Continuing Education Activity
The term “crocodile tears” is derived from the ancient belief that crocodiles weep after killing their victims. Crocodile tears syndrome, also known as Bogorad syndrome, is a condition characterized by shedding tears while eating or drinking. Most cases are associated with recovery from Bell palsy. This disorder is also referred to as gustatory lacrimation.
Crocodile tears syndrome is diagnosed clinically based on a history of aberrant lacrimation during eating, often following facial nerve injury or Bell palsy, with Schirmer testing and imaging considered in select cases. Management includes botulinum toxin injections to reduce tearing, while surgical options such as lacrimal gland excision are reserved for refractory cases. Complications may include incomplete symptom resolution, recurrence after botulinum toxin treatment, and unintended surgical effects like dry eye syndrome. The prognosis is generally favorable, with most patients responding well to botulinum toxin therapy, though repeated treatments or surgery may be necessary for long-term relief.
This activity for healthcare professionals is designed to enhance learners' competence in evaluating and managing crocodile tears syndrome. Participants will gain deeper insights into the condition's relevant anatomy, etiology, pathophysiology, risk factors, and presentation. The best diagnostic and therapeutic practices will also be discussed. Improved clinical proficiency will enable clinicians to collaborate more effectively with an interprofessional team, enhancing patient outcomes.
Objectives:
Identify the clinical features and diagnostic results indicative of crocodile tears syndrome.
Implement individualized management approaches for crocodile tears syndrome.
Improve patients' knowledge regarding crocodile tears syndrome's potential causes, management, prognosis, and potential complications to enhance their understanding and adherence to treatment recommendations.
Collaborate with the interprofessional team to educate, treat, and monitor patients with crocodile tears syndrome to improve patient outcomes.
Introduction
The term “crocodile tears” stems from the ancient belief that crocodiles weep after killing their victims. Crocodile tears syndrome, also known as Bogorad syndrome, is a disorder marked by the shedding of tears while eating, chewing, smelling, or drinking in patients recovering from facial nerve (cranial nerve VII) injury. The syndrome is named after F.A. Bogorad, a Russian neuropathologist, and is also referred to as "gustatory lacrimation" or "paroxysmal lacrimation."[1][2]
Crocodile tears syndrome typically occurs as a sequela of facial nerve injury, often following Bell palsy, surgery, or trauma. Aberrant regeneration of the facial nerve leads to the misdirection of its autonomic fibers toward the lacrimal glands instead of the salivary glands, resulting in lacrimal gland stimulation and tearing during mastication. The diagnosis is clinical and may be confirmed through the Schirmer test combined with gustatory stimulation. Management options include botulinum toxin injections to the lacrimal gland, topical anticholinergics, and surgical interventions such as vidian neurectomy in severe cases.[3][4] The prognosis is generally favorable, but symptoms may persist, requiring periodic treatment.
Etiology
Crocodile tears syndrome occurs after facial nerve injury from various causes, most commonly Bell palsy. Other etiologies include trauma, surgery, and infection involving the facial nerve.[5] Multiple theories explain the underlying mechanism of crocodile tears syndrome. The widely accepted theory attributes the condition to aberrant regeneration and misdirection of nerve fibers following Bell palsy or traumatic disruption of the nervus intermedius due to an inappropriate healing response. This process occurs gradually, and symptoms typically appear after 6 months (late onset) of the injury. Another theory suggests ephaptic transmission between damaged nerve fibers, in which a short circuit (artificial synapse) forms between fibers with compromised myelin sheaths.[6][7] This mechanism leads to early-onset symptoms, usually within a month of the injury.[8]
Damage to the nervus intermedius during surgery for acoustic neuroma (vestibular schwannoma) should be avoided, as it can lead to multiple postoperative complications, including crocodile tears syndrome.[9] The nervus intermedius is particularly vulnerable to injury because it lacks perineurium just outside the brainstem, and only about 1/5 of its fibers are myelinated.[10] Additionally, this nerve's location between the acoustic neuroma and the facial nerve increases the risk of damage. Subcapsular or subperineural dissection may help reduce the likelihood of crocodile tears syndrome while preserving facial and cochlear nerve function.
A large study found that crocodile tears syndrome occurred more frequently after microsurgery than after γ knife radiosurgery for vestibular schwannoma.[11] Infectious causes have also been implicated, with cases reported in tuberculoid leprosy, possibly due to nerve damage from lepra bacilli.[12] Bilateral crocodile tears syndrome has been documented following Guillain-Barré syndrome.[13] The condition has also been reported after repeated microvascular decompression of the trigeminal nerve (cranial nerve V) for trigeminal neuralgia.
