Continuing Education Activity
Pulmonary emphysema, a progressive lung disease, is a form of chronic obstructive pulmonary disease (COPD). Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines it as "a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway or alveolar abnormalities usually caused by significant exposure to noxious particles or gases." This activity reviews the cause, pathophysiology, and presentation of emphysema and highlights the role of the interprofessional team in its management.
Objectives:
Identify the causes of emphysema.
Assess the pathophysiology of emphysema.
Evaluate the treatment of emphysema.
Communicate the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by emphysema.
Introduction
Pulmonary emphysema, a progressive lung disease, is a form of chronic obstructive pulmonary disease (COPD). The Global Initiative for Chronic Obstructive Lung Disease (GOLD) has defined COPD as "a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway or alveolar abnormalities usually caused by significant exposure to noxious particles or gases."[1][2][3] COPD is the third leading cause of death in the United States and the fourth leading cause of death worldwide. COPD includes patients with chronic bronchitis and emphysema. Although identified as separate entities, most patients with COPD have features of both. COPD often coexists with comorbidities, which affect the disease course. Emphysema is a pathological diagnosis affecting the air spaces distal to the terminal bronchiole. It is characterized by abnormal permanent enlargement of lung air spaces with the destruction of their walls without any fibrosis and destruction of lung parenchyma with loss of elasticity.
Etiology
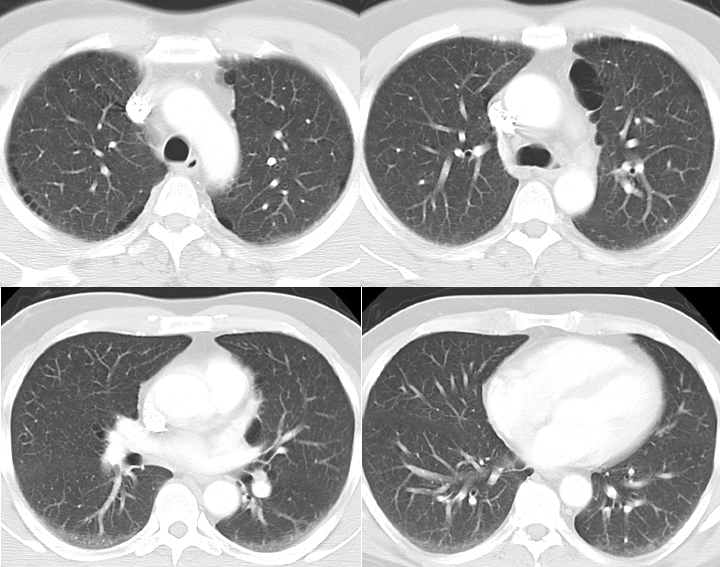
Emphysema is caused by chronic and significant exposure to noxious gases, of which cigarette smoking remains the most common cause, and 80% to 90% of patients with COPD are cigarette smokers identified, with 10% to 15% of smokers developing COPD (see Image. Emphysema). However, in smokers, the symptoms also depend on the intensity of smoking, years of exposure, and baseline lung function. Symptoms usually begin after at least 20 packs per year of tobacco exposure.[4][5] Biomass fuels and other environmental pollutants such as sulfur dioxide and particulate matter are recognized as important causes in developing countries affecting women and children greatly. A rare hereditary autosomal recessive disease, alpha 1 antitrypsin deficiency, can also lead to emphysema and liver abnormalities. However, it only contributes to 1% to 2% of cases of COPD. It is a proven risk factor and can present with pan-acinar bibasilar emphysema early in life. Other etiological factors are passive smoking, lung infections, and allergies. Moreover, low birth weight as a newborn makes one more prone to develop COPD later in life.
Epidemiology
Emphysema, as a part of COPD, is an illness that affects a large number of people worldwide. In 2016, the Global Burden of Disease Study reported a prevalence of 251 million cases of COPD globally. Around 90% of COPD deaths occur in low and middle-income countries.[6][7] COPD is the third leading cause of death worldwide, causing 3.23 million deaths in 2019. The prevalence of emphysema in the United States is approximately 14 million, which includes 14% white male smokers and 3% white male nonsmokers. The prevalence is slightly less for white female smokers and African Americans. These patient groups tend to develop emphysema after less exposure time than other patient populations. It is slowly increasing in incidence primarily due to the increase in cigarette smoking and environmental pollution. Another contributing factor is decreasing mortality from other causes, such as cardiovascular and infectious diseases. Genetic factors also play a significant role in determining the possibility of patient airflow limitation. Emphysema severity is significantly higher in coal worker pneumoconiosis, and this is independent of smoking status.
