Continuing Education Activity
The diagnosis of traumatic diaphragm injuries (TDI) can be difficult but is critical, as a delayed diagnosis can carry significant sequelae. TDIs can occur with both penetrating and blunt trauma and are often occult. Patients may vary in their presentation based on the extent and location of injury (right versus left hemidiaphragm), the presence and extent of abdominal viscera displacement, and the presence of other injuries. For this reason, the mechanism of injury (MOI) plays a crucial role in establishing a high index of suspicion for diaphragmatic injuries. The first report of diaphragm herniation was described in 1541, but it wasn't until a few centuries later, in 1853, that Bowditch diagnosed the first antemortem diaphragmatic injury secondary to trauma. This activity reviews the evaluation and management of traumatic diaphragm injuries and highlights the role of the trauma team, radiologists, and subspecialties in evaluating and managing patients with this condition.
Objectives:
- Review the anatomy and physiology of the diaphragm.
- Describe the clinical presentation, signs, and symptoms of traumatic diaphragm injuries and summarize the diagnostic approach of a patient with suspected diaphragm injury/rupture.
- Understand the treatment and management options available for traumatic diaphragmatic injuries and the limitations to each.
- Review the importance of improving care coordination amongst interprofessional team members to improve outcomes for patients with traumatic diaphragm injuries.
Introduction
The diagnosis of traumatic diaphragm injuries (TDI) can be difficult but is critical, as a delayed diagnosis can carry significant sequelae. TDIs can occur with both penetrating and blunt trauma and are often occult. Patients may vary in their presentation based on the extent and location of injury (right versus left hemidiaphragm), the presence and extent of abdominal viscera displacement, and the presence of other injuries. For this reason, the mechanism of injury (MOI) plays a crucial role in establishing a high index of suspicion for diaphragmatic injuries. The first report of diaphragm herniation was described in 1541, but it wasn't until a few centuries later, in 1853, that Bowditch diagnosed the first antemortem diaphragmatic injury secondary to trauma. The first successful traumatic diaphragm injury repair was completed in 1888.[1]
The embryologic development of the diaphragm originates from the septum transversum during the 4th week of gestation. Additional tissue contribution is supplied by the esophageal mesentery, pleuroperitoneal membranes, and chest wall muscle. After development, the diaphragm is conformed into a domelike muscle with a tendinous central septum. It attaches to the sternum, sixth through twelfth ribs, the last thoracic vertebra, and the first three lumbar vertebrae. Its most important function is in respiration, but it also provides a floor for the thoracic cavity and a partition between the abdomen and thorax. It provides additional power with expulsive maneuvers such as defecation and vomiting by contributing to the changes in intra-thoracic and intra-abdominal pressure gradients. The diaphragm is innervated by the phrenic nerve, which originates from the third through fifth cervical roots. The nerve transverses the thorax in the posterolateral mediastinum and branches at the level of the diaphragm. There is a small contribution to the sensory component of the diaphragm along the periphery, which arises anterolaterally from the intercostal innervation.
A traumatic diaphragm injury's overall incidence is exceedingly low, but prompt diagnosis is essential, as a missed injury is associated with significant morbidity and mortality (30 to 60%).[1][2] Morbidity can include anything from organ herniation and strangulation to severe respiratory compromise and even death.[3][4] Currently, there is no accepted standard in diagnostic modalities that have been shown to accurately and consistently detect the presence of a diaphragm injury. A review of the literature suggests varying reports of the successful use of high-resolution CT versus laparoscopy in early diagnosis.[1][3][5]
Appropriate management of TDIs is highly dependent on the type of diaphragm injury (blunt versus penetrating), hemodynamic stability, the timing of diagnosis, and the presence of contamination. Blunt injuries tend to be larger and require more in-depth repair, whereas penetrating injuries are usually reapproximated primarily with little difficulty. If patients are hemodynamically unstable, TDI repair may need to wait until a later time when the patient has been fully resuscitated. An acute versus delayed diagnosis dictates the surgical approach, which can vary from an open to minimally invasive abdominal versus thoracic approach. Diaphragm repairs include primary suture repair, prosthetic mesh placement, and in worse cases, diaphragm reconstruction. The type of repair is also partially dependent on whether the diagnosis is acute or delayed. Occasionally, in extreme cases, reconstruction may be required in a staged approach with the use of myocutaneous and rotational muscle flaps to redevelop thoracoabdominal integrity.[6]
Etiology
The etiology of traumatic diaphragm injuries occurs via blunt and penetrating injuries. Blunt mechanisms include motor vehicle accidents, falls from a significant height, or pedestrian strikes. Penetrating injuries can include gunshot wounds, stab wounds, or any foreign object which transverses the diaphragm disrupting the thoracoabdominal partition.
When at rest, the diaphragm is a concave tendinous structure. This downward projection towards the abdominal cavity at rest causes compression on the abdominal contents, which results in an outward projection of the abdominal wall. The chest wall is lowered, and the vertical diameter of the chest decreases. The presence of recoil brings the thorax back to its original position in exhalation. The diaphragm contracts and loses shape to a taut central tendon which becomes flat. This helps to expel air out of the lungs. With the exchange of air, the displacement of the diaphragm varies between one and two inches.[1] The ongoing diaphragmatic motion preserves the intrathoracic negative pressure gradient.