Anatomy
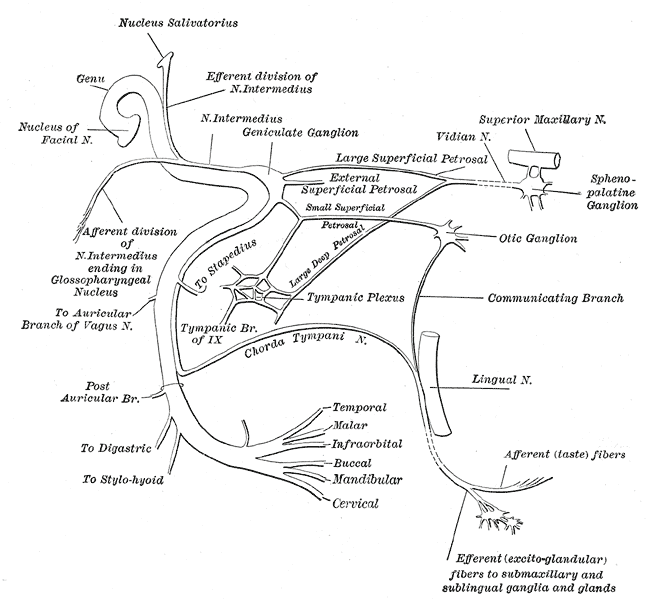
Knowledge of facial nerve anatomy is essential to understanding the etiopathogenesis of crocodile tears syndrome. The facial nerve is a mixed nerve with motor, sensory, and parasympathetic components (see Image. The Facial Nerve).[14]
The special visceral efferent (branchial motor) component innervates the muscles of facial expression, as well as the stylohyoid, the posterior belly of the digastric, and the stapedius muscle, all of which are derived from the 2nd branchial arch. The general visceral efferent (visceral motor) component provides autonomic (parasympathetic) innervation to the lacrimal, salivary, and mucosal glands.
The special visceral afferent (special sensory) component carries taste sensation from the anterior 2/3 of the tongue. The general somatic afferent (general sensory) component transmits sensation from the skin of the concha of the external ear.
Facial nerve nuclei
The facial motor nucleus is a collection of lower motor neurons located in the lower part of the pons. This nucleus sends fibers to the muscles of facial expression and the stapedius. The portion of the facial motor nucleus that supplies the muscles of the lower half of the face receives corticobulbar input from the contralateral hemisphere, while the portion that supplies the upper facial muscles receives bilateral corticobulbar innervation.
Located behind the motor nucleus, the superior salivatory and lacrimatory nuclei serve parasympathetic functions. The superior salivatory nucleus receives input from the hypothalamus and taste sensation from the oral cavity, sending preganglionic fibers to the submandibular and sublingual salivary glands. The lacrimatory nucleus, which governs lacrimal gland function, receives hypothalamic input related to emotional responses. This nucleus also processes sensory information from the trigeminal nerve nuclei, mediating reflex lacrimation in response to corneal or conjunctival irritation.
Facial nerve course and branches
The facial nerve consists of motor and sensory roots. The motor root loops around the abducens (cranial nerve VI) nucleus in the floor of the 4th ventricle and emerges at the junction of the pons and medulla along with the sensory root. Both roots travel alongside the vestibulocochlear nerve (cranial nerve VIII) to reach the internal acoustic meatus, where they fuse at the lower part of the meatus to form a single trunk.
Within the meatus, the facial nerve undergoes 2 bends, dividing it into 3 segments before exiting the skull through the stylomastoid foramen. After crossing the stylomastoid process, the facial nerve enters the parotid gland at its posteromedial surface. At the angle of the mandible, the nerve divides into its terminal branches: temporal, zygomatic, buccal, mandibular, and cervical.
Branches within the facial canal
The greater (superficial) petrosal nerve arises from the geniculate ganglion and carries parasympathetic preganglionic fibers. This nerve continues as the nerve of the pterygoid canal and ultimately synapses with the pterygopalatine ganglion. Postganglionic fibers from this ganglion innervate the mucosal glands of the nose, palate, and pharynx, as well as the lacrimal gland. The nerve to the stapedius supplies the stapedius muscle, which dampens excessive vibrations of the stapes. The chorda tympani carries taste sensation from the anterior 2/3 of the tongue, traveling through the middle ear before reaching the brain.