Pathophysiology
The clinical manifestations of emphysema are the consequences of damage to airways distal to terminal bronchiole, which include respiratory bronchiole, alveolar sacs, alveolar ducts, and alveoli, collectively known as the acinus. There is abnormal permanent dilatation of the airspaces and destruction of their walls due to the action of the proteinases. This results in a decrease in the alveolar and capillary surface area, which decreases the gas exchange. The part of the acinus affected determines the subtype.
It can be subdivided pathologically into the following:
- Centrilobular (proximal acinar) is the most common type and is commonly associated with smoking. It can also be seen in coal workers' pneumoconiosis.
- Panacinar is most commonly seen with alpha 1 antitrypsin deficiency.
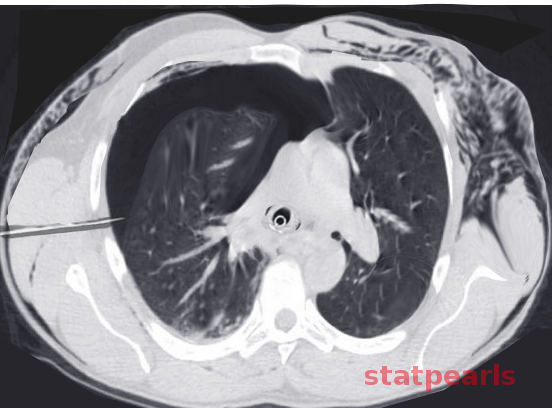
- Paraseptal (distal acinar) may occur alone or in association with the above 2. When it occurs alone, the usual association is a spontaneous pneumothorax in a young adult (see Image. CT Scan COPD, Paraseptal Emphysema).
After long-term exposure to noxious smoke, inflammatory cells such as macrophages, neutrophils, and T lymphocytes are recruited, which play an important role in the development of emphysema. First, macrophages are activated, which release neutrophil chemotactic factors like leukotriene B4 and interleukin-8. Once the neutrophils are recruited, these, along with macrophages, release multiple proteinases and lead to mucus hypersecretion. Elastin is an important component of the extracellular matrix required to maintain the integrity of the lung parenchyma and small airways. Elastase/anti-elastase imbalance increases the susceptibility to lung destruction, leading to airspace enlargement. Cathepsins and neutrophil-derived proteases (ie, elastase and proteinase) act against elastin and destroy the connective tissue of the parenchyma of the lung. Cytotoxic T cells release TNF-a and perforins, which destroy the epithelial cells of the alveolar wall. Cigarette smoking not only causes mucus hypersecretion and release of neutrophilic proteolytic enzymes, but it also inhibits anti-proteolytic enzymes and alveolar macrophages. Genetic polymorphisms have a role in inadequate antiprotease production in smokers. All of these contribute to the development of emphysema. Lung parenchyma produces alpha 1 antitrypsin (AAT), which inhibits trypsinize and neutrophil elastase in the lung. AAT deficiency (AATD) can lead to panacinar emphysema.
History and Physical
Most patients present with nonspecific symptoms of chronic shortness of breath and cough with or without sputum production. As the disease progresses, the shortness of breath and cough progressively worsen. Initially, there is exertional dyspnea with significant physical activity, especially arm work at or above shoulder level, with progression to dyspnea with simple daily activities and even at rest. Some patients may present with wheezing because of airflow obstruction. As COPD advances, patients can lose significant body weight due to systemic inflammation and increased energy spent in the work of breathing. Also, there are frequent intermittent exacerbations as the obstruction of the airways increases. Episodes of COPD exacerbations may present with increased shortness of breath, increased severity of a cough, and increased sputum, typically brought on by an infection or an environmental factor.