In blunt trauma, an abrupt increase in the pleuroperitoneal gradient causes an increase in kinetic energy transfer to the diaphragm, which results in the disruption. Petrone and colleagues [1] have suggested that this happens most commonly on the left due to a congenital weakness where fusion occurs during embryologic development. Others have suggested that the right hemidiaphragm is less vulnerable to injury due to the presence of the liver directly beneath it. Fair et al.[3][5][7][8][9] suggests that in addition to acute increases in intra-abdominal pressure from blunt force trauma, the shearing force created in blunt trauma may be responsible for the rupture as the diaphragm is fixed in all directions.
In penetrating trauma, the injury follows the tract of the foreign body and is typically small, with over 80% being smaller than 2 cm.[5][10] More common than blunt are penetrating TDIs, which are also more prevalent on the left side.[7][11] Some suggest this is due to increased mortality associated with right-sided injuries as these injuries tend to carry a greater association with other abdominal injuries.[3] Perhaps the increased mortality reflects the decrease in the number of diagnosed right-sided TDIs in the literature.
Epidemiology
Traumatic diaphragm injuries are relatively uncommon, ranging in the literature from 0.46% to 15%.[2][7] The largest published series to date analyzed 833,309 patients revealing an overall incidence of 0.46%.[2] There are a few potential explanations for the wide variation in the literature. First, it is suspected this may be secondary to the use of the National Trauma Data Bank for data where discrepancies may exist as not all patients are treated at established trauma centers, and therefore the true incidence may be underreported. Secondly, associated injuries are common with TDIs, and it is feasible that there is an underestimated number of patients who are left undiagnosed before death from associated injuries. Lastly, to date, there is a wide variation in management approaches to diaphragm injuries, and a fair number of patients may be treated nonoperatively at initial presentation leading to under-reporting.[2]
TDIs are further divided by their mechanism of injury, blunt versus penetrating. The incidence of TDI secondary to blunt traumas is 1 to 7%. TDI secondary to penetrating injury is approximately 15%.[1][2][3][5] Again, in comparison to the largest sample size for review to date, the suggested incidence of blunt TDIs is 33%, where the suggested incidence of penetrating TDI is 67%.[2] Of these patients, motor vehicle crash was the most common cause of blunt TDI, and gunshot wounds were the most common MOI for penetrating TDIs.[2]
History and Physical
Given the elusive nature of traumatic diaphragm injuries, a high index of suspicion is imperative during the initial workup. It is important in developing an appropriate level of suspicion to obtain the appropriate adjunctive studies where a TDI may be present.[1][12][13] A clinical history involving high-velocity motor vehicle crashes, falls from great heights, a direct blow to the abdomen, thoracoabdominal stabbing, gunshot wounds, and abdominal crush injuries should heighten awareness of the possibility of a TDI with or without herniation.[1]
In situations where the MOI involves a fall, the fall height and how the patient was found are important in providing clues to the degree and trajectory of energy at the time of impact.[1] In the case of motor vehicle crashes, the velocity, degree of vehicular damage, use of vehicle restraints, and details surrounding the extrication of victims will give insight into the suspected energy force involved.[1]This should prompt the anticipation for additional thoracoabdominal injuries where initial pre-hospital presentation may not be so forthcoming.
Scharff and Naunheim [12] report associated intra-abdominal injuries 60 to 100% of the time and associated cardiac injuries in 20% to 60% of all cases. This is further supported by Petrone et al. reported similar findings in their review. They showed an array of injuries in addition to the already anticipated abdominal visceral injuries to include pelvic fractures (40% to 55%), long bone fractures (75%), and closed head injuries (42%). Presentation directly attributed to a TDI may range from no symptoms at all to hypotension, respiratory compromise, and even death. Without a high index of suspicion, the non-specific symptomology could easily be attributed to the obvious clinical injuries that are present, resulting in a missed diagnosis. This is especially true in cases of TDI without herniation, where the associated injuries are treated non-operatively. In acute patients, they may report shoulder or epigastric pain with respiratory distress. These symptoms are non-specific and can be easily overlooked in a patient where you are suspecting injury to the liver, spleen, or lung.
For those patients who present in a delayed fashion, their diaphragmatic injury often includes herniation of abdominal viscera. Symptoms here depend on the size of the diaphragmatic defect, which tends to increase over time. The physical findings can vary based on the anatomical point of obstruction and the severity of the herniation. Incarcerated viscera may present with partial obstructing symptoms, whereas strangulated viscera presents with a more grave clinical picture, leading to ischemia and impending perforation with septic shock.[1]
A history of prior trauma may elude to the potential for a delayed traumatic diaphragmatic hernia. Patients often have non-specific symptoms of nausea, vomiting, and pain. This may be mistaken for peptic ulcer disease or cholecystitis in the herniated viscera without incarceration, especially if the presentation is chronic.[12] Small bowel herniation with incarceration will present as a small bowel obstruction. Patients may experience nausea, vomiting, retching, and PO intolerance. They may have abdominal distention and tympany. Bowel sounds are often present within the chest cavity. Patients with a gastric herniation may present as a classic gastric volvulus with nausea, retching, and foamy saliva.[12] Abdominal distention in these patients may not be so obvious. Tympany is less likely as the obstructive point is more proximal. With colonic herniation, patients may have abdominal distention and bowel sounds located in the chest. As the obstruction worsens, the bowel becomes increasingly distended, and patients typically develop respiratory distress. The size of the hernia and the progressive dilation of the bowel cause worsening dyspnea, chest pain, and orthopnea.[1] Patients may present as a tension pneumothorax as the space allotted for lung expansion is occupied by the abdominal viscera.
