Continuing Education Activity
Femoral neck fractures are extremely common, demonstrating a bimodal distribution pattern. Intracapsular femoral neck fractures account for approximately 50% of all hip fractures. Intracapsular fractures demonstrate limited healing potential due to the absence of the periosteal layer, so the fracture is only immersed in the surrounding synovial fluid. These injuries occur secondary to low-energy falls in older individuals and higher-energy traumatic mechanisms in younger patients. However, most of these fractures occur in older people with underlying osteoporosis.
This activity for healthcare professionals is designed to enhance learners' competence in determining surgical indications in femoral neck fracture cases. Learners gain a deeper understanding of this condition's intricacies, from its causes and classifications to its diagnostic and treatment modalities. Participants attain proficiency in recognizing the clinical presentations of these injuries and managing them according to evidence-based guidelines, preparing them to work within an interprofessional team caring for affected individuals.
Objectives:
Determine the surgical indications in a patient with a femoral neck fracture.
Create a clinically guided diagnostic plan for a patient with a suspected femoral neck fracture.
Develop a personalized management plan for an individual diagnosed with a femoral neck fracture.
Collaborate with the interprofessional team to educate, treat, and monitor patients with femoral neck fractures to enhance patient outcomes.
Introduction
Femoral neck fractures (FNFs) pose a complex and multifaceted orthopedic challenge, necessitating a nuanced understanding to navigate their diagnosis, treatment, and subsequent management effectively. These fractures occur at the critical junction between the femoral shaft and head, representing not only a physical disruption but also a significant threat to the functional independence and overall well-being of affected individuals. FNFs are among the most common fractures in older populations, with a mortality risk at 1 year reaching 36%.[1][2] Managing these injuries also entails a significant financial and societal burden.
FNFs demonstrate a bimodal distribution pattern, with low-impact injuries affecting older people and high-force trauma involving younger individuals. However, most FNFs are seen in older populations, with osteoporosis, female gender, chronic smoking, and low body mass index further increasing the risk.[3][4] Understanding the surgical management options for FNFs and their specific indications is essential in improving patient outcomes.
Anatomy and Physiology
Hip Joint Anatomy
The hip joint is a ball-and-socket joint formed by femoral head articulation with the pelvic acetabulum of the pelvis. This joint allows for a wide range of motion, including flexion, extension, abduction, adduction, and rotation. The femoral neck is a crucial part of the femur, connecting the femoral head to the femoral shaft. This region is prone to fractures, particularly in the elderly population due to osteoporosis. The iliofemoral, pubofemoral, and ischiofemoral ligaments stabilize the hip joint. These fibrous structures maintain hip stability and prevent dislocations.
Intracapsular FNFs account for approximately 50% of all hip fractures. Most of these injuries occur in older individuals with underlying osteoporosis.[5][6]
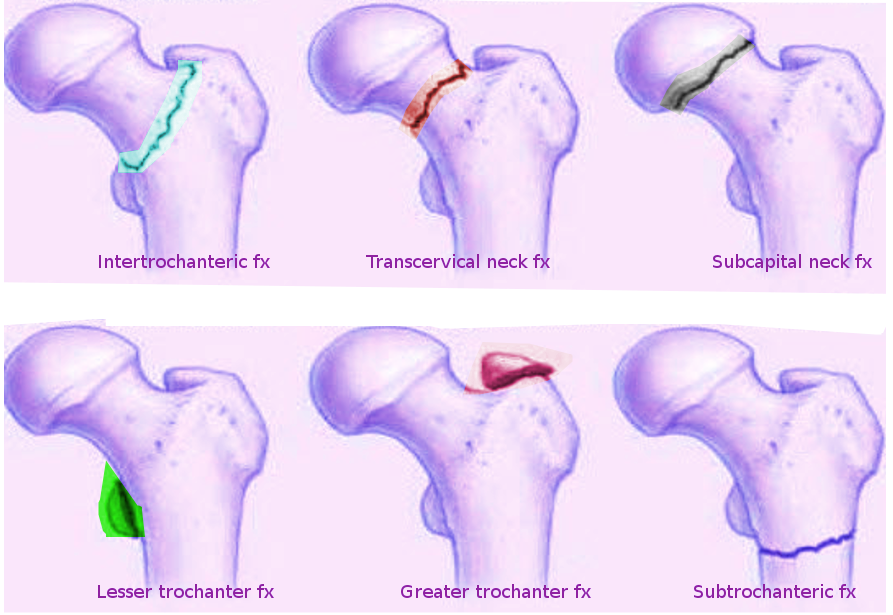
