Continuing Education Activity
Esophageal injury (EI) is a rare but challenging clinical finding in the setting of trauma. Esophageal injuries or perforations are transmural disruptions of the esophagus that subsequently lead to leakage of intraluminal contents into the surrounding mediastinum. This causes local inflammation, systemic inflammatory response, and eventually can lead to the development of sepsis, which is associated with high morbidity and mortality. Esophageal injuries are most commonly iatrogenic, such as injury incurred during endoscopic exam, naso-enteric tube placement, or surgical procedures; however traumatic injuries also may occur and may be due to blunt trauma such as a motor-vehicle accident or penetrating trauma such as a gunshot or stab wound. Other miscellaneous mechanisms include foreign body ingestion, spontaneous rupture, such as in Boerhaave syndrome, and ingestion of acid/caustic substances. This activity explains when esophageal trauma should be considered, articulates how to properly evaluate for this type of injury, and highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
Describe the anatomy of the esophagus.
Describe the components involved in evaluation of esophageal trauma.
Summarize the management approaches for esophageal injury.
Outline the importance of collaboration and coordination amongst the interprofessional team in optimizing the outcomes for patients with esophageal trauma.
Introduction
Esophageal injury (EI) is a rare but challenging clinical finding in the setting of trauma. Esophageal injuries/perforations are transmural disruptions of the esophagus that subsequently lead to leakage of intraluminal contents into the surrounding mediastinum. This causes local inflammation, systemic inflammatory response, and eventually the development of sepsis that results in significant morbidity and mortality. Esophageal injuries can be iatrogenic or traumatic. Examples of iatrogenic mechanisms include endoscopic examinations, nasoenteric tube placement, and surgical procedures. Traumatic mechanisms may be either blunt (e.g., motor-vehicle crash) or penetrating (e.g., gunshot or stab wounds). Other miscellaneous mechanisms include foreign body ingestion, spontaneous rupture (e.g., Boerhaave syndrome), and ingestion of acid/caustic substances. Overall, the most common mechanism of EI is iatrogenic (upper endoscopy), and patients who are at highest risk for iatrogenic perforations also tend to have multiple comorbid conditions.[1][2][3][4][5]
Etiology
The esophagus is a muscular conduit, approximately 25 cm long, extending from the lower end of cricoid to the stomach. In the neck, the esophagus originates at the level of the sixth cervical vertebral body. The esophagus then descends anterior to the vertebral column through the superior and posterior mediastinum. It terminates at the cardia, corresponding to the level of 11th-12th thoracic vertebrae. The esophagus has four layers: the mucosa, submucosa, muscularis propria, and adventitia. The muscularis propria is critical to esophageal structure and function. It is composed of two layers of muscle fibers: The inner (or circular) layer and the outer (or longitudinal) layer.
The esophagus is divided into three main anatomical regions: cervical, thoracic, and intra-abdominal esophagus. The corresponding arterial supplies of the esophagus are as follows: inferior thyroid artery, a branch of the thyrocervical trunk, supplies the cervical esophagus; branches of the thoracic aorta and bronchial arteries supply the thoracic portion, and the left gastric/inferior phrenic arteries supply the the abdominal esophagus. In terms of venous drainage, the inferior thyroid vein drains the cervical esophagus; the azygos, hemiazygos and bronchial veins drain the thoracic esophagus; and the coronary veins drain the abdominal esophagus.