Evaluation
The definitive diagnosis of traumatic diaphragm injury is one of both inclusion and exclusion. There are no specific laboratory finding which directly diagnoses this entity. Basic chemistries, hepatic panel, and pancreatic enzymes can help to rule out injuries to the liver or pancreas. Unfortunately, these numbers are not directly helpful nor reliable in acute trauma patients.
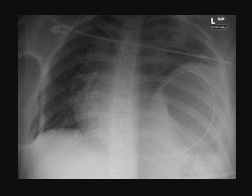
In a stable patient without an indication for emergent operative intervention, imaging studies are obtained secondary to the physical exam. Typically, a chest x-ray is the initial preferred study.[1][14] According to Bocchini et al., this is normal or non-specific 20% to 50% of the time. Additional literature supports subtle signs of diaphragmatic injury on CXR in 27% to 68% of cases.[14] The chest imaging may be immediately diagnostic in the case of significant herniation where bowel content is visualized in the chest cavity. In this instance, air-fluid levels are present above the level of the diaphragm. Additionally, a nasogastric tube may hint to TDI if it transverses the diaphragm with its apex terminating back into the chest (Fig 1). In the acute phase, if the defect is small, organ displacement into the chest may not be present. This does not exclude the potential for a TDI as these films are read as normal approximately 50% of the time.[1] Subtle but non-specific findings precluding TDIs may include atelectasis, pneumothorax, hemothorax, and/or pulmonary contusion. These may also be present in the setting of trauma without TDI making additional work up imperative. Petrone and colleagues suggest that regardless of the presence of a diaphragmatic hernia on a chest x-ray, an abnormal elevation of the diaphragm suggests a TDI on the ipsilateral side. This has been disputed by Bocchini et al.[14] as a hemidiaphragm elevation may accompany pleural effusions, eventration, and phrenic nerve paralysis. They found the accuracy in appropriately identifying a TDI with a hemidiaphragm sign to be 61%. Therefore, although the first test obtained is usually a chest x-ray, it should never be used exclusively to detect the presence of a TDI. Patients should be further evaluated with either invasive or additional non-invasive studies.
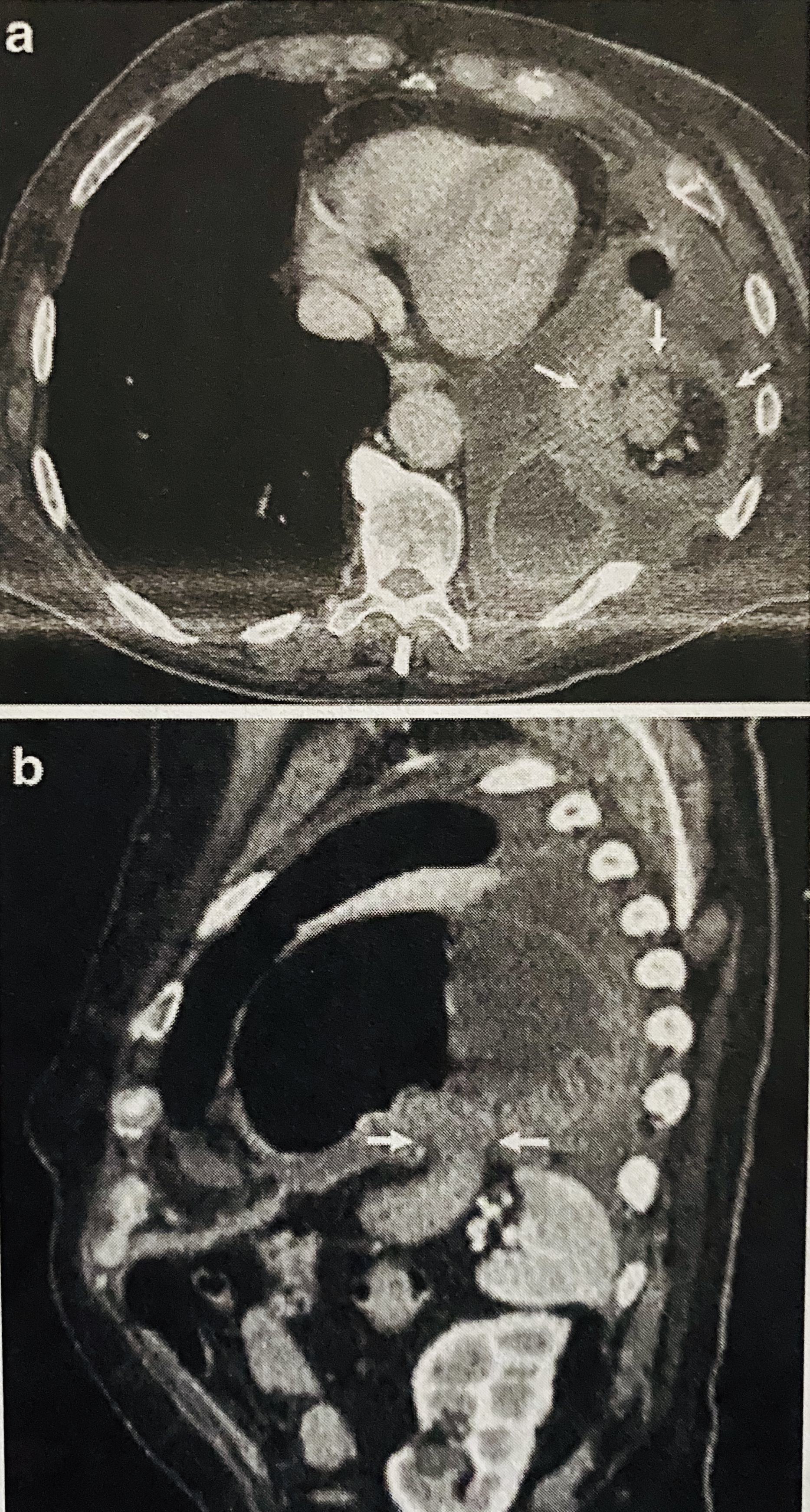
