Introduction
The facial nerve is the seventh cranial nerve (CN VII). It arises from the brain stem and extends posteriorly to the abducens nerve and anteriorly to the vestibulocochlear nerve. It courses through the facial canal in the temporal bone and exits through the stylomastoid foramen after which it divides into terminal branches at the posterior edge of the parotid gland. The facial nerve provides motor innervation of facial muscles that are responsible for facial expression, parasympathetic innervation of the glands of the oral cavity and the lacrimal gland, and sensory innervation of the anterior two-thirds of the tongue.
Structure and Function
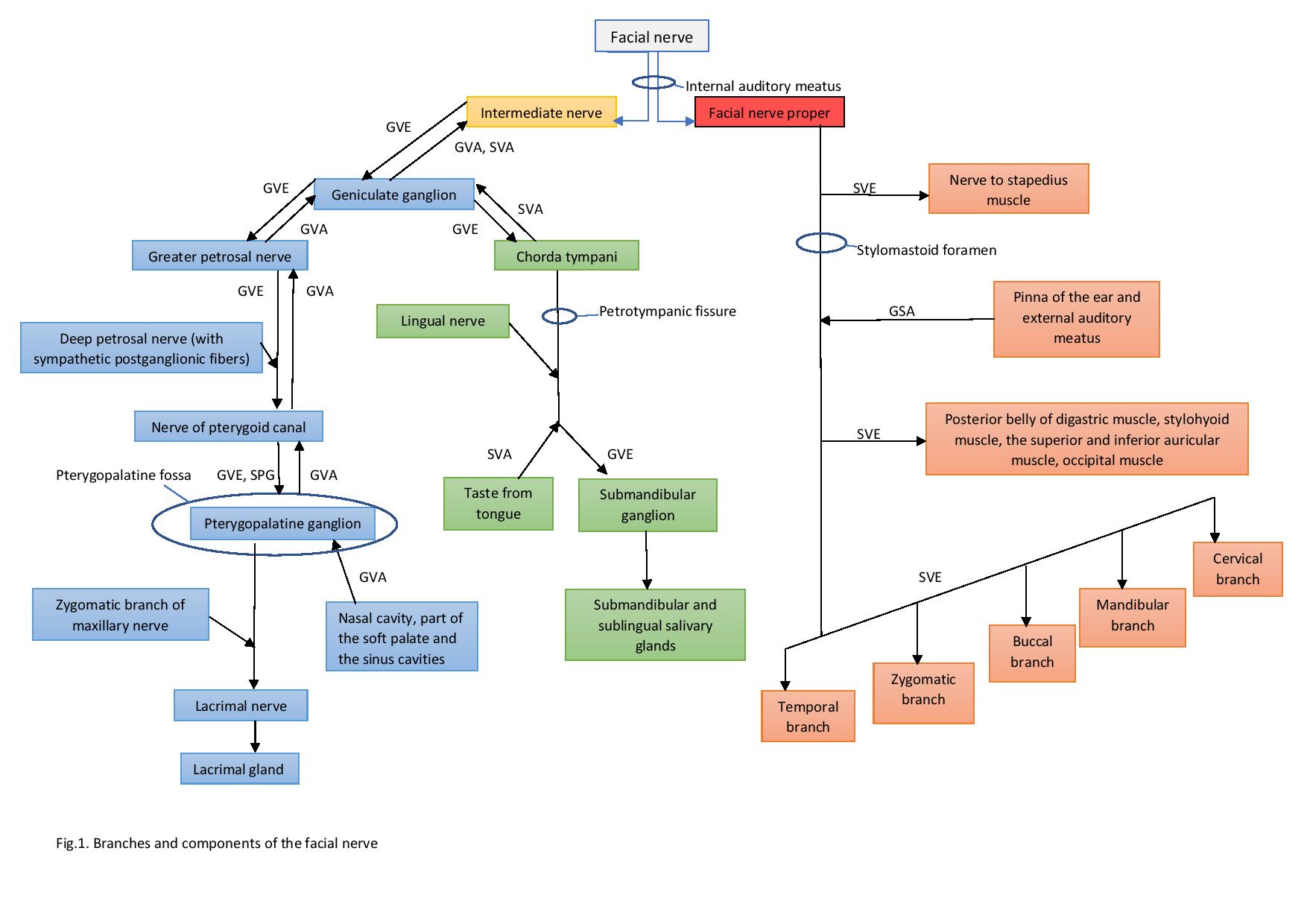
The facial nerve carries both motor and sensory fibers. Motor axons innervate the muscles of facial expression and the stapedius muscle. Parasympathetic fibers go to the ganglia that supply glands in the oral cavity and the lacrimal gland. The sensory component provides innervation to the external auditory meatus, the tympanic membrane, and the pinna of the ear. The facial nerve also carries taste sensation from the anterior two-thirds of the tongue.