Smoking history is important, with an emphasis on the age at which the person started smoking and the total pack years. If the person has quit smoking, it is important to know how many years have passed since he/she last smoked. A history of environmental and occupational exposure and a family history of chronic respiratory conditions and COPD is essential. The physical examination may be normal in the early stages of the disease. Patients with emphysema are typically called “pink puffers,” meaning cachectic and non-cyanotic. Expiration through pursed lips increases airway pressure and prevents airway collapse during respiration, and the use of accessory muscles of respiration indicates advanced disease. Clubbing of the digits is not typical of COPD. Many other comorbidities may be possible. Current smokers may have an odor of smoke and nicotine staining of hands and fingernails. Percussion may be normal early in the disease. The rest of the examination may range from prolonged expiration or wheezes on forced exhalation to increased resonance, indicating hyperinflation as the airway obstruction increases. Distant breath sounds, wheezes, crackles at the lung bases, or distant heart sounds are heard on auscultation.
Evaluation
Emphysema is a pathological diagnosis. Accordingly, routine laboratory and radiographic studies are not indicated. Pulmonary function testing (PFT), particularly spirometry, is the mainstay of diagnosis. A postbronchodilator test may be done in those with abnormal values. COPD is only partially reversible or irreversible with a bronchodilator, and post-bronchodilator FEV1/FVC is less than 0.07, which is diagnostic.[8][9][10][11]
GOLD staging based on the severity of airflow limitation is as follows:
- Mild with FEV1 greater or equal to 80% predicted
- Moderate with FEV1 less than 80% predicted
- Severe with FEV1 less than 50% predicted
- Very severe with FEV1 less than 30% predicted
The lung volume measurements of air trapping in emphysema reveal increased residual volume and total lung capacity. Diffusing capacity for carbon monoxide is reduced due to the emphysematous destruction of the alveolar-capillary pulmonary membrane. A chest x-ray is only helpful in diagnosis if emphysema is severe, but it is usually the first step when suspecting COPD to rule out other causes. Destruction of alveoli and air trapping causes hyperinflation of the lungs with flattening of the diaphragm, and the heart appears elongated and tubular. See Image. X-ray, COPD, Subtle Paraseptal Emphysema. Arterial blood gases are usually not required in mild to moderate COPD. It is done when oxygen saturation goes below 92% or when an assessment of hypercapnia is needed in severe airflow obstruction. A young person with symptoms of emphysema should be tested for AATD.
Treatment / Management