Although chest x-ray is the most common initial test in the workup for traumatic diaphragmatic hernias, computerized tomography (CT) is the gold standard.[4][14] Previously, conventional CT scans were used to evaluate the poly-trauma patient. In TDI detection, they have generally been accepted as inaccurate and unacceptable due to their low sensitivity.[11][14] With the advent of multidetector CT scans (MDCT), there has been significant improvement in recognizing these injuries. Multidetector CT with 64-slice or greater provides higher resolution with multiplanar reconstructions in the axial, coronal, and sagittal views. They are performed with double or triple (oral, intravenous, rectal) contrast dye with the potential for CT tractography, which has revolutionized the approach to diagnosing traumatic diaphragm injuries.[5] Where conventional CT fell short with low sensitivity, 64-slice or higher MDCT has improved sensitivity between 73% to 100% with specificity between 75% to 100%.[11] When TDIs are broken down further into blunt traumatic diaphragm rupture and penetrating traumatic diaphragm injury, MDCT yields better results in diagnosing blunt traumatic diaphragm injuries. This is attributed to the fact that blunt TDIs tend to be large and hence, easier to diagnose. Penetrating TDIs tend to be exceedingly small (1-2 cm), where the widely accepted radiographic signs accompanying diaphragm injury are generally absent.[4][5][7][15] The choice to proceed with MDCT imaging is at the discretion of the trauma surgeon but generally is reserved for hemodynamically stable patients. Multiple radiographic signs have been studied and are used in the practice of reading and detecting diaphragmatic injuries. They can be broken down into direct and indirect signs.
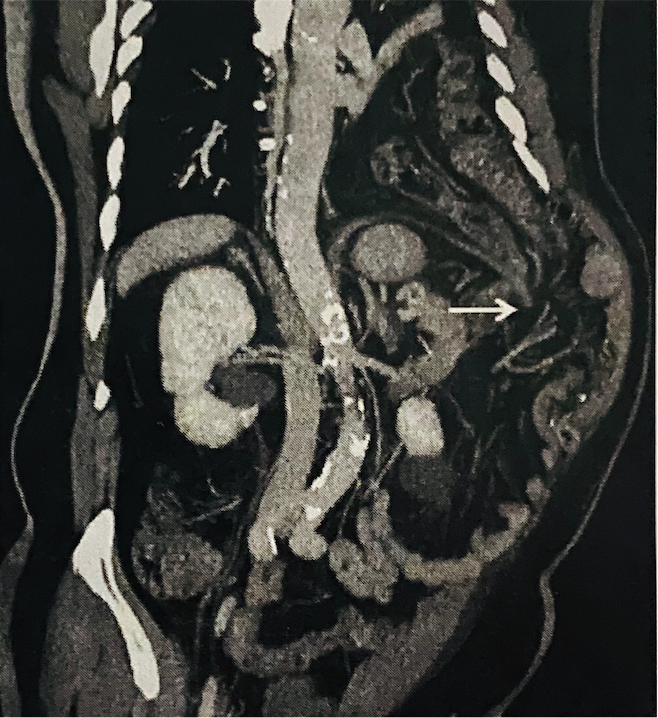
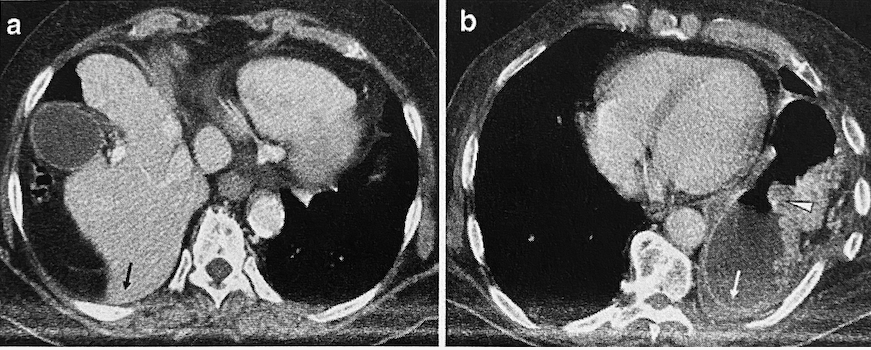
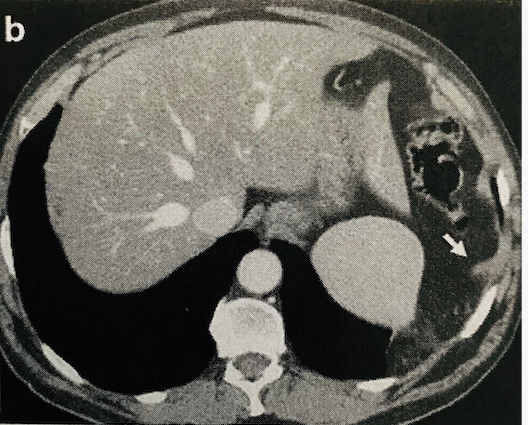
Direct signs include diaphragmatic discontinuity, intrathoracic visceral herniation, collar sign, dependent viscera sign, diaphragm thickening, and dangling sign. Diaphragm discontinuity is the loss of diaphragm integrity on imaging in the presence of surrounding muscle thickening (Fig 2). This sign is highly sensitive but not very specific (86% and 68%, respectively), and it can be falsely positive when intra-abdominal or retroperitoneal hematomas are present. An intrathoracic visceral herniation is the most sensitive and specific of all direct signs. However, it only encompasses a very small subset of patients as most patients do not present with frank organ herniation. Collar sign is defined as a waist-like constriction of the herniated viscera at the site of injury. This produces an appearance of severe compression (Fig 3).