Special visceral efferent (SVE) fibers (branchiomotor) are a major component of the facial nerve. Their function is to innervate the muscles of facial expression, the stapedius muscle, the stylohyoid muscle, and the posterior belly of the digastric muscle. The neurons of these fibers are localized in the facial nucleus in the caudal pontine tegmentum.
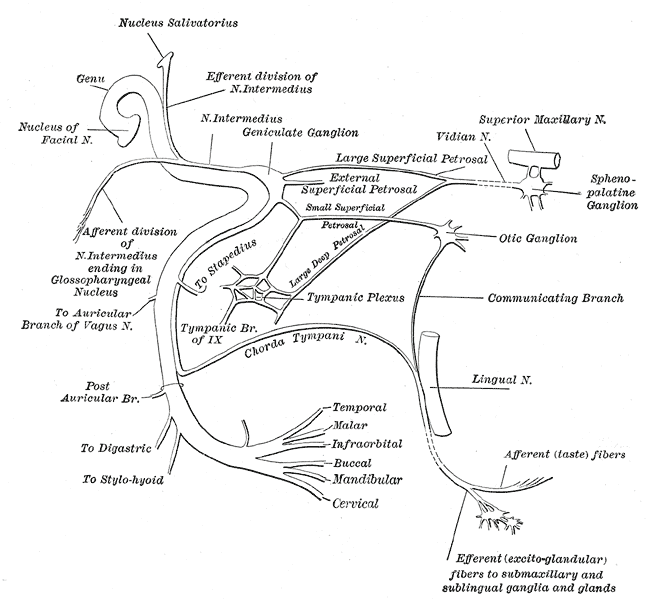
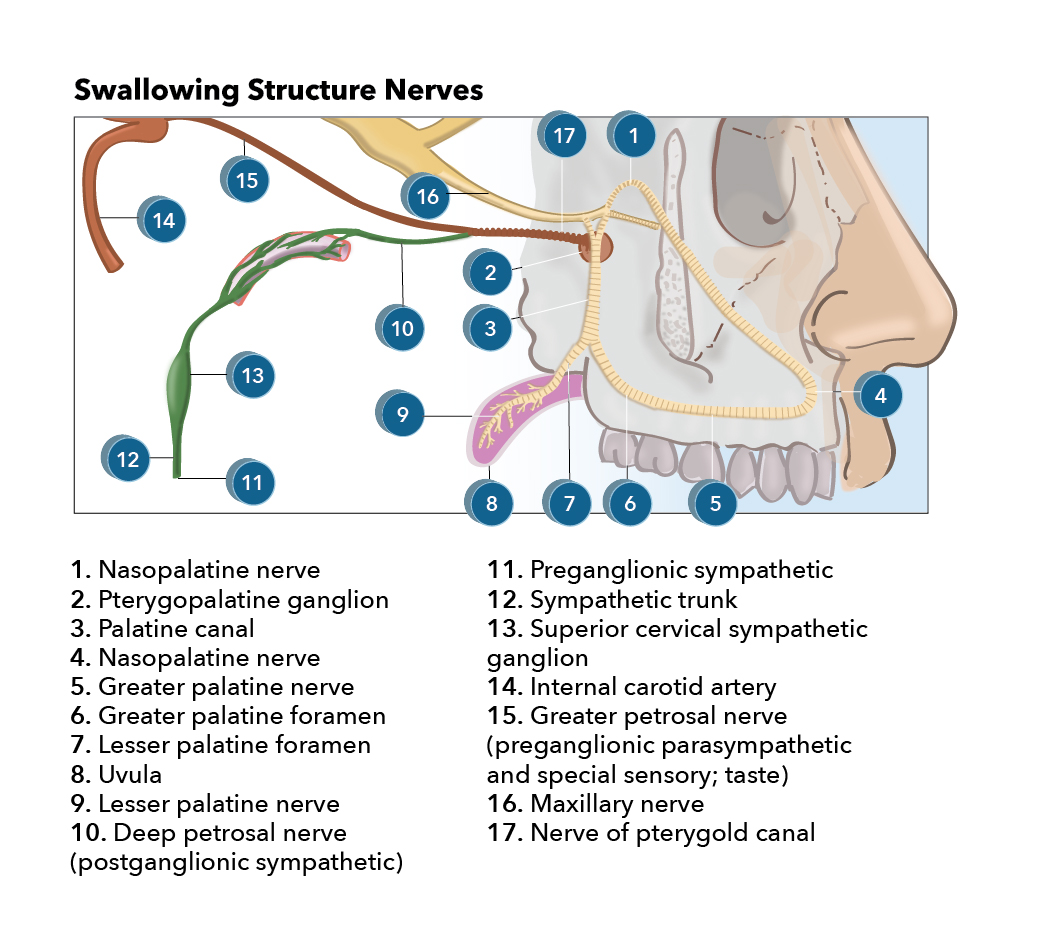
General visceral efferent (GVE) fibers (parasympathetic preganglionic motor fibers) leave the facial nerve as the greater petrosal nerve and the chorda tympani nerve. After synapsing in the pterygopalatine ganglion, the greater petrosal nerve provides postganglionic parasympathetic innervation to nasal, oral, and palatine glands.
The greater petrosal nerve supplies the lacrimal gland by giving branches to the zygomatic branch of the maxillary nerve, which later travels as the lacrimal nerve to the lacrimal gland. These postganglionic fibers cause vasodilation and cause secretion in the lacrimal gland.
The chorda tympani synapses in the submandibular ganglion and later with GVE travels as the lingual nerve, a branch of the mandibular nerve. The lingual nerve reaches the submandibular and sublingual glands where the GVE fibers cause vasodilation and stimulate secretion. GVE preganglionic neurons are located in the superior salivatory nucleus in the brain stem.
The general visceral afferent (GVA) component is very small. The primary sensory neurons are in the geniculate ganglion and gather sensory information via the greater petrosal nerve from the nasal cavity, part of the soft palate, and the sinus cavities. Fibers enter the brain stem with the intermediate nerve and synapse in the nucleus of the solitary tract.