FNFs are differentiated from extracapsular hip fracture patterns based on anatomic location (see Image. Femoral Hip Fractures). Distinguishing these injuries is critical. Intracapsular fractures have limited healing potential as they lack a vascular periosteal layer and depend only on the nutrient-depleted synovial fluid for their structural maintenance and metabolic needs. The hip joint capsule attaches to the intertrochanteric line anteriorly and the iliac crest posteriorly.[7] Preserving the hip joint capsule in the context of an intracapsular FNF theoretically poses a risk of compromised blood supply to the femoral head due to elevated intraarticular pressures. A tamponade effect that compromises femoral head perfusion has been demonstrated in previous studies.[8]
The femoral head's arterial supply arises from 3 main sources. The first is the profunda femoris artery, which branches into the medial (MFCA) and lateral circumflex femoral arteries (LFCA). The MFCA is the femoral head's predominant contributor through the lateral epiphyseal artery. The LFCA supplies portions of the anterior and inferior femoral head. Retinacular vessels branching from the circumflex arteries also feed the femoral head.
The second is the ligamentum teres, a predominant arterial contributor in pediatric patients that loses importance in adult patients. The third is comprised of minimal contributions from the medullary canal and inferior gluteal artery.[9][10] Besides the tamponade effect potentially compromising femoral head blood flow, patients with FNFs risk developing avascular necrosis (AVN) due to retrograde flow and injury to the retinacular vessels.[11]
The hip joint receives innervation from branches of the femoral, obturator, and sciatic nerves. These nerves provide sensation to the joint and motor function to the surrounding muscles.
Treatment Implications
Displaced intracapsular FNFs in older people are typically managed with hip reconstruction procedures. The femoral head and neck are replaced with a reconstruction prosthesis. These procedures typically include hip hemiarthroplasty or total hip arthroplasty (THA). Nondisplaced fractures may be managed with fixation using cannulated screw fixation.
In contrast, extracapsular fractures rarely compromise the femoral head and neck's arterial circulation. Thus, a broader array of surgical fixation techniques may be used to manage these injuries. Femoral head AVN is very rare following extracapsular fractures.[12]
Indications
General Concepts in FNF Management
The interprofessional approach is often necessary in managing FNFs due to the presence of comorbidities in older patients. Notably, surgery is nearly always indicated for patients presenting with an FNF.[13] The surgical goals include pain control, mobility and function recovery, and osseous healing.[14]
Femoral Neck Fracture Nonoperative Management Indications
Nonoperative management is rarely indicated in FNFs due to the unacceptably high complication rates. Nonoperative management is reserved only for nonambulatory patients with significant medical comorbidities.[15] The primary management goals are pain control and gradual mobilization.
Patients often experience pain on ambulation, likely from forming a functional pelvic girdle stone. Pain management and immobilization are important in the initial stages after the injury. Mobilization may be attempted after callous formation weeks after the injury. The risks associated with nonoperative management include increased rates of pulmonary dysfunction, pneumonia, urinary tract infections, pressure sores (eg, sacral decubitus ulcers), deep vein thrombosis (DVT), and venous thromboembolism (VTE) from immobilization.
Femoral Neck Fracture Surgical Management Indications
FNFs pose significant challenges due to their propensity for AVN and nonunion. Surgical intervention realigns fractured bone fragments, stabilizing the fracture site and promoting optimal healing. The different FNF procedures and their indications are discussed below.