[14] It is more likely to be seen with left-sided TDIs as opposed to the right due to the presence of the liver. When this sign is present on the right, variants tend to exist, known as the hump sign and band sign. These signs are typically observed in the sagittal and coronal reformatted images and refer to a small portion of the liver dome which has herniated through the diaphragmatic defect to create a "hump" appearance. When this is present, it may be accompanied by a sliver of low attenuated liver parenchyma at the rupture site. This is known as the band sign, and it represents low perfusion due to compression in comparison to surrounding normal enhancement seen with administration of IV contrast in normal liver tissue. Dependent viscera sign is the loss of separation between the abdominal organs and the posterior thoracic wall where the costophrenic sulcus becomes obliterated (Fig 4). Typically, this sign is only present with larger defects. Dangling sign (Fig 5) is described by the inward curling of the free edge of the diaphragm that has avulsed away from its peripheral attachments giving the appearance of a comma.[14] The main problem with all of these signs is that they rarely present together, and none of these share both high sensitivity and specificity.
According to Bocchini et al., indirect signs associated with TDIs include elevated hemidiaphragm, high ISS (injury severity score) and AIS (abbreviated injury severity) scores, associated injuries, and peri-diaphragmatic bleeding. An elevated hemidiaphragm may be appreciated without the presence of a TDI, especially when intra-abdominal bleeding is present. It may also be a normal variant in some patients where congenital diaphragmatic anomalies exist. Associated injuries such as rib fractures, hemothorax, pneumothorax, pulmonary contusions, atelectasis, and pleural effusions should allude to the possibility of a TDI, but depending on the severity of additional injuries, this may not be the case. Injuries such as internal bleeding, traumatic brain injury, or pelvic fractures tend to take precedence, as these patients are typically unstable. When this is the case, the potential for a diaphragm rupture becomes an afterthought. Contrast extravasation at the level of the diaphragm should always suggest further evaluation into a traumatic diaphragm injury. These signs, both direct and indirect, are traditional teaching in the radiographic diagnosis of traumatic diaphragm injury.[11][14][15][16][17] Hammer et al. reported high reliability of the following radiographic signs: dependent viscera, intrathoracic viscera herniation, hemidiaphragm elevation, and wound track transversion of the diaphragm. Unfortunately, they recognize the limitation of these signs in that they almost exclusively relate to blunt TDI. They showed that in a prospective attempt to correctly diagnose penetrating TDI, they were far less successful. This is mainly due to the mechanism of how these injuries occur. In blunt trauma, the high kinetic force it requires to create the injury does not exist in penetrating TDIs.