The special visceral afferent (SVA) component (primarily sensory) carries information about taste from the anterior two-thirds of the tongue. Its fibers travel with the lingual nerve and the chorda tympani. The primary neurons are in the geniculate ganglion – at the genu of the facial nerve. The fibers enter the brain via the intermediate nerve and terminate at the ipsilateral nucleus of the solitary tract in the rostral medulla.
The general somatic afferent (GSA) component gathers sensory information from the pinna of the ear and the external acoustic meatus by forming the auricular nerve together with the vagal nerve. Primary sensory neurons are located in the geniculate ganglion. Their central processes enter the brain stem with the intermediate nerve and terminate in the spinal nucleus of cranial nerve V.[1][2][3]
Embryology
The facial nerve is derived from the second branchial arch. The second branchial arch also produces the muscles of the face, the occipitofrontalis muscle, the platysma, the stylohyoid muscle, the posterior belly of the digastric muscle, the stapedius muscle, and the auricular muscles, all of which are innervated by CN VII.[1]
Nerves
The facial nerve exits the brain stem from its ventrolateral surface at the cerebellopontine angle. It consists of two parts: a proper facial nerve and the intermediate nerve. The proper facial nerve contains only a motor component and a very small general somatic afferent component, whereas the intermediate nerve carries sensory and parasympathetic visceromotor components.