Hemiarthroplasty and Total Hip Arthroplasty
Hemiarthroplasty, or femoral head replacement, is recommended for displaced intracapsular FNFs, especially in older patients with low activity levels. THA is preferred for patients with intact ambulatory function or evidence of hip pain and degenerative arthritis. Implant design and surgical technique advances have been developed despite the higher risk of hip dislocation associated with THA for FNFs.[16][17] For active elderly patients with these fractures, using a dual mobility cup during THA reduces dislocation rates and improves functional outcomes without increasing mortality or morbidity compared to hemiarthroplasty.[18]
Girdlestone resection arthroplasty (GRA) may be an option for patients who are unsuitable for hemiarthroplasty due to conditions like systemic infections or severe neurological impairment. However, a retrospective study from Germany reported that patients with hemiarthroplasty after FNF had higher survival and better functional outcomes when compared with GRA in matched patient groups. Thus, the recommendation is to use GRA for FNFs selectively.[19]
Cannulated Screw Fixation
Cannulated screw fixation is indicated in nondisplaced, intracapsular FNFs in older patients and displaced fractures in younger people with ideal bone quality. The technique consists of inserting 3 or 4 cannulated screws in an inverted triangle or diamond configuration, respectively. Outcome differences are not significantly different between procedures using 3 and 4 screws. However, the literature suggests better results with inverted triangle fixation than techniques using only 2 cannulated screws. Recently, the biplane double-supported screw fixation method has been described for FNFs.[20][21]
In Swedish patients aged at least 75 years, a retrospective study reported that reoperation-free survival 1 year after sustaining an undisplaced FNF was similar whether internal fixation or arthroplasty was performed. However, reoperations were more common after internal fixation, and early deaths were seen more frequently after arthroplasty.[22]
Critical utilization of partially threaded (long or short thread options) screw options should be preoperatively planned before the procedure begins. The surgeon should plan on optimizing the "lag by design" technique. Recently, a femoral neck system implant has been described for the internal fixation of FNFs in young patients with theoretical biomechanical advantages compared to other implants.[23][24]
Sliding Hip Screw Fixation
The sliding hip screw (SHS) fixation construct is comprised of a large, cancellous lag screw that passes from the lateral, proximal femur across the fracture site and ends near the femoral head's center. The lag screw dynamically slides inside an incorporated metal sleeve, with the latter being connected to a fixation plate that subsequently is secured with multiple screws to the proximal femur. The compression mechanism is amenable and may be used in stable, intertrochanteric hip fractures, basicervical FNF patterns, and vertical FNFs. SHS fixation is superior to cannulated screw fixation in younger patients with vertical fracture patterns.
The fracture can be compressed as weight-bearing forces transfer from the appendicular skeleton through the pelvis and femoral head and neck before propagating distally. Thus, the SHS fixation construct allows for longitudinal sliding and compression as the patient ambulates postoperatively. The fracture compresses down as the lag screw slides into the barrel and further promotes healing.[25]
Contraindications
Sliding hip screw fixation constructs are contraindicated in the following fracture patterns due to instability:
- Reverse obliquity
- Transtrochanteric involvement
- Comminuted fracture patterns with a large posteromedial fragment, as the medial calcar buttress is absent
- Fracture patterns with subtrochanteric extension [26]
Hemiarthroplasty and THA are contraindicated in patients with an active hip infection.
Equipment
All surgical femoral neck procedures require a standard orthopedic tray and should be carried out in an operating theatre equipped with laminar flow. For cannulated screw fixation and SHS, all procedures require the necessary implants, a radiolucent traction table or flat Jackson operating table, and an image intensifier. For hemiarthroplasty and THA, a standard operating table may be used if it has the necessary side supports. Other necessities include a complete implant set and, when applicable, the instruments and materials that allow for incorporating cement fixation. Computer navigation and robotics are increasingly being utilized in THA.[27]
Personnel
The key personnel involved in FNF surgeries include the operating surgeon and assistant, anesthetist, operating department practitioner, scrub nurses, and circulating staff. A radiographer must also be present during SHS and cannulated screw fixation.
Preparation
A complete history, physical examination, and appropriate anteroposterior and lateral (APL) hip and pelvis radiographs must be obtained before the procedure. Routine preoperative lab results should be checked, including a complete blood count, basic metabolic panel, and blood typing, screening, and cross-matching. Other routine preoperative examinations include a chest radiograph and electrocardiogram. The anesthesiologist must review the patient's clinical findings and diagnostic results when deciding between spinal and general anesthesia. Preoperative medical service comanagement may include additional consultation services, eg, internal medicine or cardiology, depending on the pertinent medical comorbidities' severity.