Although ultrasound and magnetic resonance imaging (MRI) may help diagnose diaphragm injuries, they are often not clinically feasible in the poly-traumatized patient.[7] Hemoperitoneum, pneumoperitoneum, and retroperitoneal hematoma may obscure ultrasonographic interpretation of images making this modality less favorable. MRI is typically avoided in the initial presentation of trauma patients. This is because of the instability of trauma patients on arrival, the length of time that is required to obtain the study, and the typical location of MRI, which tends to be distant from the resuscitation area, leading to increased concern for patient safety. Therefore, evaluation of potential traumatic diaphragm injury when there is a high suspicion is typically performed in the operating room. The decision on the operative approach is left to the discretion of the operating surgeon and is typically determined by an index of suspicion, stability of the patient, associated injuries, and the need for surgical intervention secondary to other injuries.
Invasive approaches to evaluate for diaphragm injury include diagnostic peritoneal lavage, laparoscopy, laparotomy, thoracotomy, and video-assisted thoracoscopic surgery (VATS).[4] Petrone et al.[1] has reported diagnostic peritoneal lavage (DPL) to carry low sensitivity in the evaluation of the diaphragm due to the red blood cell count threshold that is required to delineate a positive test. Lack of utility in the use of DPL is further supported by the Western Trauma Association as it adds very little to the treatment algorithms in present-day medicine.[5] A laparoscopy is an option for further evaluation of injury where it has been reported with excellent outcomes in identifying diaphragm injuries.[1][10] It is particularly useful in left-sided penetrating TDIs. Petrone et al.[1] advocate that all stable patients with left-sided penetrating thoracoabdominal injuries should undergo laparoscopy to evaluate for diaphragm injury. Thoracoscopy is also used for the definitive evaluation of these injuries, with an accuracy rate nearing 100%.[1] Perhaps the lack of popularity with such a technique can be attributed to intraoperative patient positioning, difficult visibility to perform the repair, and the surgeon's level of comfort with the procedure.
Treatment / Management
Surgical management of traumatic diaphragm injuries varies based on patient presentation, mechanism of injury, associated injuries, and the need for immediate surgical intervention. Early management of the trauma patient consists of a concise and rapid assessment to identify and address life-threatening injuries. Those patients presenting in hemorrhagic shock or with systolic blood pressure less than 90 mm Hg are considered unstable and should receive immediate resuscitation as per Advanced Trauma Life Support (ATLS) guidelines. Adjunctive procedures such as intubation or chest tube placement should be performed as indicated during the primary and secondary surveys. In an unstable patient, the chest x-ray is typically still performed but at the discretion of the trauma surgeon. As previously mentioned, signs of diaphragmatic injury may or may not exist on initial chest x-ray, but moreover, are often either missed or overlooked due to the severity of associated injuries or lack of supporting symptomology.[4][5]
Amid instability, regardless of mechanism, patients should proceed immediately to the operating room, where an exploratory surgery is indicated to combat life-threatening injuries.[5][7] The trauma surgeon must maintain a high index of suspicion for TDI. Once patient stabilization has been achieved, the trauma surgeon is obligated to establish if a definitive diaphragmatic injury exists. These injuries should be repaired immediately when possible as they do not heal but tend to worsen over time.[7] The benefit of laparotomy is that it provides good exposure for the repair of TDIs as well as definitive management of associated intra-abdominal injuries. In the critically ill patient who remains hemodynamically unstable despite resuscitation, damage control surgery is performed, and the diaphragm injury is left for repair at a later time when stability has been obtained.[14]
In the hemodynamically stable patient, surgical intervention is more obscure. The mechanism of injury plays a major role in the decision to perform surgery. According to McDonald et al.[2], a ten study review yielded a total of 208 hemodynamically stable patients with suspected TDI. Of these, only three (1.4%) were due to blunt mechanisms. This suggests that patients with blunt TDI do not commonly present in a stable fashion. This is because of the force required to create the injury in the first place. These patients will more than not progress to laparotomy as associated injuries and instability are more likely.
Penetrating injuries are more commonly reported in the literature and usually present with minimal to no clinical signs, strengthening the argument to assess these wounds with laparoscopy as a standard approach. According to the Western Trauma Association, the controversy as to whether high-resolution MDCT is sufficient to detect diaphragm injuries has not been resolved. They support the findings in the literature, which suggest a 40% incidence of missed injury in the left thoracoabdominal region with penetrating thoracoabdominal wounds. They recommend diagnostic laparoscopy in these patients as the standard modality to further assess for TDI. This is further supported as a practice management guideline by the Eastern Association for the Surgery of Trauma.[2][5][2] The concepts of basic laparoscopic surgery should be maintained. Patients are not candidates if they have a clinically significant traumatic brain injury, become unstable, or are suspected of having associated injuries spanning more than one body cavity.[18] A supra-umbilical incision is made, and access is gained into the peritoneum via a Veress needle or cut-down technique. Pneumoperitoneum is achieved, and 2-3 additional 5 mm ports are placed under direct vision adjacent and inferior to the site of injury, most commonly in the mid-clavicular and anterior axillary lines.[18] If technically feasible, the thoracic cavity should be assessed through the diaphragmatic defect without enlarging the defect. This helps to ensure that no thoracic injuries exist and that an iatrogenic pneumothorax has not been created with insufflation. The remainder of the procedure is completed using the classic principles of hernia repair. Penetrating wounds on the right side of the diaphragm are more difficult to evaluate laparoscopically due to the presence of the liver. The Eastern Association for the Surgery of Trauma [2] recommends proceeding with thoracoscopy in these cases. Video-assisted thoracoscopic surgery (VATS) is a reliable option when laparoscopy is suspected to be inadequate, such as in the case of multiple prior abdominal surgeries, suspected right-sided injuries, or less ideal body habitus lending to decreased visibility.[5][12] The limitation of VATS lies in its inability to simultaneous assess for associated intra-abdominal injuries and how facile the surgeon may be in a trans-thoracic approach.
