Continuing Education Activity
Folliculitis is a common skin condition that usually involves infection of the hair follicle. While this condition is typically benign, prompt recognition can aid in the improvement of quality of life of patients with this condition. This activity reviews the evaluation and treatment of folliculitis and highlights the role of the interprofessional health care team in evaluating and treating patients with this condition.
Objectives:
- Outline the etiology of different forms of folliculitis.
- Review common history and physical exam findings in patients with folliculitis.
- Summarize the different treatment options for each listed type of folliculitis.
- Explain the importance of collaboration and communication among the interprofessional team to enhance the delivery of care for patients affected by folliculitis.
Introduction
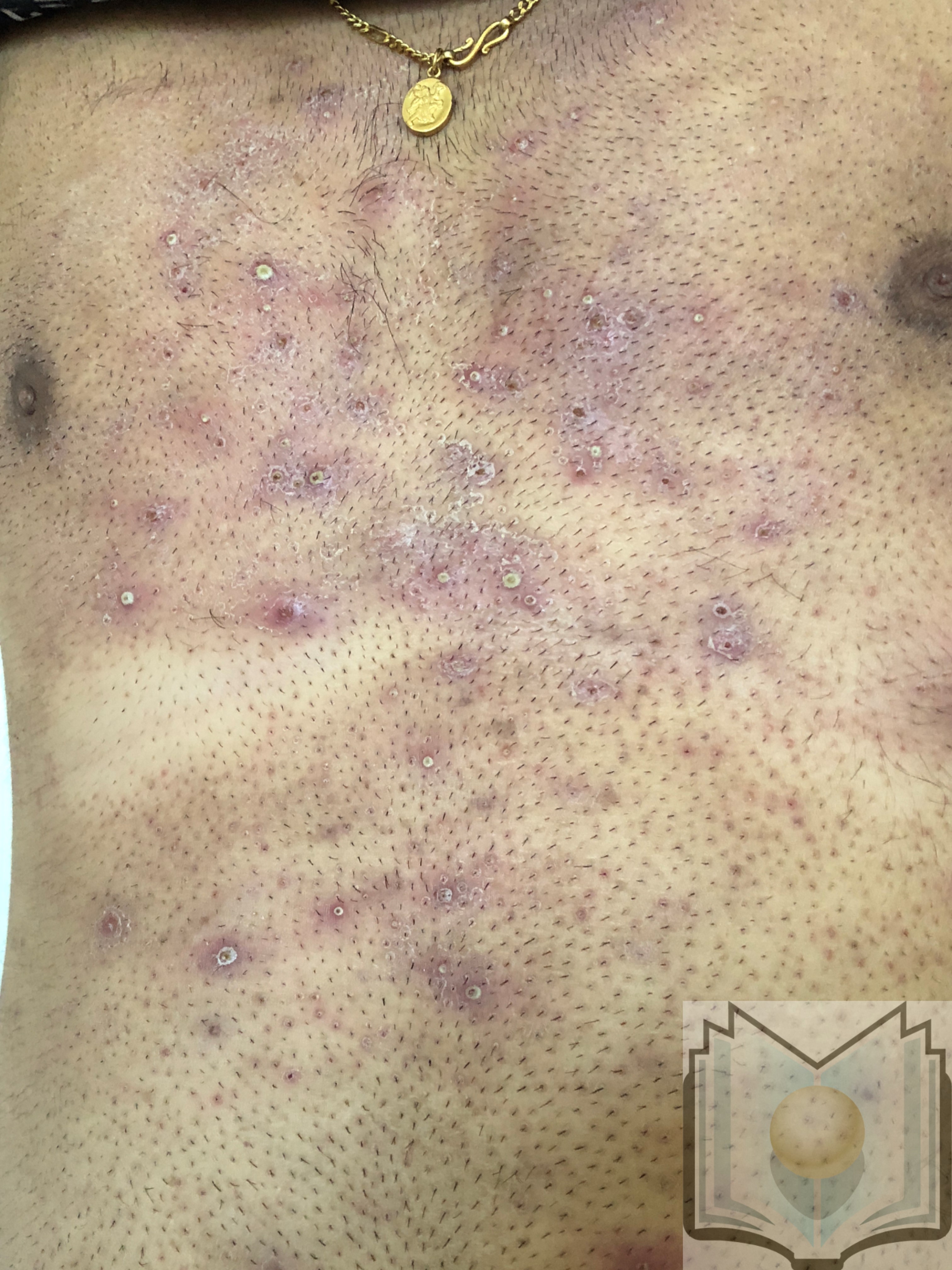
Folliculitis is a common, generally benign, skin condition in which the hair follicle becomes infected/inflamed and forms a pustule or erythematous papule of overlying hair-covered skin. While this is a non-life threatening condition and in most cases is self-limited, it can present challenges for immunocompromised patients and in some cases progress to more severe diseases.[1]
Etiology
Most commonly, folliculitis is caused by bacterial infection of the superficial or deep hair follicle. However, this condition may also be caused by fungal species, viruses and can even be noninfectious in nature. Several of the causative agents of folliculitis are listed below and include:
Superficial bacterial folliculitis – The most common form of folliculitis, this particular condition is usually caused by the bacteria Staphylococcus aureus. It should be noted that both the methicillin-sensitive and methicillin-resistant forms of this bacteria can cause folliculitis.[1]
Gram-negative bacterial folliculitis - Commonly referred to as “hot tub” folliculitis, this condition results from the bacteria pseudomonas aeruginosa. It typically arises after exposure to contaminated water from either an improperly treated swimming pool or hot tub. Other bacteria that may cause this condition include Klebsiella and Enterobacter. Folliculitis from these bacteria commonly arises after long-term use of oral antibiotics.[2][3]
Pityrosporum Folliculitis - This particular form of folliculitis is fungal, caused by the Malassezia species of fungi such as Malassezia furfur. Typically found in adolescence secondary to increased activity of their sebaceous glands, and is commonly found in a cape-like distribution over the patient’s shoulders, back, and neck. Clinical suspicion of this condition should arise in patients diagnosed with acne that has failed to respond or even worsened, after antibiotic treatment.[4]
Viral folliculitis - Most commonly caused by herpes virus it could also be caused by Molluscum contagiosum, but this is far rarer. Folliculitis due to herpes virus presents in much the same way as bacterial folliculitis with the exception that papulovesicles and/or plaques are usually present and not pustules. Another key to the diagnosis of this condition is that lesions typically appear in either groups or clusters.[5]
Demodex folliculitis - a type of folliculitis caused by the mite Demodex folliculorum. This particular type of folliculitis is controversial as the Demodex mite normally presents in the pilonidal sebaceous area of the skin. Estimates are that 80 to 90% of all humans may carry this mite.[6]