Preoperative optimization is essential for patients with comorbidities. Healthcare providers must carefully assess whether these individuals are taking anticoagulants, which may necessitate reversal with vitamin K, or, in patients taking warfarin, fresh frozen plasma. Available reversal agents vary by country and geographic region.
The patient should sign consent forms and be identified appropriately before surgery. Once in the theatre, the World Health Organization checklist should be completed. The patient must be positioned as detailed below and appropriately prepped and draped. Surgical procedures must be finished as soon as possible for better outcomes.[28]
Positioning During Sliding Hip Screw and Cannulated Screw Fixation
For these procedures, the patient is placed supine on a radiolucent traction table. The foot on the side to be operated on must be in a traction boot. The unaffected side is placed in the lithotomy position, strapped in a leg holder, and placed in flexion, abduction, and external rotation to ensure the radiographic C-arm can access the fracture site appropriately. Gentle traction and internal rotation should be applied to reduce the fracture. Slight abduction may be needed to reduce any varus malalignment. The fracture should be nearly anatomically aligned, with radiographic confirmation, before prepping and draping. Open reduction may be necessary if closed reduction is not possible.
Correct lower extremity rotational alignment is imperative. The patient should be positioned with the patella facing toward the ceiling.[26]
Positioning During Hemiarthroplasty or Total Hip Arthroplasty
For these procedures, the patient is placed in a lateral decubitus position with support over the anterior superior iliac spine and sacrum. The pelvis should be at 90° to the table. The preoperative radiographs must be reviewed to assess offset or the distance between the femoral head's center and a line drawn down the middle of the femur. The femoral head size should match the patient's own as closely as possible.[29]
Technique or Treatment
Sliding Hip Screw
For the incision, a direct lateral approach is performed. The skin incision typically begins parallel to the lesser trochanter and extends along the femur, progressing distally. A longitudinal incision through subcutaneous fat is made afterward. The next layer is the fascia lata, cut parallel to the skin incision to reveal the vastus lateralis. The epimysium is then incised. The vastus lateralis can be lifted off the lateral intermuscular septum but is more commonly split along its fibers.
When exposing the femur, a periosteal elevator (Bristow) is used to clear muscle from the bone. A clear surface is thus left for the plate without soft tissue interposition. One or two self-retaining retractors may help gain adequate exposure for guidewire placement.
During guidewire insertion, a guidewire jig is placed on the femoral shaft. The jig must be aligned properly on the femur's lateral aspect, ensuring equal anterior and posterior distances. During guidewire placement, the wire's tip must be visualized in its eventual position in the femoral head. The lesser trochanter usually marks the entry level for a 135° angle plate. The tip should be within the subchondral bone. The position should be continually assessed using an image intensifier. A measuring device is slid over the guidewire, ensuring it sits on the bone. Typically, 5 to 10 mm are deducted from the measurement.
The guidewire is then over-drilled with a triple reamer to create a channel for both the lag screw and plate barrel. Reaming extends to the depth selected for the screw. Radiography must show that the reamer's 3rd part has engaged with the bone cortex, and the guidewire is not advancing into the pelvis.
Tapping the bone is beneficial in young patients or those with strong bones. Tapping is a process that creates a threaded hole in the bone using a tapping instrument. This process helps ensure implants are correctly placed and securely fit, especially in patients with strong or dense bones.
The lag screw is then applied over the wire and screwed in using the attached handle. The handle's final position should be parallel to the femur to ensure the lag screw will slot into the plating barrel. The plate is then slid over the lag screw. The plate template may be needed to ensure the plate is fully advanced. The guidewire can now be removed. The plate may be secured to the femur using a clamp.
The screws are inserted next. The most distal screw is conventionally placed first. The 3.5-mm drill is used with the neutral drill guide to make the screw holes, drilling through both cortices. The screw holes are then measured using the depth gauge, and the appropriate screw is inserted.
Final APL radiographs should be obtained. The wound is washed, and closure is performed in layers.[30]
Cannulated Screw Fixation
Reduction is usually not needed in this procedure, as screws are typically used for nondisplaced fractures. Similar to SHS, a direct lateral approach is taken with a longitudinal incision made at the level of the lesser trochanter. However, the incision is typically much smaller, usually around 5 cm.