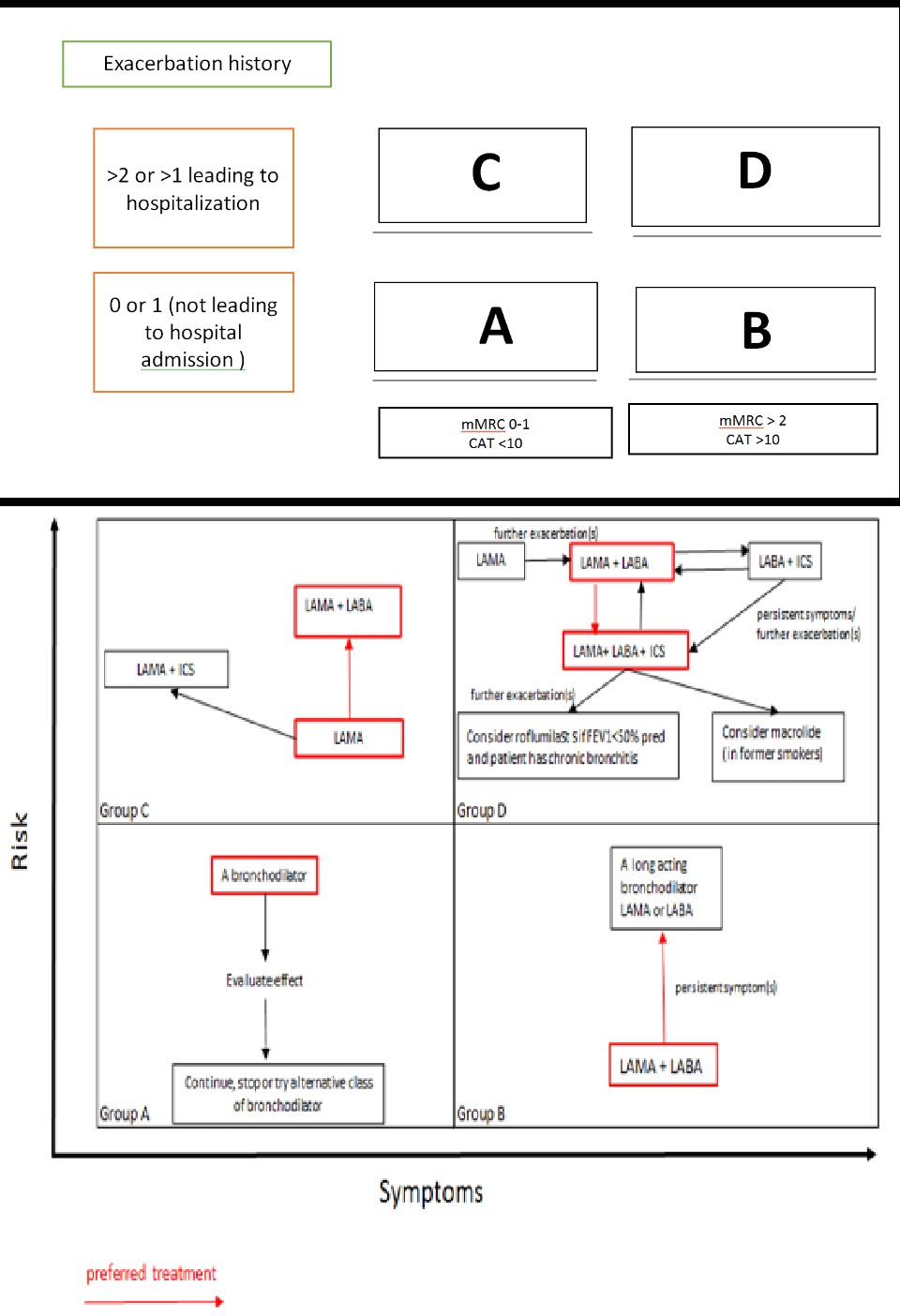
There is no known, definitive treatment that can modify the disease process. However, risk-factor modification and management of symptoms have been proven effective in slowing the disease progression and optimizing the quality of life.[12][13][14] Based on the symptoms and number of exacerbations, we can divide the disease into 4 COPD GOLD stages and modify the treatment accordingly.
Medical Therapy
Medical therapy includes using a bronchodilator alone or with anti-inflammatory drugs such as corticosteroids and phosphodiesterase-4 inhibitors.
Bronchodilator
The primary mechanisms of action can be divided into 2 categories: beta2 agonists and anticholinergic medications. They are first-line drugs for COPD and are administered by inhalation. They are known to improve FEV1 by altering the smooth muscle tone of the airways and thus improving exercise tolerance. Bronchodilators are usually given regularly to prevent and reduce symptoms, exacerbations, and hospitalizations. Short-acting beta2 agonists (SABA) and short-acting muscarinic antagonists (SAMA) are usually prescribed as needed for the management of intermittent dyspnea. Long-acting beta2 agonists (LABA) and long-acting muscarinic antagonists (LAMA) are used, especially in increasing dyspnea or more than occasional dyspnea. If the symptoms are persistent while on 1 bronchodilator, another bronchodilator should be added. Beta2 agonists cause relaxation of airway smooth muscles. SABA, like albuterol, can be used with or without anticholinergics. SABA is the mainstay in COPD exacerbation. LABA includes formoterol, salmeterol, indacaterol, olodaterol, vilanterol, among others. The side effects are arrhythmias, tremors, and hypokalemia. Caution should be taken in heart failure as tachycardia may precipitate heart failure. Anticholinergics inhibit acetyl-choline-induced bronchoconstriction. SAMA includes ipratropium and oxitropium. LAMA, such as tiotropium, can be given once daily.
Inhaled corticosteroid (ICS) is an add-on therapy to bronchodilators in a step-up therapy. ICS includes beclomethasone, budesonide, fluticasone, etc. The common side effects are local infection, cough, and pneumonia. Oral systemic corticosteroids are used for all patients with COPD exacerbation and are avoided in stable patients due to more adverse effects.
Oral Phosphodiesterase-4 inhibitors like roflumilast act by reducing inflammation and can be added if there is severe airflow obstruction with no improvement with the above medications.
Triple inhaled therapy (LABA+ LAMA+ ICS) has been recently approved by the FDA and is taken only once a day.
Intravenous alpha1 antitrypsin augmentation therapy for AATD patients. The high cost and lack of availability are the main limitations of this therapy.