Eosinophilic folliculitis - This particular brand of folliculitis is found predominantly in those with advanced HIV or those with low CD4 counts.[7] Although a non-HIV variation of this condition has been seen as a rare side effect in patients undergoing chemotherapy.[8] While the exact etiology of this condition is unknown, studies suggest it could result from inflammatory disease secondary to immune dysregulation and that there may be an associated underlying infection.[9] Most commonly, this condition presents as erythematous and urticarial follicular papules, usually on the scalp, face, and neck with rare pustules.
Epidemiology
While the precise incidence of folliculitis is not currently known, we do know that patients who have a history of diabetes, obesity, prolonged use of oral antibiotics, are immunosuppressed/immunocompromised or who shave frequently are at risk for developing this condition. While gender does not correlate with an increased incidence of folliculitis, there may be a correlation between the type of folliculitis and gender. For example, Malassezia folliculitis is commonly seen in men more than women.[4]
Pathophysiology
Most commonly, infection of the hair follicle is the mechanism behind most folliculitis cases. Even so, folliculitis may also result from fungal or viral infections, but this does not mean that all folliculitis cases are infectious. Sometimes, folliculitis may be the result of inflammation secondary to ingrown hairs as well as caused by certain drugs such as lithium and cyclosporine.
Histopathology
In the vast majority of cases of folliculitis, histopathology is not needed for diagnosis as this condition is a clinical diagnosis. However, in the case of eosinophilic folliculitis skin biopsy should be done for confirmation of the diagnosis. These biopsies would show perifollicular infiltrates that include lymphocytes and eosinophils predominantly around the area where the sebaceous gland and duct meet follicle. Uncommonly, the clinician may need to perform a skin biopsy to differentiate folliculitis from a condition that may mimic it. In cases of bacterial folliculitis, a biopsy would show a neutrophilic invasion of the hair follicle.
History and Physical
A complete history, as well as a focused physical exam, is usually enough to elucidate the diagnosis. Essential elements of history should include[10]:
- Recent increase of scratching due to pruritus
- History of increased sweating
- Use of topical corticosteroids
- Recent and/or long term use of oral antibiotics
- Any hot tub and/or swimming pool exposure
- History of HIV with CD4 count less than 250 or immunosuppression (ex. A patient who recently had a transplant that’s on immunosuppressive drugs)
Physical exam should include close inspection of hair-bearing areas, including the bilateral upper and lower extremities as well as the chest, back, face, and scalp. On exam, the clinician should look for small pustules in these areas with peri-follicular inflammation.
Evaluation
The diagnosis of folliculitis is clinical. In general, no diagnostic testing or radiographic evaluation is necessary to diagnose this condition in lieu of a thorough history and physical exam. A standard KOH preparation can be used to visualize hyphae and spores associated with folliculitis caused by Malassezia. KOH preparation could also be used to diagnose Demodex folliculitis; however, this is not common in clinical practice.[11][6] Also, a skin biopsy is usually required to confirm the diagnosis of eosinophilic folliculitis.