Three guidewires are then inserted using a guide or freehand, depending on the surgeon's preference and experience. The typical formation is an inverted triangle with 1 screw distally and 2 proximally placed. The 1st guidewire's entry point should be no lower than the lesser trochanter to reduce the risk of forming a stress riser, which may trigger a comminuted subtrochanteric fracture. Ideally, the guidewire should sit just above the calcar on anteroposterior view and go up to the subchondral bone in the femoral head. The 2nd guidewire is placed superiorly and posteriorly to the 1st. On lateral view, this guidewire should lie next to the posterior cortex. The 3rd wire is placed superiorly and anteriorly to the 1st wire, ideally sitting parallel to the 2nd guidewire on anteroposterior view. All 3 should be within 5 mm of the subchondral bone.
The measure ascertains which screw length will be used. A cannulated drill is then used to ream over the guidewires, usually 5 to 10 mm short of the measured distance. Three partially threaded screws are then inserted before a wire driver is used to remove the guide wires. The screw measurement is typically the same as the original guidewire measurement. The screw threads should be beyond the fracture site to ensure that adequate compression takes place. The screws should be tightened together to ensure uniform compression. Depending on surgeon preference, washers may be used to increase compression further.
Final APL images should be taken. The wound should be washed with normal saline and closed in layers.[30]
Hemiarthroplasty
This operation may be approached in different ways.[31] The anterolateral approach, also known as the modified Hardinge approach, is most commonly used. A longitudinal incision over the greater trochanter is made, usually around 20 cm long and curving posteriorly and proximally. The layers encountered are the subcutaneous fat, fascia lata, bursa, and gluteus medius layers.
The fascia lata is initially incised in alignment with the femur, following the original incision line and curving posteriorly. Typically, a small central incision is made using a scalpel to initiate the process. The fascia lata is cut with scissors distally and then proximally. The fascia is then retracted using either self-retainers or a Charnley retractor, with the latter positioned so that the D shape created points toward the knee. The trochanteric bursa is excised using forceps and scissors. The greater trochanter and its attached muscles become visible after this step, with the gluteus medius proximally and vastus lateralis distally.
The assistant should then externally rotate the leg to put the gluteus medius on the stretch. The greater trochanter's tip should be identified, and the gluteus medius fibers split. The superior gluteal nerve is approximately 5 cm proximal to the tip of the greater trochanter.
The hip abductors, the superficial gluteus medius and the deep gluteus minimus, are then detached from the greater trochanter using diathermy. This procedure is typically performed by tracing an "s" or "omega" shape, leaving a sufficient cuff for repair at the end. Splitting some of the vastus lateralis fibers is occasionally necessary. Adequate dissection should reveal the capsule. A T-shaped incision is made in the capsule, staying close to the bone at the femoral neck's base. Dislocating the hip is necessary and can be achieved through external rotation, which exposes the fractured neck as the leg is positioned into the leg bag to improve visibility.
The next step is to make the neck cut, accomplished with an oscillating saw at a 45° angle. This cut is usually measured from a line extending between the neck's superior aspect to 1cm proximal to the lesser trochanter, although it may vary depending on the prosthesis being used, particularly if it includes a collar.
The femoral head may be removed using the corkscrew, which is placed centrally in the head and then twisted in. The head is spun to detach it from the acetabulum. A mallet may be necessary to help engage the corkscrew with the bone. The capsule cut's sufficiency must be checked if the femoral head is difficult to remove. The femoral head must be measured using the guide. If between sizes, most surgeons advise erring on the smaller side to minimize the risk of dislocation. Ensure all soft tissue is removed when preparing the acetabulum. A bone nibbler may be used to remove any remaining soft tissue.
For femoral canal preparation, a Hohmann retractor is used to expose the femoral calcar. The femur is prepared using a box chisel, which is typically placed posterolaterally to open the femoral canal. A T-handled reamer is then introduced into the canal. One hand must be placed on the patient's knee during this step to ensure alignment with the anatomical axis. Reamers of progressively larger sizes are used until rotational movement is impeded. The femoral canal is then smoothed using a rasp, with particular attention given to rasping the lateral side.
The head is trialed, and the hip is reduced to assess size and stability with internal and external rotation, with the hip flexed and extended. Leg length equality is assessed. However, this part is not always performed because of the joint's intrinsic stability. Difficulty reducing the hip may be due to the stem being too proud, offset being too great, or soft tissue obstruction being present. The trial is dislocated if further adjustments are necessary.