Parasympathetic supply to the lacrimal gland
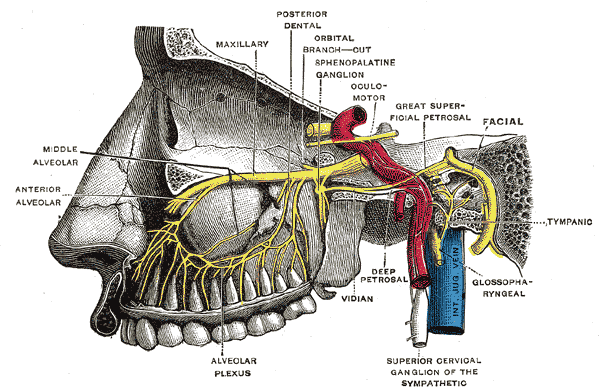
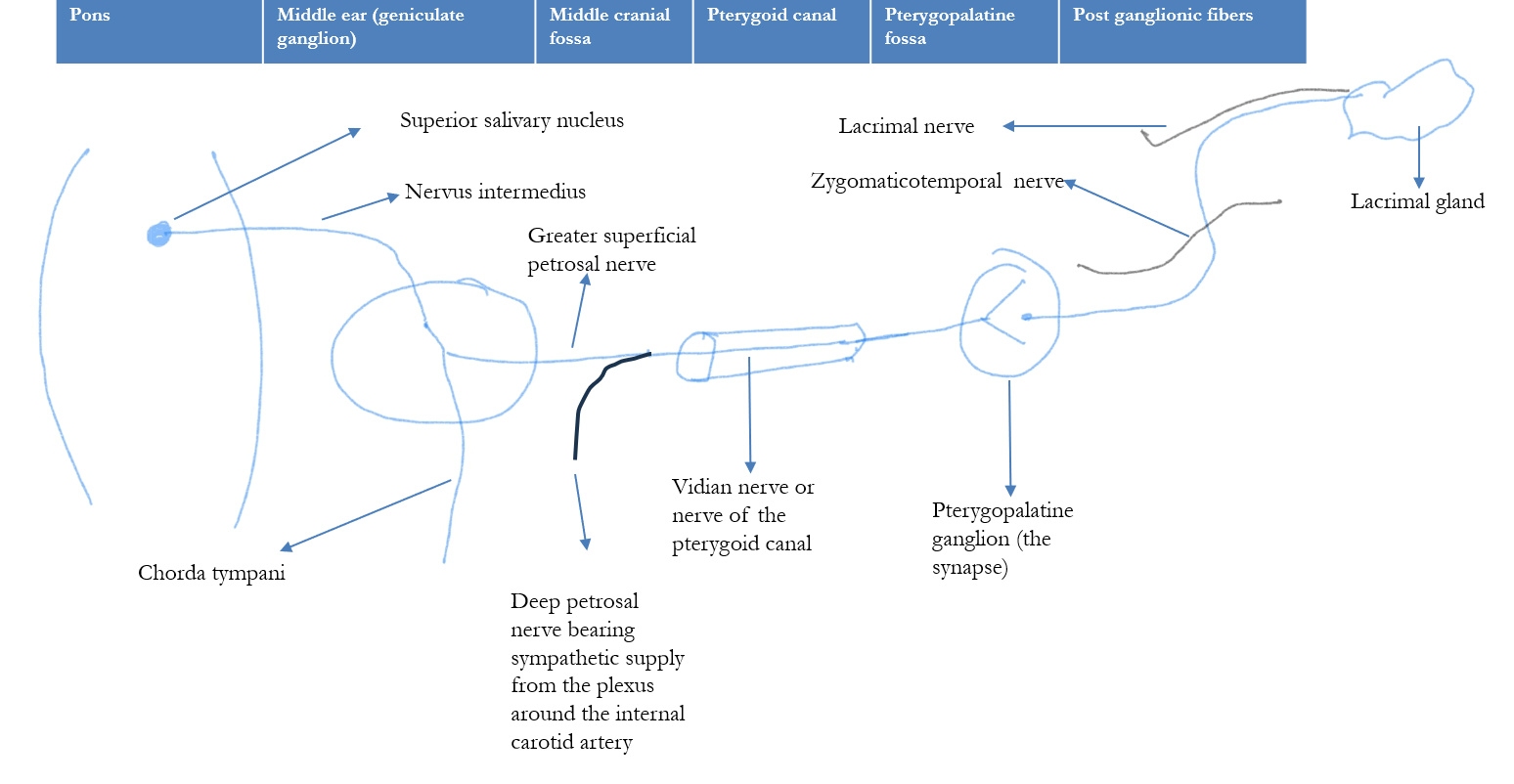
The parasympathetic fibers responsible for lacrimation originate from the superior salivatory nucleus in the pons (see Image. Parasympathetic Innervation of the Lacrimal Gland). These fibers travel via the nervus intermedius of the facial nerve and enter the greater superficial petrosal nerve, a branch of the facial nerve. The greater petrosal nerve merges with the deep petrosal nerve, which carries sympathetic fibers from the sympathetic plexus around the internal carotid artery, forming the nerve of the pterygoid canal, also known as the Vidian nerve (see Image. Facial and Trigeminal Nerve Interactions in Lacrimal Gland Function).