The facial nerve anatomy can be divided based on its relation to the cranium and the temporal bone into intracranial, intratemporal, and extratemporal parts.[4]
Intracranial Part
The upper motor neuron (UMN) of the facial nerve is located in the primary motor cortex of the frontal lobe. UMN axons descend ipsilaterally as the corticobulbar tract via the genu of the internal capsule and reach the facial nucleus in the pontine tegmentum. The facial nucleus is divided into a dorsal and ventral region. It contains the cell bodies of the facial nerve lower motor neurons (LMN). The dorsal region supplies innervation of the muscles of the upper face, whereas neurons in the ventral region innervate muscles of the lower face. The dorsal aspect of the facial nucleus receives input from both the left and right cerebral hemispheres. This results in both hemispheres having control over the muscles of the upper face. The ventral aspect of the facial nucleus receives mainly contralateral inputs. As a result, the left hemisphere partially controls the upper left and right side of the face partially and fully the lower right side of the face.
The intermediate nerve carries descending parasympathetic GVE fibers from the superior salivatory nucleus and ascending GVA, GSA, and SVA fibers from the geniculate ganglion.
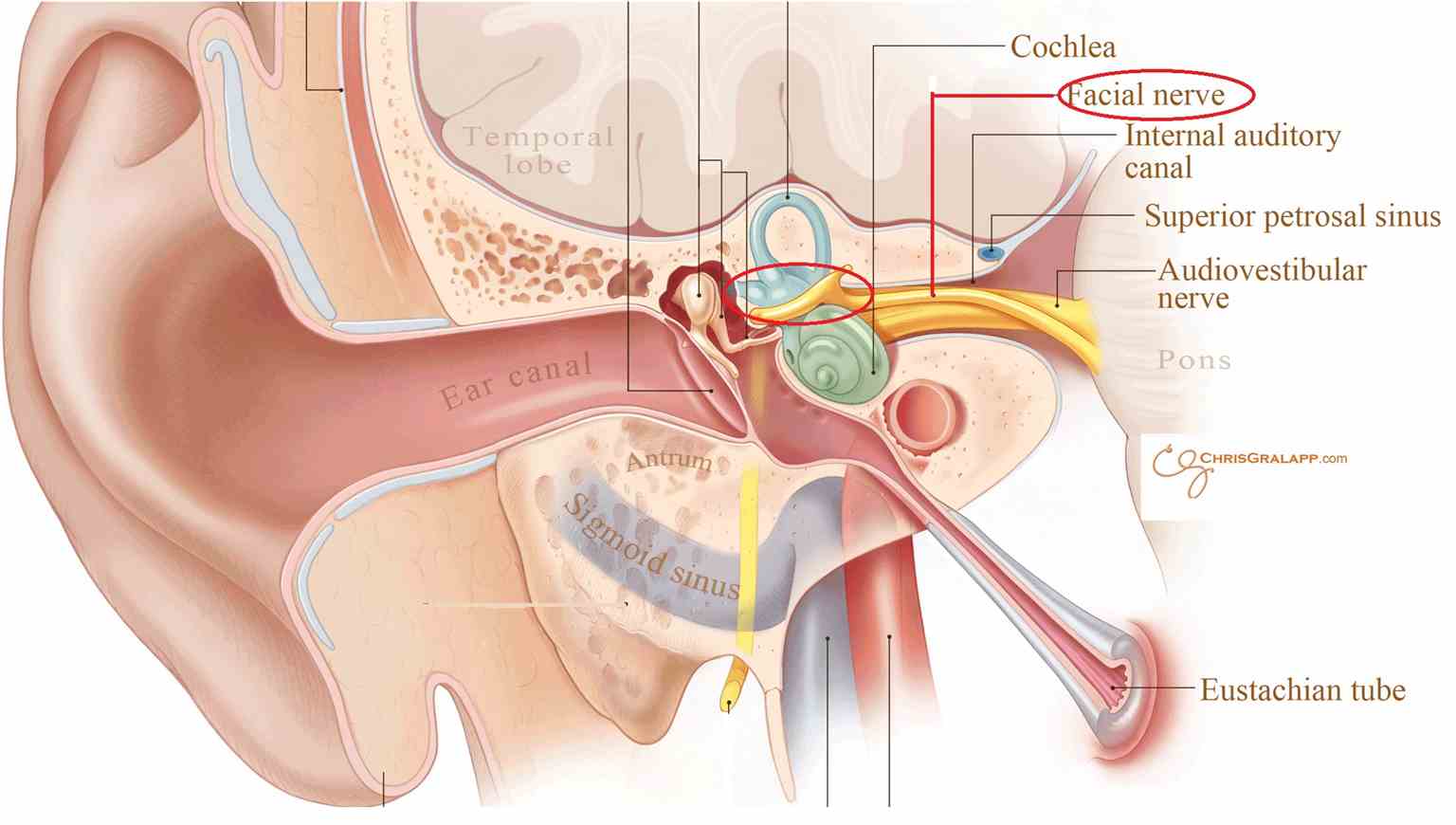
The Intratemporal Part
The intratemporal part of the facial nerve begins when the facial nerve, together with the intermediate nerve, passes through the internal auditory meatus of the temporal bone to enter the facial canal within the petrous part of the temporal bone. After synapsing on the geniculate ganglion, the facial nerve gives rise to the first branch; the greater petrosal nerve, which carries visceromotor parasympathetic fibers (GVE) to the lacrimal gland and GVA from the nasal cavity, paranasal sinuses and part of the soft palate. The greater petrosal nerve joins the deep petrosal nerve which carries sympathetic postganglionic fibers from the superior cervical ganglion. Together they form the nerve of the pterygoid canal that innervates the pterygopalatine ganglion in the pterygopalatine fossa.
The second branch of the facial nerve running in the facial canal is the nerve to stapedius muscle, which provides motor (SVE) innervation to the stapedius muscle of the inner ear.