A cement restrictor is inserted, which may need to be sized depending on the kit used. The restrictor is typically 2 cm more than the stem's length. The femoral canal is then washed using copious pulse lavage. Ribbon gauze is inserted into the femoral canal alongside a clean suction catheter. This process ensures the canal is dry and free from fat and blood, allowing the cement to interdigitate with the bone for solid fixation. The cement is then prepared. The gauze is afterward removed, and the cement is inserted into the canal using the cement gun. The nozzle should be inserted fully into the canal, and the cement pressure should push the gun up proximally. Surgeon preference dictates whether the cement is pressurized.
The selected femoral stem is then inserted into the femoral canal. All excess cement must be removed. The femoral stem should ideally have 10 to 15° of anteversion. The degree of anteversion must not change once the stem is in situ at the appropriate depth to prevent a varus stem, which may compromise the outcome. The femoral head is then attached to the trunion, and the hip is reduced. Reduction is achieved with gentle traction and a small degree of internal rotation. Stability should be assessed afterward.
The wound is then washed and closed in layers—capsule, abductors en masse, fascia lata, fat, and skin. A double-layered combination using interrupted and continuous suturing of the abductors helps securely close the wound.[32]
Postoperative Plan
Routine labs must be obtained after the procedure, including a complete blood count and a basic metabolic panel. The results must be checked at various intervals following surgery, with the frequency depending on the patient's overall condition. Formal radiographs may also be ordered, depending on the surgeon's assessment. A posthemiarthroplasty x-ray ensures the joint is reduced and in an ideal position. Postoperative antibiotics and DVT prophylaxis may be initiated as per hospital protocol.
Mobilize full weight-bearing as pain allows with physiotherapists, incorporating partial or touch weight-bearing in cases involving cannulated screws and comminuted fractures managed with an intramedullary nail. Follow-up appointments are scheduled depending on the surgeon's assessment.
Complications
Patients undergoing an FNF procedure typically have comorbidities that put them at high risk of developing complications. These potential occurrences must be explained to patients to help them make informed decisions about their treatment plans. Possible surgical complications include the following:
- Infection: Sepsis can occur in up to 20% of cases and can result from superficial or deep infection. Healthcare professionals believe the presence of hematoma increases this risk. Antibiotics are usually given at induction, with 2 doses administered postoperatively.[33][34]
- Fixation failure: This complication is more likely to occur in patients with pathological bone conditions, for example, rheumatoid arthritis and osteoporosis. Fixation failure may also result from technical errors while operating. Loosening or dislocation can also occur following a hemiarthroplasty.[35]
- Fracture: Hemiarthroplasty procedures themselves have a 4.5% fracture risk. These fractures often occur during hip reduction and commonly affect the neck or greater trochanter.[36]
- DVT and VTE: These complications are significant concerns following FNF procedures due to factors such as immobilization, surgery-related trauma, and underlying comorbidities. Preventive measures, including pharmacological prophylaxis and mechanical interventions, are essential to mitigate the risk of DVT and its possible consequences in patients undergoing FNF procedures.
- Fat embolism: This condition is a potential complication of pressurizing cemented stems and nailing. Hypoxia may be noted during pressurization or after hip reduction. Adequate femoral canal lavage and drying can minimize the risk.
- Leg length discrepancy: This condition may arise in any FNF procedure. Slight differences can be managed with a shoe lift if problematic.
- Nonunion: Patients may present with groin or buttock pain approximately 12 months following fixation. Pain is worse on hip extension or with weight-bearing. Nonunion is thought to occur in up to 25% of displaced fractures and 5% of undisplaced fractures. Management is either with total hip replacement in the elderly or proximal femoral osteotomy in the young. The condition is more common after SHS and cannulated screw fixation than other techniques.
- Dislocation: This complication is often associated with hemiarthroplasty. Patients undergoing THA for an FNF generally exhibit an elevated postoperative dislocation rate compared to those undergoing elective, primary THA procedures for other conditions, eg, osteoarthritis and hip dysplasia.