The parasympathetic fibers synapse in the pterygopalatine (sphenopalatine) ganglion located in the pterygopalatine fossa. Postganglionic fibers then travel with branches of the maxillary nerve (cranial nerve V2), specifically via the zygomatic nerve. These fibers pass to the lacrimal nerve, a branch of the ophthalmic nerve (cranial nerve V1), ultimately reaching the lacrimal gland and stimulating tear secretion.
Parasympathetic supply to the salivary glands
Anatomically, the facial nerve carries fibers for both the submandibular and sublingual salivary glands, as well as the lacrimal gland. After passing through the geniculate ganglion, the secretomotor fibers for the salivary glands travel with the main nerve trunk via the chorda tympani, whereas the secretory fibers for the lacrimal gland separate from the facial nerve to join the greater petrosal nerve.
Parasympathetic innervation of the salivary glands originates from the superior and inferior salivatory nuclei in the brainstem and stimulates saliva production. The parotid gland receives parasympathetic fibers from the glossopharyngeal nerve (cranial nerve IX) via the otic ganglion, where preganglionic fibers synapse before postganglionic fibers travel with the auriculotemporal nerve to the gland.[15] The facial nerve innervates the submandibular and sublingual glands through the chorda tympani, which joins the lingual nerve and synapses in the submandibular ganglion.[16] Postganglionic fibers from this ganglion innervate both glands, promoting the secretion of serous and mucous saliva.[17]
Disruptions in this pathway can lead to crocodile tears syndrome. Misdirection or aberrant regeneration of fibers intended for the submandibular and sublingual glands to the lacrimal gland contributes to the development of this condition.
Epidemiology
Bell palsy is a lower motor neuron facial nerve palsy that causes facial muscle weakness of unknown origin. Nemet et al reported an annual incidence of 0.08%, with rates increasing with age, particularly in the 4th to 6th decades of life.[18] A study by Valencia et al found that women were more commonly affected and that the left eye was involved more frequently than the right.[19]
Crocodile tears syndrome is a complication of Bell palsy, occurring in approximately 3.3% of cases. Yamamoto et al reported that symptoms typically develop 6 to 9 months after Bell palsy.[20] The syndrome has also been documented following surgical procedures involving the facial nerve, including acoustic neuroma removal and parotid gland surgery. In these cases, the incidence ranges from 9.5% to 44%, with symptoms emerging within 6 to 12 months postoperatively.
Pathophysiology
During the recovery period following facial nerve injury, damaged salivary nerve fibers may undergo synkinesis or aberrant regeneration, leading to misdirection toward the lacrimal gland instead of normal regrowth toward the submandibular gland. These fibers are redirected via the greater superficial petrosal nerve, causing stimuli such as the smell or taste of food to trigger ipsilateral tearing rather than salivation.[21]
An alternative theory proposed by Spiers et al suggests a congenital abnormality. Supporting this hypothesis, some patients with crocodile tears syndrome have underlying lateral rectus palsy or Duane retraction syndrome, indicating a possible lesion in the pons near the abducens nerve. Another proposed mechanism involves the formation of an artificial synapse at the injury site, allowing impulses to jump between fibers and cause misdirected signaling.[22] Ephaptic transmission, resulting from inadvertent short circuits between nerve fibers, may explain some early-onset cases of crocodile tears syndrome.