The upper one-third of the esophagus is under voluntary control whereas the mid- and distal thirds are under involuntary control. Because of other nearby anatomic structures, these three distinct esophageal regions tend to have different injury patterns, mechanisms, and presentations. Diagnostic and therapeutic approaches vary based on the anatomic region involved. Esophageal injuries are graded based on the American Association for the Surgery of Trauma (AAST) classification, as follows:
- Grade I - Contusion/hematoma, partial thickness tear
- Grade II - Laceration less than 50%
- Grade III - Laceration greater than 50%
- Grade IV - Less than 2cm disruption of tissue or vasculature
- Grade V - Greater than 2cm disruption of tissue or vasculature
Injuries can occur along the entire course of the esophagus. The preferred approach to abdominal perforations is a surgical repair. For many thoracic and cervical perforations, non-operative primary management is acceptable, with surgery being the second-line therapeutic option. The approach was chosen often depends on the patient's clinical presentation and the presence (or absence) of associated injuries to nearby anatomic structures. The cervical esophagus is surrounded by the trachea anteriorly, the spine posteriorly, and the carotid sheath on both sides. Morbidity and mortality of penetrating trauma to the cervical esophagus are closely related to associated injuries to nearby vital structures. In the normal esophagus, the greatest at-risk location for iatrogenic instrumentation injury is the cervical esophagus around the region bounded by the inferior pharyngeal constrictor and the cricopharyngeus muscle. Cervical esophageal injuries are the most common overall and carry the lowest mortality due to significant advances in both operative and non-operative management. Thoracic esophageal injuries occur less commonly but are associated with the highest morbidity and mortality, primarily because of the proximity of the thoracic esophagus to other vital structures and the risk of severe mediastinal sepsis. The abdominal esophagus is the least commonly injured, with intermediate morbidity and mortality. The lack of the serosal layer, combined with a relatively poor blood supply, combine to increase the overall risk of subsequent complications following injury.[6][7][8][9][10]
Epidemiology
Overall traumatic esophageal injuries (EI) are rare. Even among large trauma centers, the typical incidence of EI may be as low as one to two cases per month. Penetrating EI is more common than blunt EI, with a corresponding ratio of approximately 10-to-1. Among penetrating injuries, the most common etiologies in the United States are gunshot wounds (about 75%) and stab wounds (about 15%). Many penetrating EI's are associated with damage to nearby structures, including neighboring mediastinal organs (e.g., trachea, heart, lungs). Although uncommon, combined esophageal and tracheal perforations can be life-threatening. Mortality is extremely high if great vessels are also injured. Penetrating trauma to the esophageal hiatus may be associated with potential concomitant injuries to other critical structures such as the aorta, heart, liver spleen, colon, pancreas, and stomach.
The morbidity and mortality of esophageal injuries are usually determined by a combination of temporal, patient, and injury severity factors. The best prognosis is associated with early injury identification and treatment, minimal or no injuries to surrounding structures and minimal or no contamination, and an otherwise healthy patient with minimal or no co-morbid conditions. The converse is true with each of the factors being at the opposite of its corresponding spectrum. Traumatic esophageal injuries often present a diagnostic challenge, especially because of the potential for damage to surrounding tissues and concurrent contamination. Consequently, the trauma surgeon must be aware of the various mechanisms of EI, employ a high index of clinical suspicion, and act in a timely manner when an injury is suspected.
Pathophysiology
In absolute terms, the most common EIs are iatrogenic. Commonly associated medical conditions include esophageal strictures and achalasia. Iatrogenic EIs can also result from intraoperative injury to the esophagus (e.g., during thoracotomy or neck exploration). In approximately 15% of non-traumatic EIs, the cause is a spontaneous rupture, not otherwise associated with any pre-existing condition. Some causes include forceful vomiting, retching, or increasing in intra-abdominal pressure as seen in Boerhaave syndrome.
Non-iatrogenic, traumatic EI patterns vary depending on mechanistic considerations. In this broad grouping of EIs, penetrating mechanisms predominate. Both stab and gunshot wounds can be problematic because the associated tissue damage may not be immediately apparent, resulting in diagnostic (and therapeutic) delays. Injury patterns and modalities can vary across different geographic areas. For example, gunshot wounds are more common in the United States while stab wounds tend to be more prevalent in other countries. Penetrating cervical EI is present in less than 1% of all penetrating traumas but has been identified in 5% to 12% of all penetrating neck injuries. Penetrating thoracic EIs have been reported to occur in less than 1% of all penetrating thoracic wounds.
Depending on projectile velocity and other characteristics, gunshot wounds can cause significant amounts of shearing, stretch, and blast injury to surrounding tissues. The associated tissue ischemia and full-thickness necrosis may evolve over time, contributing to either a missed diagnosis or delayed presentation, both of which can substantially increase morbidity and mortality. Stab wounds generally cause less injury to surrounding tissues but can difficult to visualize if minimal/focal in character. The increasing availability of advanced imaging for trajectory determination, especially for gunshot wounds, is important in the assessment, diagnosis, and operative planning for EI. This may not be true for stab wounds, mainly to the lesser extent of tissue injury.