Supportive Therapy
Supportive therapy includes oxygen therapy, ventilatory support, pulmonary rehabilitation, and palliative care.
Routine supplemental oxygen does not improve the quality of life or clinical outcomes in stable patients. Continuous long-term, ie, longer than 15 hours of supplemental oxygen, is recommended in patients with COPD with PaO2 less than 55 mmHg (or oxygen saturation less than 88%) or PaO2 less than 59 mm Hg in case of cor pulmonale. Oxygen therapy has been shown to increase the survival of these patients with severe resting hypoxemia. For those who desaturate with exercise, intermittent oxygen helps. The goal is to maintain oxygen saturation greater than 90%. A major cause of hypoxemia in COPD is ventilation-perfusion mismatch (V/Q mismatch), particularly in low V/Q areas. Hypoxic vasoconstriction of pulmonary arteries is to improve overall gas exchange efficiency. Supplemental oxygen can successfully reach the alveoli in these lungs, which prevents this vasoconstriction and thereby increases perfusion and improves gas exchange, thus improving hypoxemia.
Noninvasive positive pressure ventilation decreases morbidity and mortality in patients with acute respiratory failure. It should be tried as the first mode of ventilation in patients with COPD exacerbation with respiratory failure who otherwise have no absolute contraindication. It improves gas exchange, decreases hospitalization duration, reduces work of breathing, improves VQ matching, and improves survival. If noninvasive positive pressure ventilation does not work in a patient with COPD in a hospital setting, the patient should be intubated and put on a ventilator.
Pulmonary rehabilitation for patients with severe symptoms and multiple exacerbations reduces dyspnea and hospitalizations and is recommended for GOLD stages B, C, and D. Although available from the time the person is diagnosed with COPD, palliative care is typically recommended for GOLD stage D. It is additional care to the patient's ongoing treatment plan. The goal is to provide the best quality of life possible. Not only does it play a role in assessing and managing the symptoms, but it also helps patients understand their illness and facilitates a discussion about the patient's goal of care, advanced care, and end-of-life care plans. Advance care planning involves communication between patients, their families, and the physician and helps patients formulate their treatment preferences. Reassuring patients with a clear plan to deal with dyspnea in advanced disease and management of depression and anxiety is an important component of palliative care. These can be managed with low-dose opioids, lifestyle modification, and relaxation techniques, respectively. Most patients underestimate the disease, so looking for transition time and discussing advanced care early in the disease is important. It is also important to explore where the patients want to spend their last days (eg, home or hospital) and help provide them with as much comfort as possible.
Interventional Therapy
- Lung volume reduction surgery reduces hyperinflation and improves elastic recoil.
- Lung transplantation when FEV1 and or DLCO is less than 20%.
Additional Interventions
- Identification and reduction of exposure to risk factors. Counseling about smoking cessation is the single most important intervention that slows the progression of the disease. Reducing exposure to open cooking fires and promoting efficient ventilation are also beneficial.
- Daily oral opioids for severe COPD symptoms refractory to medical therapy. Nutritional supplementation in malnourished patients with COPD
- Pneumococcal vaccine 23 valent every 5 years for patients with COPD older than 65 or with other cardiopulmonary disease and Influenza vaccine for all patients with COPD every year
- Readmission rates can be reduced with counseling on the optimal use of metered-dose inhalers
- Exercise for all patients with COPD
Management of a Patient with COPD Exacerbation
Beta-blockers and anticholinergics are used simultaneously. Initially, with nebulizers and later switched to metered-dose-inhalers. Systemic corticosteroids (intravenous or oral) are shown to hasten recovery and decrease hospital stays. Antibiotics are beneficial, especially if a cough productive of purulent sputum is present. Second-generation macrolides, extended-spectrum fluoroquinolones, cephalosporins, and amoxicillin-clavulanate. NIPPV can be beneficial in patients who can protect their airways and do not have a major acid-base disorder on the ABG. Very often, patients with end-stage COPD with exacerbations are intubated and put on a ventilator. Ventilated patients should be watched for the development of auto-PEEP and its related complications.