History and Physical
Crocodile tears syndrome involves unilateral lacrimation during eating, drinking, or smelling food, though bilateral cases have been reported. The condition is not associated with irritation, photophobia, or pain.
On clinical and slit-lamp examination, the eye and lacrimal structures typically appear normal. Lacrimal syringing confirms the passage of fluid to the nose or mouth, ruling out nasolacrimal duct obstruction (NLDO). Other causes of epiphora, such as punctal stenosis, conjunctivitis, corneal diseases, and conjunctival foreign bodies, should be excluded.
Crocodile tears syndrome is primarily a diagnosis of exclusion in individuals with a history of facial nerve palsy. Patients with prior Bell palsy may report acute-onset symptoms, including neck, mastoid, or ear pain, altered taste or facial sensation, and hyperacusis. Residual facial muscle weakness may be present. In cases of vestibular schwannoma, the corneal reflex may be absent, warranting sensory and motor testing of the trigeminal nerve. Examination of the vestibulocochlear nerve and hearing assessment should also be performed.[23] Signs of healed exposure keratopathy due to previous lagophthalmos may be observed.
Evaluation
Crocodile tears syndrome is a diagnosis of exclusion. Slit-lamp examination of the eye and its appendages is typically performed to rule out other causes of epiphora. Basal tear secretion can be assessed using the Schirmer test, which, in cases of crocodile tears syndrome, may be conducted before and after gustatory stimulation with sweet or sour candy to document increased tearing following salivation. Neuroimaging with magnetic resonance imaging (MRI) may provide insights into the pathogenesis. Facial nerve electrodiagnostic tests, including electroneurography (ENoG) and needle electromyography (EMG), can help evaluate facial nerve function.[24]
Other diagnoses should also be considered. Orbicularis oculi weakness due to facial palsy is assessed by asking the patient to shut their eyes tightly while the examiner attempts to open them. The force required to do so is graded to determine the degree of muscle weakness. Paralytic ectropion is evaluated using the snap-back test, in which the examiner pulls down the lower eyelid and observes whether it immediately returns to its original position. A positive test result indicates lower lid laxity. NLDO is assessed using the regurgitation on pressure over lacrimal sac (ROPLAS) test. Lacrimal syringing is an important tool for confirming or ruling out NLDO.[25]
Treatment / Management
The treatment of crocodile tears syndrome depends on the severity of hyperlacrimation and the patient’s needs. Mild cases are typically managed with counseling and regular monitoring. Lubricating drops may be used to alleviate ocular irritation.
Less invasive approaches are generally preferred. McCoy et al found that subtotal resection of the palpebral lobe of the lacrimal gland was beneficial. Preoperative Schirmer testing helps determine the extent of gland resection necessary to prevent dry eye.
The most widely accepted treatment for crocodile tears syndrome is botulinum toxin injection into the lacrimal gland.[26] Botulinum toxin A is an acetylcholine release inhibitor that acts at the neuromuscular junction, blocking transmission along aberrantly regenerated parasympathetic nerve fibers. This agent may be administered both transcutaneously and transconjunctivally.
The injected dose varies across studies, ranging from 2.5 to 60 units, though 5 to 10 units are typically preferred.[27][28] Higher doses and transcutaneous injections may increase the risk of adverse effects, including ptosis and diplopia. The effects generally last for about 6 months. The transconjunctival approach, targeting the palpebral lobe of the lacrimal gland, has been shown to cause fewer complications than transcutaneous injection. Montoya et al reported that botulinum toxin injection is a safe and effective method for managing excessive tearing in crocodile tears syndrome. This modality has also been used to treat Frey syndrome.[29]
Various treatments have been used historically to reduce lacrimation. A 5% guanethidine eye drop was employed to block adrenergic receptors in the lacrimal gland, while oral propantheline bromide at a dose of 30 mg was also attempted. Additionally, instilling 1% homatropine hydrobromide into the conjunctival sac was believed to block secretomotor nerve activity. However, the side effects of these pharmacological approaches outweighed their therapeutic benefits, and they are no longer considered preferred treatments.
Surgical options for crocodile tears syndrome include excision of the palpebral lobe of the lacrimal gland, chorda tympani nerve sectioning, lacrimal gland denervation through dissection or diathermy, and sphenopalatine ganglion blockade using alcohol or cocaine. Vidian neurectomy has also been attempted. However, these procedures are considered redundant and drastic, with adverse effects that may persist, such as vision loss and total lacrimal gland ablation. Other interventions include intraorbital injections of cocaine or alcohol to destroy postganglionic fibers from the sphenopalatine ganglion and sectioning the facial and glossopharyngeal nerves at multiple levels.