Blunt EIs tend to affect the abdominal/distal esophagus and are commonly associated with motor-vehicle crashes. The pathophysiologic mechanism is due to the sudden application of a blunt force to the abdomen, usually with a full stomach. This then leads to the sudden stretching of the gastroesophageal junction, tissue stretching against the hiatal crura, and the presence of shear forces that results in the tearing of the esophageal wall. The lack of an esophageal serosal layer further exacerbates the injury potential and the risk of perforation. Finally, EIs can result secondarily as a result of other nearby anatomic structures either eroding into or puncturing the esophagus. For example, vertebral injuries associated with bony fragmentation can injure the esophagus, especially in the mid-cervical and upper thoracic locations, and in the presence of osteophytes. Mediastinal abscesses and hematomas may also cause external compression of the esophagus and resultant symptoms and/or secondary injury.
Because the esophagus can be considered to be in an anatomically “protected” mediastinal location, it is inherently surrounded by a highly crowded number of other, often critical anatomic structures. Consequently, many traumatic EI's are associated with other, potentially serious injuries to surrounding tissues. This is why some traumatologists consider the presence of EI to be a “marker” for other associated injuries. In fact, nearly 9 out of 10 patients with penetrating esophageal trauma had major associated findings, including tracheal, vascular, pulmonary, diaphragmatic and spinal injuries.[11][12][13]
History and Physical
A detailed and thorough history and physical examination, with the concurrent identification of pertinent clinical risk factors, is required for all patients with a suspected esophageal injury. Appropriate imaging is an essential part of EI management. Pain associated with EI tends to be very acute, with chest pain being the principal symptom in 70% of patients with intrathoracic esophageal perforation. The pain may radiate to the back or left shoulder, depending on injury location and any associated tissue damage. Vomiting and dyspnea may be present in about 25% of patients, although this may increase with diagnostic and/or therapeutic delays. Although appreciated in only about 1 out of 7 cases, Mackler’s Triad (e.g., subcutaneous emphysema, chest pain, and vomiting) is considered to be pathognomonic for esophageal perforation. The Hamman sign, a systolic "crunching" or "rasping" sound, synchronous with the heartbeat, and heard over the precordium, is found in up to half of EI cases.
A thorough history and physical examination enhance the clinician's understanding of the location and severity of EI. This then helps prevent clinical delays, in addition to better guiding the use of diagnostic imaging. Cervical esophageal injury, for instance, may be associated with dysphonia, hoarseness, cervical dysphagia, and subcutaneous emphysema. Associated imaging workup may then be tailored specifically to these clinical findings. In contrast, perforation at the gastroesophageal junction will most likely present with acute abdominal pain, thus prompting an imaging investigation focused on the identification of peritoneal contamination source. Finally, the thoracic esophageal perforation may manifest either with mediastinal or pleural findings/complaints. Trauma victims suspected to have EI should prompt special attention if they develop a temperature greater than 38.5 C, tachycardia, or auscultation of crepitus on physical examination. This is especially important given that clinical decline toward septic shock can be rapid following the initial period with relatively few signs and/or symptoms.
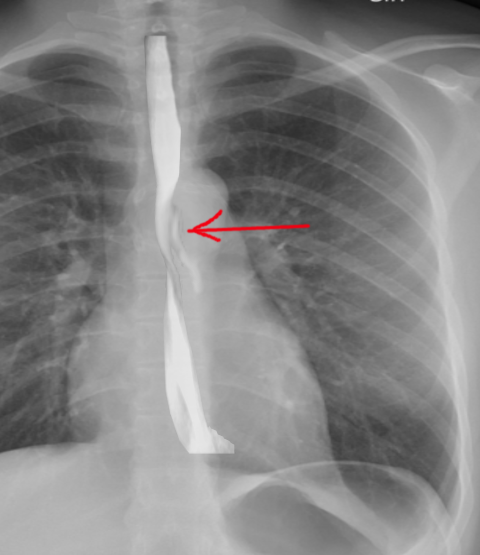
Although specific diagnostic and radiographic findings are beyond the scope of this discussion, a simple chest x-ray study will demonstrate evidence of perforation in as many as 90% of cases. Despite that, the finding of subcutaneous emphysema requires approximately one hour to develop, and the findings of mediastinal widening and pleural effusion(s) may take up to several hours. Consequently, it is important to reevaluate patients whose initial workup was negative because additional evidence of EI may be detected within the initial 12 hours post-injury.