Treatment / Management
Staphylococcal folliculitis - most simple cases of staph folliculitis with few pustules will resolve spontaneously within a few days. However, for more extensive disease, topical antibiotics can be an option. First-line agents typically include topical mupirocin and clindamycin. Should these prove ineffective or should the patient present with deeper folliculitis such as furunculosis and carbunculosis or more extensive involvement of the skin, then oral antibiotics such as cephalexin and dicloxacillin are options.[12][13]
Gram-negative folliculitis - Much in the same way as staph folliculitis, simple cases will generally resolve spontaneously after 7 to 10 days with good skin hygiene. In certain cases where this is seen secondary to prolonged antibiotic use, oral antibiotic treatment that covers for pseudomonas are possible choices including ampicillin, trimethoprim-sulfamethoxazole, and ciprofloxacin all being first-line agents.[14]
Pityrosporum Folliculitis - systemic therapy with oral antifungal agents, is often the treatment of choice for this condition. Although topical antifungals are an option, the belief is that systemic therapy can’t eliminate the Malassezia fungus deeper within the follicle than can topical therapies. Itraconazole and fluconazole are the two treatments of choice for this condition. Although there is more evidence for the effectiveness of itraconazole for treating this condition, fluconazole is often the treatment of choice secondary to its better side effect profile.[15]
Viral folliculitis - folliculitis secondary to infection with herpes simplex virus may receive treatment in the same way as a normal outbreak of herpes with oral acyclovir, valacyclovir, and famciclovir. In the same way, folliculitis secondary to molluscum contagiosum infection may be treated the same as an outbreak of molluscum with either curettage or cryotherapy. Cantharidin is a topical agent that can be used to treat molluscum folliculitis. However, this drug is not available in the United States.[14]
Demodex Folliculitis – anti-parasitic agents, are the treatment of choice for this particular brand of folliculitis. Treatments such as topical permethrin as well as oral ivermectin and oral metronidazole are therapeutic options. One study found that dual therapy with oral ivermectin/oral metronidazole could be more effective than monotherapy of either drug alone. Although, topical permethrin 5% cream is usually the initial treatment of choice.[16][17]
Eosinophilic folliculitis - in general, the first-line treatment for this condition is antiretroviral therapy to treat the patient’s underlying HIV. In the vast majority of patients, treatment of the underlying HIV which show improvement or even resolution of this condition. Although some patients may have a flare of this condition during the first six months after ART initiation. In these cases, patients may be treated with optional therapies for a few weeks to months which include topical corticosteroids, antihistamines, phototherapy, and even itraconazole or isotretinoin.[18]
Differential Diagnosis
- Acne vulgaris
- Papulopustular rosacea
- Drug-induced folliculitis
- Hidradenitis suppurativa
- Scabies
- Pseudofolliculitis barbae
- Keratosis pilaris
- Acne keloidalis nuchae
Prognosis
As this condition is generally benign and often self-limiting, the outlook and prognosis are very good for a full recovery. With proper hygiene and management of any underlying conditions, recurrence rates can remain minimal.
Complications
- Progression to a more severe skin condition such as cellulitis or abscess
- Medication side effects (drug allergies or adverse drug-drug interactions)
Deterrence and Patient Education
In the vast majority cases of folliculitis, the only therapy needed is time, as most cases will resolve spontaneously. More severe cases can be managed medically with either antibiotic, antifungal, or anti-parasitic agents. Patients should be counseled on proper hygiene for the affected area as well as the use of warm compresses several times daily for up to 15 minutes on the affected area. Patients should also receive counsel against scratching or shaving the affected areas as this could cause increased irritation and could potentially spread the causative agent.
Enhancing Healthcare Team Outcomes
Folliculitis is a very common condition that can easily be identified by all members of the healthcare team, including primary care physicians, nurse practitioners, physician assistants, and nursing staff. All of these individuals can play essential roles in the diagnosis and patient education of this condition.
Proper hygiene is of paramount importance to prevent recurrence as well as to facilitate the resolution of this condition. In more severe cases, medical therapy may be necessary. In these cases, the local pharmacist can be consulted to help determine correct coverage for the underlying causative agent for these patients. However, most cases of folliculitis are self-limiting and will resolve on their own with proper home care.
Should these cases prove to be too extensive, do not resolve on their own, or don’t resolve after medical management referral to a dermatologist is recommended. A pharmacist can also offer a consult on two fronts; they can verify whether the patient's medication regimen has any drugs that could result in folliculitis, and they can also assist in agent selection, antimicrobial coverage assessment, and perform additional patient counseling. Nursing must also have involvement, including monitoring for treatment effectiveness, counseling on the application of topical agents, and looking for signs of adverse drug reactions. While folliculitis is a generally benign, self-limiting condition, this does not preclude the involvement of an interprofessional team approach to diagnosis and management, resulting in better patient outcomes. [Level V]