb. When these are tightly gripping the thumb, have the patient adduct (ulnar or medial deviation) of the hand somewhat forcibly. If this maneuver causes hand pain in the thumb, de Quervain's tenosynovitis is probably the correct diagnosis.[15][16][17]
Ulnar Nerve Clinical Syndromes
Ulnar Nerve Lesions
Ulnar nerve (C8, T1) injury - These injuries arise from the medial cord of the brachial plexus, where it passes behind the medial epicondyle and is subject to damage from a medial epicondyle fracture. This injury causes loss of medial deviation of the hand (flexor carpi ulnaris), weakness of flexion of the ring and little fingers (due to loss of the medial portion of the flexor digitorum profundus), and the symptoms of the lower ulnar neuropathy (Guyon's canal syndrome).
Cubital tunnel syndrome - This condition involves the ulnar nerve, medial epicondyle, the ulnar collateral ligament, and the heads of the flexor carpi ulnaris.[27] This is similar to a fracture of the medial epicondyle, which will damage the ulnar nerve. A milder version is the student's palsy, in which the elbows rest on a desktop while the student studies for hours. This latter version is usually limited to numbness without atrophy because the pain and numbness are sufficient to draw attention to the condition.
Guyon canal syndrome - This syndrome causes loss of innervation if the dorsal and palmar interossei, opponens digiti minimi (opposition of the little finger), abductor digiti minimi (abduction of the little finger), and flexor digiti minimi (flexion of the little finger – but flexor digitorum superficialis and profundus prevent any real weakness of flexion of the ring and little fingers). The digital palmar sensory nerve serves sensation to the adjacent surfaces of the ring and little fingers and the medial surface of the little finger: third and fourth lumbricals, deep head of flexor pollicis brevis, and adductor pollicis. The deep ulnar nerve supplies the third and fourth lumbricals, all seven interossei, the deep head of the flexor pollicis brevis, and the adductor pollicis.
Testing for the Adductor Pollicis
Have the patient hold a piece of paper between the thumb and the index finger while the examiner tries to remove it. Loss of the ulnar nerve causes the inability to retain the paper. Loss of the deep branch of the ulnar nerve causes loss of the adductor pollicis and first dorsal interosseous. When the patient attempts to hold the paper, he uses the flexor pollicis longus because the adductor pollicis is not functional. This causes flexion of the distal phalanx of the thumb due to the action of the flexor pollicis longus (Froment's sign).
Sensory losses from the ulnar nerve in the hand - These injuries are confined to the adjacent surfaces of the ring, little fingers, and the medial side of the hand. The dorsal surface of the medial hand will be denervated due to the loss of the dorsal branch of the ulnar nerve.
"Claw hand" - This condition results from a lesion of the ulnar nerve either at the elbow or more proximally. In diagnosing this condition, have the patient rest the hand on supported on a desk or other surface and observe the ring and little fingers. The fingers will be hyperextended at the metacarpophalangeal joint due to the action of the unopposed long extensors. The absence of lumbricals 3 and 4 acting with the long extensors causes the extension of the phalanges at the interphalangeal joints. The fingers will be flexed at the interphalangeal joints due to the action of the intact flexor digitorum superficialis and profundus. Wasting and atrophy of the hypothenar eminence and loss of adduction of the thumb will also be present.
Testing for loss of the adductor pollicis - Have the patient try to retain a piece of paper between the thumb and index finger while the examiner pulls on it. The patient will be unable to retain it because of loss of the adductor pollicis. However, he will flex the thumb at the interphalangeal joint with the flexor pollicis longus. No thought is involved in the response.
Testing the interossei 1 - Have the patient hold a piece of paper between his index and ring fingers (served by the first palmar and second dorsal interossei). If the patient cannot retain the paper when the examiner pulls on it, a lesion of the deep branch of the ulnar nerve (or ulnar nerve proper at higher levels) is present.
Testing the interossei 2 - The examiner holds the patient's hand, squeezing the fingers and thumb. Determine whether the patient can abduct the fingers against resistance.[18][5]