Evaluation
Contrast-enhanced esophageal imaging provides excellent demarcation of the anatomy and is effective in detecting perforations. There are different types of contrast media that can be utilized, including water-soluble iodinated high osmolality agents and water-soluble non-ionic agents for preliminary detection of perforation. These are generally followed by barium sulfate in cases where initial esophagram is negative, but suspicion for the presence of injury remains high. It should be noted that because of the possibility of significant esophageal inflammation and edema in the setting of injury, the false-negative rate of esophagograms approximates 10%.
Computed tomography (CT) is useful to evaluate nontransmural esophageal perforations not detected on esophagram. CT may help establish the full extent of an injury and guide any subsequent therapeutic interventions. Some clinical scenarios where CT has high utility include negative early esophagram with continued high clinical suspicion; in patients who are uncooperative, neurologically impaired, and/or critically ill; and cases involving simultaneous vascular and airway injuries. Findings on CT imaging may include gas and fluid gathering around the esophagus; esophageal wall thickening; and radiographic evidence of inflamed mucosa. Finally, air or air-fluid collection in the mediastinum, pleural effusion(s), pneumocardium and pneumoperitoneum may also be seen. A chest and upper abdominal CT study with oral contrast are most likely to demonstrate a leak from thoracic or abdominal esophageal perforations.
Flexible esophagoscopy has clinical utility in penetrating trauma because it provides direct visualization of the EI and has a sensitivity of nearly 100% with a specificity of about 85%. On the other hand, the role of esophagoscopy in nonpenetrating EIs is inconclusive at best. Because it requires air insufflation, flexible esophagoscopy, is contraindicated with small mucosal or submucosal tears because it may exacerbate the perceived severity of the injury/perforation and thus lead to inappropriate subsequent management. Although generally not indicated as the initial diagnostic tool, endoscopy may be justified for use in the setting of continued suspicion of injury despite negative CT scans and esophagograms, as well as in the setting of the history of GERD or peptic ulcer disease.
Early diagnosis of esophageal perforation is associated with improved morbidity and mortality. Because EIs are rare, and their initial symptoms tend to be vague, a high degree of suspicion, in conjunction with a thorough physical examination and consideration of injury mechanism in the context of pertinent anatomy, may help optimize the management of EIs.[14][15]
Treatment / Management
Given their relative rarity, clinical management of EIs has primarily been extrapolated from accumulated clinical cases and series, many of which also discuss non-trauma etiologies of esophageal injury/perforation. Consequently, the following management strategies commonly applied to esophageal perforation are being generalized to include both penetrating and blunt traumatic EI. As previously stated, the location of injury will play an important role in the treatment of the EIs, with the focus of this review on thoracic EIs.
In general, earlier and more prompt diagnosis and management of EIs results in better patient outcomes. The high risk of mediastinitis leading to severe systemic sepsis/septic shock, impaired future healing, and disruption of the surgical plan(s) underscores the importance of early and proper management. The lack of a serosal layer makes any esophageal repairs far more tenuous than repairs of other portions of the gastrointestinal tract. Definitive closure and drainage are best carried out as soon as possible, although exceptions to these rules do exist. On rare occasions, other life-threatening injuries and/or competing pressing medical conditions may take precedence over the immediate management if EI. In such cases, prioritization of which injury/condition should be approached first must consider the overall risk-benefit equation specific to a particular clinical scenario.