The chorda tympani nerve is the last branch of the facial nerve within the facial canal and at the same time, the terminal extension of the intermediate nerve. It runs through the ossicles in the middle ear and exits the tympanic cavity at the petrotympanic fissure where it joins the lingual nerve, which is itself a branch of the trigeminal nerve. The chorda tympani nerve carries two kinds of fibers: parasympathetic GVE to the submandibular ganglion and SVA fibers from the anterior two-thirds of the tongue. Fibers from the submandibular ganglion later innervate the submandibular and sublingual glands.[5][6][7][6]
The Extratemporal Part
The extratemporal part of the facial nerve begins when the facial nerve leaves the cranium through the stylomastoid foramen. As the facial nerve exits, it gives GSA fibers to the pinna of the ear and external auditory meatus and SVE fibers to the posterior belly of digastric, stylohyoid, the superior and inferior auricular, and occipitalis muscles. Thereafter, the facial nerve divides at the end of the posterior edge of the parotid gland into the terminal branches. Usually, five branches can be identified:
- The temporal branch – innervating the frontalis and orbicularis oculi muscles and the muscles in the upper part of the face.
- The zygomatic branch – innervating the middle part of the face
- The buccal branch – innervating the cheek muscles, including the buccinator muscle
- The mandibular branch – innervating muscles of the lower part of the face
- The cervical branch – innervating the muscles below the chin and, among others, the platysma muscle[4][1]
Muscles
As stated, the facial nerve innervates the following:
- The muscles of facial expression – responsible for the expression of emotions by changing facial expression
- The stylohyoid muscle – draws the hyoid bone backward, which initiates a swallowing action and elevates the tongue
- The posterior belly of the digastric muscle – together with the anterior belly of the digastric muscle, elevates the hyoid bone and is involved in any complex movements involving the jaw
- The stapedius muscle of the middle ear – stabilizes the stapes, preventing excessive movement in response to loud sounds
Surgical Considerations
The facial nerve is an important cranial nerve and effort should be taken as much as possible to preserve it during surgeries - especially when working around cerebellopontine angle tumors and parotid lesions.
Clinical Significance
Damage to the facial nerve can have various etiologies including iatrogenic, trauma, stroke, idiopathic Bell palsy, neoplasm, or granulomatous meningitis. It is very important not only to recognize the cause of the paralysis but also the side at which the lesion has occurred. The precise neurologic examination allows us to point to the side of the lesion with the greatest likelihood.