Differential Diagnosis
Crocodile tears syndrome should be considered only after excluding common differential diagnoses, such as simple epiphora following Bell palsy, which results from weakness of the orbicularis oculi. This condition is characterized by sagging of the lower eyelid, which prevents normal tear drainage through the punctum, leading to tear overflow and eye-watering.
Other differential diagnoses include NLDO, conjunctivitis, and allergies. These conditions do not involve hyperlacrimation, and patients typically do not report increased tearing while eating. In crocodile tears syndrome, clinical examination of the eye and its appendages is usually unremarkable. Additionally, a latency of about 6 months between the onset of facial nerve palsy and the development of crocodile tears syndrome is expected, allowing time for nerve regeneration.[30]
Frey syndrome, also known as gustatory sweating or auriculotemporal syndrome, is characterized by sweating and flushing in the preauricular region during eating, typically following parotid gland surgery or trauma. The condition results from aberrant regeneration of postganglionic parasympathetic fibers from the auriculotemporal nerve, errantly innervating sweat glands instead of the parotid gland. The diagnosis is confirmed using the Minor starch-iodine test. Treatment options include botulinum toxin injections, anticholinergic agents, and surgical interventions in severe cases. Although benign, Frey syndrome can cause significant social distress, often necessitating long-term management strategies.[31]
Prognosis
While crocodile tears syndrome is not life-threatening, it can significantly impact an individual's quality of life due to the social and functional distress associated with involuntary tearing. The condition is usually chronic but does not progress over time. Symptoms generally remain stable once aberrant nerve regeneration is complete, typically within 6 to 12 months after injury. The severity of symptoms varies among individuals, with some experiencing mild tearing and others significant lacrimation that interferes with daily activities.
Crocodile tears syndrome following vestibular schwannoma surgery has been reported to improve in approximately 70% of cases, with 50% of patients experiencing complete resolution. Symptoms fluctuate in some cases, and hypotheses explaining recovery include negative feedback mechanisms. Botulinum toxin injections into the lacrimal gland are considered the 1st-line treatment, significantly reducing involuntary tearing and improving quality of life. Response to botulinum toxin is generally favorable, and the Schirmer test may be used to monitor treatment efficacy.
Complications
Involuntary tearing can be socially embarrassing and emotionally distressing, leading to anxiety and reduced social interactions. Excessive tearing may also cause blurred vision and discomfort, affecting daily activities and overall visual function. Botulinum toxin injection, the primary treatment, carries potential complications such as ptosis and hypotropia.[32] A study involving 14 patients with crocodile tears syndrome following vestibular schwannoma surgery found no association between the syndrome and taste abnormalities.
Deterrence and Patient Education
Early intervention following facial nerve palsy or trauma can reduce the risk of aberrant nerve regeneration, a common cause of crocodile tears syndrome. A meticulous technique is essential during surgical procedures involving the parotid gland or facial nerve to minimize neural damage and subsequent miswiring. Comprehensive postoperative care and monitoring allow for early identification of nerve miswiring, facilitating timely intervention.
Patients should be informed that the condition is benign and results from misdirected facial nerve regeneration. Education on symptom management, including the use of artificial tears to reduce discomfort, can improve quality of life. Psychological support and counseling may help patients cope with the syndrome's social and emotional impact. Regular follow-up with healthcare providers ensures ongoing assessment and treatment adjustment as needed.
Enhancing Healthcare Team Outcomes
Since crocodile tears syndrome is rare, early and accurate diagnosis is essential for optimal patient outcomes. In some cases, patients with Bell palsy who experience mild symptoms may choose periodic monitoring rather than active treatment. This concern was demonstrated in the case of a 74-year-old woman in Brazil who had crocodile tears syndrome that was undiagnosed for 9 years.[33]
Increasing awareness among healthcare professionals, including physicians, physician assistants, nurse practitioners, ophthalmologists, neurologists, otorhinolaryngologists, oral and maxillofacial surgeons, and dentists, is necessary to ensure timely recognition and diagnosis. These professionals should also educate patients and their families about the condition. An interprofessional approach to eye disorders can aid in the early detection of other nasolacrimal duct lesions, further improving patient care.[34]