Non-Operative Management
Non-operative management of EI may be indicated in patients who have contained leaks, are hemodynamically stable with few signs/symptoms, or those who are moribund and unlikely to survive a major operation. Many patients within this group may have had a significant delay in diagnosis due to a mild clinical presentation. Others may have been found to have a major injury after surviving the initial sepsis and mediastinitis. Assuming that diagnosis has not been missed and that the patient genuinely has a "contained" esophageal injury, the following criteria may warrant non-operative management (all three criteria required): (1) contained leak (2) mild symptoms, and (3) minimal evidence of clinical sepsis. A contained leak is best described as extravasation of contrast on esophagram, but the contrast “loops back in” after initially extravasating from the esophagus. This is usually a small area not associated with a standing fluid collection, mediastinal inflammation, or pleural effusion. An esophagram can be repeated within several days to document the resolution of the leak before starting an enteral diet. Patients who are not ideal candidates for operative intervention because of severe sepsis or pulmonary compromise should undergo wide chest drainage at the bedside, usually using a greater than one tube thoracostomy.
Operative Management
Although there are no prospective studies defining a "safe window" of time within which diagnostic testing can be completed before operative intervention, there is general agreement that EI is a surgical emergency, and pre-operative testing must be expedited to facilitate a timely repair. The severity of concomitant injuries often necessitates a delay of esophageal repair. Literature supports the notion that the degree of inflammation in surrounding tissues (as opposed to the time initial injury) should guide the choice of primary repair versus drainage. It is also known that the degree of soilage correlates with the overall morbidity associated with EI. Surgical repairs can usually be accomplished, even at delayed time periods, in patients with minimal soilage at time of the operation. Because post-repair morbidity and mortality are mainly related (and attributed) to anastomotic failures, every single factor should be considered carefully at the time of initial management strategy formulation.
The location of the injury is another factor that influences both the surgical approach and various surgical repair options. Injuries of the cervical esophagus are best approached from the left neck where the recurrent nerve can be more easily identified and preserved. The incision should be placed at the anterior border of the sternocleidomastoid muscle and carried down through the soft tissues between the trachea and the carotid sheath. The esophagus can be mobilized using the blunt technique, with careful attention not to injure either the recurrent nerve or the membranous portion of the trachea. Buttressing flaps are discussed in later paragraphs (see below).
Thoracic esophageal injuries are best approached through a right posterolateral thoracotomy. Appropriate patient positioning is critical to proper surgical visualization and surgical repair optimization. The intercostal muscle bundle is of great importance and must be preserved when entering the thoracic cavity. It can be extremely valuable as a potential repair-buttressing flap, providing vascular tissue coverage over the esophageal repair.
The distal third of the thoracic esophagus is best accessible via a left postero-lateral thoracotomy or from the abdomen (after appropriately mobilized). Finally, the abdominal portion of the esophagus is best accessed by an upper midline laparotomy. This should be carried up to the xiphoid process and down to the level of the umbilicus.
Primary Repair
Primary repair of an IEs requires attention to several important surgical principles. First, anatomic areas directly involved in the injury must be fully debrided to healthy tissue. Use of necrotic or devascularized tissue will endanger the integrity of the repair. EIs tend to be most extensive at the level of the mucosa. Consequently, simply identifying and repairing the muscular portion of the injury will likely result in an incomplete closure of the mucosal defect. The muscular defect should be carefully extended until the ends of the mucosal injury are identified.
Second, EI repair must be tension free, and mobilization of the esophagus should be minimized because its blood supply is segmental. Overzealous mobilization can render the anastomosis ischemic and result in a postoperative leak. To help strengthen the integrity of the repair, the esophagus should be reapproximated in two-layers, with an inner, running, absorbable suture and an outer, interrupted, non-absorbable suture. Stapled mucosal anastomosis also can be performed, followed by suture approximation of the outer esophageal layer.
Third, repairs should be buttressed with local tissue and muscle flaps, especially if repair is delayed (e.g., greater than 8-12 hours from injury) or if there is another nearby injury or adjacent suture line. For example, injury to both the esophagus and trachea with parallel suture lines should be separated by a tissue flap to tracheoesophageal prevent fistula formation. Muscle flaps also improve the vascular supply in the setting of active contamination. The choice of tissue flap is dictated by the relative location of the injury and the flap's anatomic origin (e.g., vascular supply). Commonly used flap materials include latissimus dorsi, serratus anterior, or intercostal muscles. Pericardium or pleura are secondary choices because they are more fragile and comparatively less vascular. In the chest, the intercostal muscle provides the simplest and most reliable tissue flap. Care must be taken when making the thoracotomy incision to preserve this important muscular complex. Other flap options in the chest include the latissimus dorsi, the rhomboid, and the diaphragm. In the abdomen, a Thal patch (e.g., gastric fundus) or various types of fundoplications can be performed. For cervical EIs, the sternocleidomastoid muscle can be used as a barrier between adjacent structures or to reinforce the repair. Due to its abundant blood supply and location, the sternocleidomastoid is very reliable as a tissue flap. Wrapping the esophagus with the platysma muscle has also been described.