- AVN: This condition can occur in up to 10% of undisplaced fractures and 30% to 45% of displaced fractures. Patients typically present with groin pain. Sclerosis signs may show on radiographs. Management typically involves conversion to a total hip replacement, but alternatives such as osteotomy or core decompression may be considered in younger patients.[37]
- Malunion: This complication has an incidence of 5% to 30%. Varus malreduction following cannulated screw fixation correlates with fixation failure.
- Death: Mortality is approximately 30% in the elderly in the first year following an FNF.
Many of these surgical complications can be mitigated or effectively managed with vigilant preoperative optimization, meticulous surgical technique, and proactive postoperative care. Collaboration among multidisciplinary healthcare teams, patient education, and adherence to evidence-based protocols are crucial in minimizing the occurrence of complications and optimizing patient outcomes.
Clinical Significance
The above procedures are commonly performed, though different fracture types and patient characteristics may warrant modifying a surgical approach. Contentious areas in surgical techniques are briefly considered below.
Bipolar versus Unipolar Hemiarthroplasty
Debate exists over the use of bipolar or unipolar implants. In bipolar implants, the femoral head is surrounded by a polyethylene liner within an acetabular shell where it can move. Unipolar implants are simpler and less expensive than bipolar types. Studies suggest that bipolar implants confer the benefits of reduced pain, less acetabular wear, and lower dislocation rates, though these types are more expensive than their unipolar counterparts. Bipolar implants are also easier to convert to a total hip replacement than unipolar types when necessary. However, evidence suggests that bipolar implants also lose movement at the inner bearing and eventually resemble a unipolar implant over time.[38]
Cemented versus Uncemented Hemiarthroplasty
Cemented implants give better functional and mobility-related outcomes than uncemented types. These implants also confer greater stability than uncemented ones. However, cemented implants carry an increased risk of fat embolism, which can cause hypoxemia. Still, research suggests that cemented stems carry a higher overall survival rate than their uncemented counterparts. The cement acts as a grout, creating an interface to distribute the load between the femoral stem's smooth surface and the bone surface's irregularities.[39]
Uncemented implants carry a higher postoperative and intraoperative periprosthetic fracture risk.[40] Stability is conferred from the uncemented stem's impaction in the cancellous bone, but poor bone quality impairs impaction and reduces stability. A study reported that cemented femoral component fixation for THA was associated with lower periprosthetic fracture and aseptic revision rates but higher VTE rates in patients with FNF aged 65 and older.[41]
SHS Lag Screw Positioning
The tip-to-apex distance (TAD) is the distance between the screw tip and the femoral head's apex on the APL view. Baumgaertner et al. found that a TAD less than 20 mm avoided screw cut-out.[42] A TAD less than 25 mm can minimize failure risk. The lag screw should be slightly inferior on anteroposterior view and slightly posterior on lateral view. Eccentric placement is likely to cause a rotational construct failure.[43] The anterosuperior region is where bone quality is the poorest.
Arthroplasty Timing
A retrospective FNF study lasting over 6 years in China reported that early THA had a lower risk of pulmonary embolism, DVT, blood transfusion, 30-day readmission, and VTE-related readmission. Similarly, early hemiarthroplasty had a lower DVT and blood transfusion risk than delayed hemiarthroplasty.[44]
Effect of Obesity
A retrospective study reported that obesity increased operative time without increasing postoperative complication risks in hemiarthroplasty and THA for isolated FNFs. However, anesthetic exposure is prolonged in patients with obesity. The postoperative effect of long anesthesia duration must be explored in future studies.[45]
Enhancing Healthcare Team Outcomes
The interprofessional approach is essential when caring for patients undergoing hip surgery for FNF. Notably, preoperative medical optimization of patients with FNF is vital for an excellent surgical outcome. Specialists within orthogeriatric and medical teams must collaborate to achieve preoperative optimum medical conditions.
Physiotherapists and occupational therapists are also vital to safely mobilize patients with FNFs and ensure a safe hospital discharge. Proper physical therapy can help most patients regain function and muscle strength. Failure to comply with physical therapy may lead to disuse and numerous other complications.
The primary care provider and nurse practitioner must continually follow individuals with FNFs to ensure they ambulate without pain and avoid postsurgical complications. All healthcare professionals involved must coordinate their activities, working as an interprofessional team, to achieve satisfactory rehabilitation and restore limb function in patients with FNFs.