Prevention
- Smoking cessation
- Vaccination against Pneumococcus and Haemophilus Influenzae.[15][16]
Differential Diagnosis
The disease presents with nonspecific symptoms and has broad differential diagnoses (see Image. Subcutaneous Emphysema). These include:
- Chronic obstructive asthma
- Chronic bronchitis with normal spirometry
- Cystic fibrosis
- Bronchopulmonary mycosis
- Central airway obstruction
- Bronchiectasis
- Heart failure
- Tuberculosis
- Constrictive bronchiolitis
- Anemia
- Complications
- Pulmonary hypertension
- Cor pulmonale
- Chronic respiratory failure
- Spontaneous pneumothorax
Prognosis
Various prognostic indicators have been evaluated concerning mortality and morbidity associated with emphysema. The following measures have been correlated with the disease burden and prognosis:
- FEV1
- DLCO (diffusion capacity for carbon monoxide)
- Blood gas measurements
- BMI
- Exercise capacity
- Clinical state
- Radiographic severity[17]
The coexistence of other illnesses also makes the prognosis poorer in COPD patients. For instance, patients with features of both asthma and COPD have a poorer quality of life with higher mortality rates. Similarly, patients with emphysema who have raised serum alpha-1 antitrypsin levels also have higher mortality.[18] Other frequently encountered comorbid illnesses include metabolic syndrome, cardiovascular disease, hypertension, and bronchiectasis.[19]
A widely used tool for prognosis prediction is the BODE index, which takes into account the following:
- BMI
- FEV (obstruction)
- Dyspnea
- Exercise capacity
Complications
Patients suffering from emphysema are prone to develop various complications, some of which are life-threatening. Following are some of the most frequently encountered complications of emphysema:
- Respiratory insufficiency or failure
- Pneumonia
- Pneumothorax
- Chronic atelectasis
- Cor pulmonale
- Interstitial emphysema
- Recurrent respiratory tract infections
- Respiratory acidosis, hypoxia, and coma
Consultations
An internist, an emergency physician, a pulmonary specialist, specialized nurses, respiratory therapists, and physician assistants must all play their part in managing patients with emphysema. A pulmonary specialist's help is to be sought in the following cases:
- When the diagnosis is uncertain
- Persistent symptoms despite initial medical therapy
- Frequent exacerbations despite medical management
- ATTD is diagnosed
- Atypical presentation
- Alarming features (hemoptysis, weight loss, night sweats)
- Coexistence of asthma and COPD
- Other comorbid illnesses
Pearls and Other Issues
Key facts to keep in mind about emphysema are as follows:
- Medications for primary pulmonary hypertension are not recommended for patients with pulmonary hypertension secondary to COPD.
- Depression and anxiety are very common in end-stage lung disease, and pharmacological agents can be used accordingly.
- Statin therapy does not reduce exacerbation.
- Long-term oral corticosteroids are not recommended.
- ICS alone is not recommended.
- Combination treatment with LABA and LAMA is more effective in reducing exacerbations as compared to monotherapy.
- A combination of SAMA and SABA improves symptoms and FEV-1.
- Theophylline has little bronchodilator effect in stable COPD and is associated with modest symptomatic benefits.
- Assessment and appropriate management for comorbidities in a patient with COPD independently influence mortality and hospitalizations.
- Excessive correction of hypoxia in a patient with longstanding COPD can sometimes lead to hypercapnia. This is due to the loss of compensatory vasoconstriction with ineffective gas exchange, as there is a loss of hypoxic drive for ventilation. Also, increased oxyhemoglobin decreases the uptake of carbon dioxide due to the Haldane effect.
- The only interventions that decrease the mortality of COPD are smoking cessation and continuous home oxygen.
Enhancing Healthcare Team Outcomes
The management of emphysema is by an interprofessional team that consists of a pulmonologist, internist, pharmacist, dietitian, social worker, respiratory therapist, primary care provider, and a thoracic surgeon. There is no cure for emphysema, and the primary cause needs to be treated. This means educating the patient about the harms of smoking and getting the annual influenza vaccine. The outlook for most patients is guarded, and the quality of life is poor, marked by frequent exacerbations and remissions of acute respiratory distress. Some may develop repeated pneumothoraces, which may need to be managed by a thoracic surgeon. Several types of lung volume reduction procedures are available, but they are high-risk, associated with serious complications, and require prolonged intensive care. Pharmacists must review prescriptions, check for interactions, and stress the importance of compliance to patients and their families. Nurses should monitor and educate patients, reporting changes in status to the team.[2][20]