Fourth, appropriate drainage should accompany all esophageal repairs. This reduces the severity of systemic reaction and sepsis in the event of an anastomotic breakdown. It also serves as a diagnostic "early warning system," especially when one considers that an undrained mediastinal collection can lead to severe sepsis and significantly elevates patient mortality. When used appropriately and performed in a timely fashion, primary repair of EIs is the preferred option, with low morbidity and mortality.
Wide Chest Drainage
Wide chest drainage alone can be utilized as an option to control contamination in patients who are not candidates for primary repair or surgical diversion. This may be due to other competing clinical priorities, co-morbid conditions, or cases where tissue inflammation and soilage preclude injury repair. Usually, wide drainage can be performed in the setting of close observation, in the intensive care unit. In many such cases, patients may be unstable to withstand a major operation. At the same time, operative placement of drains tends to be more effective. Beyond initial management, if wide drainage becomes the "primary" management, it may be combined with esophageal diversion and/or exclusion (see below). Because of the inherent patient selection bias, wide drainage alone is associated with exceedingly high mortality.
Esophageal Diversion & Exclusion
Esophageal diversion and exclusion facilitate a decreased local flow of oral secretions and reflux of gastric contents at the site of EI. A diverting cervical esophagostomy should be performed in cases where primary repair is not a viable option and wide drainage is therefore chosen as the treatment approach. Esophageal exclusion (diversion with the closure of the gastro-esophageal junction) can be considered for extensive EIs (or those diagnosed with a delay), especially in the setting of significant tissue contamination and swelling. The involved anatomic locations are most often in the mid-to-distal esophagus.
Patients with a delayed diagnosis of EI can present with marked inflammation of the upper mediastinum that can preclude esophageal mobilization and creation of a proximal loop esophagostomy. In such cases, an end cervical esophagostomy can be created, clearly not a preferred approach that is acceptable only as a temporizing measure for several days while the mediastinal sepsis resolves. If the diverted esophagus is also temporarily excluded, either with absorbable sutures or a stapling device, recanalization of the diverted portion takes place, usually in as little as two weeks. This may present clinically as renewed mediastinal contamination in an otherwise recovering patient. Once the esophageal injury seals off from the pleural spaces and mediastinum, careful attention must be given for the development of the so-called “blind loop" syndrome. Bacterial stasis and overgrowth within the excluded esophagus can result in sepsis. In such cases, CT imaging may show a grossly dilated and enhancing esophagus. After confirming the diagnosis, the "blind loop" syndrome is treated with appropriate drainage procedure(s), usually determined on case-by-case basis.
T-Tube Diversion
T-Tube diversion of the esophagus can be used for smaller, usually distal injuries in patients who are not candidates for primary repair and where formal diversion and exclusion may not be required. From a surgical standpoint, the T-tube is placed directly through the injury into the site of EI and kept on constant suction to encourage the formation of a controlled fistula. The tube is kept in place for several weeks to allow a tract to form. This approach is especially useful for small injuries near the gastro-esophageal junction. Placement of large bore mediastinal and pleural tubes should accompany the T-tube. Once stable, the patient will need a gastrostomy tube for decompression and a jejunostomy tube for feeding.
Esophagectomy
Esophagectomy is rarely required as therapy for EIs but may be needed if the primary repair fails or cannot be performed after "damage control" maneuvers involving diversion and/or exclusion. Limited, retrospective clinical data suggest that esophagectomy may be the preferred approach for patients diagnosed with delayed EIs. These experiences suggest an acceptable safety profile of this approach, especially in the absence of any further interventions. Associated mortality also may be lower than that for non-operative approaches. If esophagectomy is selected as the optimal approach for a carefully selected patient, it is best performed using the Ivor-Lewis technique because the mediastinum is usually too inflamed to facilitate safe of transhiatal approach. Because of the technical complexity of this operation, especially in the setting of EI, it should optimally be carried out by experienced thoracic or esophageal surgeon(s).