The approach, be it open, laparoscopic, or thoracoscopic, demands a thorough examination of the diaphragm. In laparotomy, this necessitates takedown of the falciform ligament and potentially the associated liver attachments to palpate and visualize the posterior right side of the diaphragm. Regardless of the approach, once a TDI has been identified, the principles of repair remain the same. If herniated viscera exist, they must be reduced and carefully inspected to rule out hollow organ perforation or clinically significant ischemia.[7] All hernia contents should be placed back into anatomical position or resected in the case of irreversible damage. If the wound is contaminated with enteric contents, foreign debris, or devitalized tissue, the wound should be well irrigated and appropriately debrided. The diaphragm is then re-approximated using interrupted non-absorbable sutures such as polyester or polypropylene.[7][10][18] Petrone et al. suggest a running locking suture followed by a layer of reinforced interrupted sutures. Techniques are variable throughout the literature, but regardless of the approach, the integrity of the repair should be assessed before the completion of the operation.[7] This is accomplished by submerging the repair under saline and having anesthesia produce intentional increased intra-thoracic pressure. A positive test will reveal air bubbles which confirms inadequate repair requiring revision. A key component of the procedure is to reduce as much pneumothorax as possible before the completion of the repair. A common approach is to place a chest tube in the ipsilateral thorax. In unstable patients, this may be done before operative intervention. However, regardless of timing, the importance of this step is maintaining respiratory stability and avoiding inadvertent and unrecognized tension pneumothorax. When the pericardial space has been violated, this should be opened and irrigated. The judicious use of chest tubes is encouraged for wide drainage of this area in the face of gross contamination. Depending on the size of the defect, reconstruction may be required, including rotational or myocutaneous muscle flaps.[1] Lastly, the synthetic non-absorbable mesh material may be required when re-approximation of the diaphragm is not possible. In the event of immediate repair, mesh use is rarely needed. It is contraindicated in the contaminated field. It should be recognized that a gold standard in diaphragmatic repair has not yet been achieved. Multiple approaches exist, and these are inconsistent amongst experts. Furthermore, very few, if any, prospective randomized control trials exist to provide solid evidence in support of one approach versus another.
Delayed diagnoses in missed TDIs follow the same concepts as the immediate repair, with a few exceptions. First, these patients have a progressive clinical course owing to pain, intermittent obstruction, strangulation, and in some cases, perforation. Addressing the potential contamination that accompanies these hernias is the same: debridement, irrigation, contamination control, and wide drainage. Second, the diaphragm tends to regress laterally over time. A missed injury is subject to an inability to reapproximate the tissue, primarily when repaired at a later date. These require non-absorbable prosthetic mesh placement to bridge the defect. In a delayed fashion, Petrone et al. recommend approaching these defects via thoracotomy to avoid inadvertent injury from potential associated intra-abdominal adhesions.[1]
Differential Diagnosis
In the initial workup for traumatic diaphragmatic injury, the differential diagnosis is much more extensive in blunt trauma. This is due to the magnitude of associated injuries that produce nonspecific signs seen on initial imaging, such as pneumothorax, pulmonary contusion, atelectasis, and hemothorax. Findings suggestive of diaphragm injury may suggest a phrenic nerve paralysis or injury.[14] In the presence of a defect, not all defects are secondary to trauma. These include congenital or acquired hernias such as Bochdalek, Morgagni, paraesophageal hernias, or a diaphragmatic eventration.[1]
Prognosis
It has been generally accepted in the literature that the prognosis of a traumatic diaphragm injury by itself is good. However, it is the missed injury that later leads to herniation of abdominal viscera and increases morbidity and mortality, making the initial diagnosis so important.[13][19] Morbidity associated with TDIs ranges from atelectasis to prolonged respiratory failure and includes everything in between: pleural effusion, lung abscess, prolonged pneumothorax, empyema, and pneumonia. There is a wide range of reported morbidity with these injuries, but it is presumed these ranges are due more to the underlining health of the patient at the time of injury, not the fact that they suffered a traumatic diaphragm rupture. Further, Zarour et al.[7] found that left diaphragmatic injuries were associated with greater multi-organ injury and longer hospital stays compared with right-sided injuries. The right-sided injury leads to a much higher mortality rate with poorer outcomes (26% versus 17%).[7][9][13]
The overall mortality rate of these injuries ranges anywhere from 4% to 38%.[19][20] Blunt traumatic diaphragm rupture carries a longer length of stay, greater ventilator days, and greater ICU days than penetrating diaphragm injury. Additionally, mortality rates for blunt injuries are much higher than for penetrating injuries. This is because these patients carry greater injury severity scores (ISS), multiple associated injuries, and present in hemorrhagic shock on initial presentation. Cardoso et al. showed mortality to be higher among those with an ISS greater than 25. Not at all surprising, as patients with blunt traumatic diaphragm ruptures are more likely to have injuries spanning two cavities, most commonly, the lung, aorta, spleen, and bladder.[9] Fair et al. proposed a six-fold increase in the likelihood of aortic injury with blunt traumatic diaphragm rupture.[3]
There is little support in the literature to show how these patients do with diaphragmatic repair on their index hospitalization, probably because blunt rupture is less common than penetrating and has worse outcomes. Cardoso et al.[3] showed the direct effect of suture repair alone in their analysis of 103 patients with traumatic diaphragm injury. They concluded that when solely analyzing diaphragm suture repair alone, and all other variables were excluded, the repair, in of itself, was an independent predictor of decreased mortality by 24%. When associated injuries were considered in this analysis, the number of associated injuries increased the predicted mortality. An exclusive diaphragm injury, as seen with penetrating stab wounds, carried 0% mortality. One additional injury increased the mortality rate to 11.1%. Two additional injuries increased mortality to a rate of 20.5% and greater than three injuries to 37.5%. This supports the major difference between penetrating and blunt diaphragmatic injuries and why there is a greater propensity for worse outcomes, longer hospital stays, and increased ICU days.