Supranuclear Lesion
This occurs as a result of damage to the UMN of the facial nerve. The most common cause of this condition is a lacunar stroke in the posterior limb of the internal capsule. However, UMN lesions can be caused by damage to any part of the corticobulbar tract as it travels from the primary motor cortex in the precentral gyrus of the frontal lobe. From there, the corticobulbar tract descends through the corona radiata and the anterior part of the posterior limb of the internal capsule, and then further in the crus cerebri to the caudal portion of the ventrolateral pontine tegmentum. In the pons, axons of UMN synapse with lower motor neurons in the facial motor nucleus. As was described previously, the supranuclear innervation is bilateral to the muscles of the upper part of the face and contralateral to the muscles of the middle and lower part of the face. UMN lesion results in paralysis of the contralateral middle and lower parts of the face with sparing of the muscles of the forehead and the orbicularis oculi muscle.[2]
Nuclear or Infranuclear Lesion
Lesions that involve the facial motor nucleus or the infranuclear portion of the facial nerve result in complete paralysis of all the facial muscles on the ipsilateral side. The patient presents with mouth droop, flattening of the nasolabial fold, inability to close eye, and smoothing of the brow on the damaged side.
The precise anatomic location of the lesion can be evaluated by the characteristics of the dysfunctions and involvement of associated structures:
- PonsLesion of ventral pons: ipsilateral facial plegia, palsy of lateral rectus muscle (abducens nerve), contralateral hemiplegia (corticospinal fibers)Lesion of pontine tegmentum: ipsilateral facial plegia, contralateral hemiplegia, paralysis of conjugate gaze to the side of the lesion (pontine paramedian reticular formation)
- Cerebellopontine angleIpsilateral facial plegia, decreased secretion of saliva and tears, hyperacusis, and loss of taste (ageusia) in anterior two-thirds of the ipsilateral part of the tongue. In addition, other cranial nerves can be damaged. If the vestibulocochlear nerve is involved, further findings can present as deafness, vertigo, tinnitus; the trigeminal nerve – ipsilateral sensory loss over face and absence of corneal reflex
- Facial canal between the internal acoustic meatus and the geniculate ganglionIpsilateral facial plegia, decreased secretion of saliva and tears, hyperacusis and ageusia to anterior two-thirds of the ipsilateral part of the tongue
- Facial canal between geniculate ganglion and nerve to the stapedius muscleIpsilateral facial plegia, decreased salivary secretion, ageusia to anterior two-thirds of the ipsilateral part of the tongue, hyperacusis.
- Facial canal between nerve to stapedius and leaving of chorda tympaniIpsilateral facial plegia, decreased salivary secretion, ageusia to anterior two-thirds of the ipsilateral part of the tongue
- After giving the branch of chorda tympaniIpsilateral facial plegia[8]
Bell Palsy
Bell palsy is an idiopathic form of facial nerve palsy. One theory is that it is caused by edema because of a viral infection. Bell palsy can be distinguished from other causes of facial paralysis by rapid onset over several hours and lack of trauma. What is more, this kind of facial paralysis is very often self-limiting, and the patient usually recovers within days to weeks. Residual symptoms can include facial weakness, synkinesis, tearing, and contracture. Patients can benefit from early initiation of steroids as this prevents the progression of edema, diminishes chances of further damage, and speeds recovery. There is no established evidence for the use of antiviral agents. Eye patching and artificial tears protect from corneal scarring.[9][10][9]
Other Issues
Reflexes
The facial motor nucleus receives afferent information from several origins and participates in a number of reflexes:
The corneal reflex is tested by stimulating the cornea with a wisp of cotton. It results in the reflex closure of both eyelids. The afferent limb of this reflex is mediated by the trigeminal nerve, and the efferent limb is mediated by the facial nerve.
Orbicularis oculi reflex can be evoked by various stimuli such as stimulation of the supraorbital nerve, light, and sound. The afferent limb of this reflex is mediated by the trigeminal, optic, and vestibulocochlear nerves respectively. The efferent limb is mediated by the facial nerve and produces bilateral eye blink.
Orbicularis oris reflex, also known as snout reflex, is produced by percussion on the upper lip or the side of the nose and results in ipsilateral elevation of the angle of the mouth. The trigeminal nerve stands for the afferent limb and the facial nerve for the efferent limb of the reflex. Orbicularis oris reflex can be evoked in infants and disappears later in life. It can recur in the setting of the supranuclear facial nerve lesion and extrapyramidal diseases like Parkinson disease.[8]