The simplest and most commonly performed repair, characterized by a single anastomosis, is the gastric "pull-up." Because the stomach is usually the conduit of choice, gastrostomy tubes should not be placed in patients with EIs who require resective managment. When the gastric "pull-up" option is not available, post-esophagectomy restoration of luminal continuity can be performed using a colonic interposition (usually transverse colon) or a Roux-en-Y jejunal limb. The decision regarding which conduit to use depends on any concomitant injuries and the availability of a non-injured, well-perfused conduit. Preferred enteral feeding access is via a surgical jejunostomy tube.
Post-Operative Care
Post-operative care involves appropriate monitoring, initially in an ICU setting. Early recognition and treatment of cardiovascular complications and/or sepsis is paramount. Adequate nutritional support also plays an important role in optimizing clinical outcomes. Total parenteral nutrition or jejunostomy feeding should be started as soon as possible. Contrast swallow evaluations should take place 5 to 7 days after primary esophageal repair if no clinical signs of leakage are present. All drains should be maintained until contrast radiography confirms healing.
Complications of Operative Care
An anastomotic breakdown is unfortunately relatively frequent after EI repairs, primarily due to the multitude of risk factors outlined in previous sections. Depending on the location of EI, these leaks can lead to secondary wound infection, mediastinitis, abscess, empyema, pneumonia, and sepsis. Of all these complications, sepsis carries the highest associated mortality. Thus, the primary goal of postoperative management should be the prevention of sepsis by maintenance or establishment of wide drainage. Early recognition of sepsis is critical in instances where wide drainage fails to control soilage.
Fistula formation between the repaired esophagus and adjacent structures can occur in the immediate post-operative period or in a delayed fashion. The incidence of such fistulae increases when an adjacent structure also requires a concomitant surgical repair. Cutaneous and vascular fistulas have been described, but the most common fistula is a tracheal-esophageal fistula. These fistulae usually form at or just above the carina, and present with coughing after food or liquid ingestion and eventually the development of pneumonia. As previously discussed, the placement of an interposition vascularized tissue flap may help reduce the incidence of this morbidity. Commonly seen longer-term complications include stricture formation and the development of diverticulum around the repair site. Although most anastomotic strictures can be treated with endoscopic dilations, refractory cases may require esophagectomy. Diverticulum formation has also been noted post repair. Treatment of such diverticula depends on their size, location, and global clinical circumstance/context.
Cervical Esophageal Injury
In most cases, cervical EIs can be managed non-operatively or by simple retroesophageal drainage, usually combined with nil per os (NPO), antibiotics, and early nutritional support. Provided that any foreign bodies associated with the injury have been removed, such a non-operative approach is generally sufficient to achieve healing of the EI in question. In the continued presence of foreign bodies, surgical removal of the offending object and primary repair seems to be the best option. Surgery also may be required when the non-operative approach fails to result in expected clinical improvement. If other injuries (e.g., vascular or airway trauma) mandate surgical exploration, a primary repair can be effective in both controlling any ongoing contamination and reducing any associated vascular or airway-related complications. Negative pressure wound therapy has also been reported for complicated cases that failed to respond to the aforementioned options.
Esophageal Stenting
In patients with significant comorbid conditions, intra-luminal stenting has been described as a means to prevent intraluminal material from contacting the esophageal wall during the tissue healing process. Although this technology is still maturing, it will likely play a greater role in the future. As mentioned briefly in previous sections of this review, esophageal stenting has been used selectively in cases of EI, both primarily and for postoperative anastomotic leaks. Stents have been utilized in the care of thoracic EIs with good results, challenging the existing standard of care. In a recent retrospective study, treatment of esophageal perforation with stents rather than primary repair was associated with lower costs, fewer ICU days, shorter hospitalizations, quicker resumption of oral intake, and equivalent overall mortality. The timing of stent placement (e.g., less than 24 hours versus greater than 24 hours post-injury) does not seem to affect outcomes.