Complications
Petrone et al. suggests that TDI complications can be subdivided into morbidity as a direct result of the diaphragm repair and secondary to the trauma. Complications associated with the repair include iatrogenic phrenic nerve paralysis and suture dehiscence. Both complications can lead to the need for additional invasive procedures and potentially long-term complications whose details are beyond the scope of this paper. Morbidity associated with traumatic injury varies depending on the presence of associated injuries but could include empyema, subphrenic abscess, and resultant ventilator-dependent respiratory failure. When these patients present in a delayed fashion due to a missed injury, the timeframe to presentation has varied in the literature from a few weeks to years. Complications in this setting such as atelectasis, respiratory failure, pneumonia, bowel obstruction, strangulation, and perforation have all been reported.[1]
Deterrence and Patient Education
Because these types of injuries have an array of mechanisms, it is difficult to provide patient education to prevent. Perhaps, the focus in avoiding these types of injuries should be on overall injury prevention in the most common TDI presentations. For penetrating wounds, this would include education and prevention on knife and gun violence. For blunt TDIs, this would including decreasing the risk of internal injury in the use of motor vehicles by utilizing restraints properly, following traffic regulations, and participating in defensive driving courses.
There is certainly literature supporting the approach of non-operative management in a hemodynamically stable patient with thoracoabdominal trauma. When this is the case, patients should be educated on the risks of missed or undiagnosed injury as well as signs or symptoms that would suggest a need for immediate evaluation. In these patients, where TDI was not definitively ruled out, close follow-up is important. Repeat imaging is suggested at a 6 to 12-month interval to rule out or identify a missed TDI.[2][5]
Enhancing Healthcare Team Outcomes
The approach to any trauma patient is multi-faceted, which requires interprofessional collaboration amongst physicians, nurses, ancillary staff, and sub-specialty providers. On a larger scale, the specialty of Traumatology is a collaborative effort amongst the experts of the field to develop and provide guidelines that are accepted as the standards in the treatment of diagnoses as they relate to trauma. Whether blunt or penetrating, Traumatic diaphragm injuries require the same standardized approach in the initial assessment and work up. The challenge to these patients is a missed injury lending to the necessity for repair months to years later, which increases morbidity and mortality. To minimize the risk of a missed injury, it requires astute awareness in part by the trauma surgeon in understanding or reconstructing the mechanism of injury to anticipate potential injuries. For this to occur, the appropriate and detailed handoff from EMS providers is essential.
Because it has been shown that the initial evaluation is crucial to favorable outcomes, a point of controversy is an agreed-upon standard approach to assess for reliable diagnostic signs on MDCT. Although it has been shown that MDCT has improved the identification of these injuries, the sensitivity and specificity are still highly variable, and the sample size is small. Further, the radiologist's ability to correctly identify imaging signs suggestive of TDI is reviewer-dependent.[5] [Level IV] When treated conservatively, the Western Trauma Association recommends close interval follow-up due to the potential for missed injury on MDCT.[5] [Level IV] This requires coordination with ancillary staff to assure appropriate and timely post-admission follow-up.
Because the incidence of traumatic diaphragmatic injury is low, an abundance of large randomized control trials lacks in the contribution to gold standards for workup, diagnostic imaging, and management strategies. In a combined effort of centers across the nation, The American College of Surgeons National Trauma Data Bank has contributed to the largest study known to date establishing injury patterns associated with traumatic diaphragm injuries.[9] [Level IV] This has helped predict injury patterns such as aortic or pulmonary injuries, which may guide the operative approach or the anticipated need for subspecialty assistance, such as vascular or cardiothoracic surgery. Regardless of the approach, laparotomy, thoracotomy, thoracoscopy, laparoscopy, the principles remain the same, reduction of herniated content and a watertight seal of the defect.[7] [level III]