Among some of the reported advantage of esophageal stenting are (a) the ability to administer oral hydration and nutrition; (b) the possibility of device removal (e.g., reversibility); and (c) rapid elimination of mediastinal, pleural, and peritoneal contamination. In whatever setting esophageal stenting is used, it is important to remember that contamination must still be controlled and adequately drained. In some cases, a hybrid approach utilizing stenting and thoracoscopic decortication may be indicated. Finally, esophageal stenting is best utilized in the setting of isolated EI, and the presence of concomitant injuries may preclude its use. Consequently, stenting has been employed for iatrogenic and other non-trauma indications far more frequently than EI resulting from trauma.
Despite its clinical attractiveness and ease of placement, stenting of thoracic EIs has some potential downsides, including patient tolerance issues and the risk of stent migration. For the latter reason, stenting is not being performed for cervical or gastroesophageal junction EIs. Stent migration is a concern and may lead to further interventions. Migration of the stent is more likely with nonmetal stents are used.
Differential Diagnosis
Esophageal perforation can often be an obvious diagnosis if the patient presents after a traumatic event or if symptoms coincide with an esophagogastroduodenoscopy (EGD).
However, if a perforation is missed then the patient can present with chest pain, fever, or signs of systemic infection which can have a broad differential including, but not limited to:
- Myocardial infarction
- Mediastinitis
- Viral myocarditis
- Esophagitis
- Pulmonary embolism
- Aortic dissection
- GERD
- Gastritis
Prognosis
Esophageal injuries can result from both penetrating and blunt trauma. The need to screen for injury is based on a high degree of suspicion. Many patients may be asymptomatic initially. Imaging using CT scan is helpful to determine the potential for injury, especially in penetrating injury. Further workup should be timely, as an early diagnosis can help prevent further soilage and subsequent morbidity and mortality. Flexible endoscopy and contrast esophagography are complementary and together give the highest diagnostic yield. Primary repair with suture line reinforcement using muscle flaps and wide drainage affords the patient the best outcome. Stent placement in certain conditions can aid as a bridge either to surgery or definitive management. Early enteral nutrition via jejunostomy is preferred. Overall, the morbidity and mortality of esophageal trauma are high, and a high index of suspicion and aggressive treatment plan are required to optimize outcome.
Complications
The most feared complication of esophageal perforation is mediastinitis and sepsis which account for most of the morbidity and mortality related to this condition. Patients with undiagnosed esophageal perforations may also suffer from pleural effusions, abscess formation, bleeding, pneumothorax, or other complications involving leakage of air and esophageal contents into the thorax.
Postoperative and Rehabilitation Care
Postoperative and rehabilitative care may vary widely with patients that have a small, contained perforation able to be discharged within the same day as admission whereas patients with large revitalized segments of the esophagus may require extended ICU time as well as nutritional support via a feeding tube or parenteral nutrition.
Consultations
Esophageal perforations can be a surgical emergency and a general or thoracic surgeon should be consulted immediately upon diagnosis of this pathology. Depending on the patient's condition at presentation it may also be reasonable to inform an intensivist ahead of time of the likely need for an ICU bed.
Deterrence and Patient Education
Given that the majority of esophageal perforations are iatrogenic or traumatic in nature deterrence is difficult. Patients undergoing esophagogastroduodenoscopy (EGD) for any reason should be informed of the potential risk for esophageal perforation and the treatment options that would then become necessary.
Enhancing Healthcare Team Outcomes
Care of patients with EIs is an interprofessional, usually consisting of multi-specialty teams, including traumatologists/acute care surgeons, thoracic surgeons, otolaryngologists (for upper aerodigestive injuries), gastroenterologists, and intensivists. Mortality rates associated with EI range between 10% to 40% and depend on a variety of factors, including the cause of the perforation, the presence of any underlying (pre-existing) pathology, the location of the perforation, any diagnostic or treatment delay, the method of treatment employed, and the extent of the injury. Comorbid conditions, as well as the patient's functional and nutritional status, also play an important prognostic role. For a patient who survives their EI, high levels of morbidity, long hospital and ICU stays have been reported. Subsequent (post-discharge) quality of life can be negatively affected by EI. Because esophageal injuries occur infrequently and may produce vague symptoms, diagnostic and therapeutic delays are not uncommon. [16]