Continuing Education Activity
Approximately 3 percent of all visits to the emergency department are due to eye trauma, with the vast majority of these presentations involving corneal injury. The morbidity from corneal injuries can vary greatly, from minor and insignificant to potentially vision-threatening. Injuries to the cornea can broadly be categorized into traumatic and exposure-related. Traumatic injuries most commonly include corneal abrasions and foreign bodies. Exposure-related injuries to the cornea include burns from chemical, thermal, and radiation sources. Ocular chemical burns are an emergency, accounting for 11.5%–22.1% of all ocular injuries. This activity examines when a corneal injury should be considered and how to properly evaluate it, and also highlights the role of the inter-professional team in caring for patients with all forms of corneal injury.
Objectives:
- Outline the etiology and pathophysiology of the major types of corneal injury.
- Describe the patient presentation of types of corneal injuries, differential diagnosis, and proper examination procedure for evaluation.
- Summarize the treatment and management of corneal injury based on specific etiology.
- Explain the importance of improving care coordination amongst the interprofessional team to enhance the delivery of care for patients with corneal injuries.
Introduction
Approximately 3% of all visits to the emergency department are due to eye trauma, with the vast majority of these presentations involving corneal injury. The morbidity from corneal injuries can vary greatly, from minor and insignificant to potentially vision-threatening. Injuries to the cornea can broadly be categorized into traumatic and exposure-related. Traumatic injuries most commonly include corneal abrasions and foreign bodies. Exposure-related injuries to the cornea include burns from chemical, thermal, and radiation sources.[1][2][3][4][5] More severe corneal injuries include penetrating trauma with or without the involvement of the anterior and posterior segment structures, ocular surface burns leading to limbal stem cell deficiency, and secondary glaucoma. This review focus on the major types of corneal injury, their assessment, acute management, and long-term sequelae.
Etiology
Corneal Abrasion and Foreign Body
Corneal abrasions may be caused by any number of objects including fingernails, contact lens wear, plant branches, and foreign objects blown or thrown into the eyes. Lack of eye protection can result in high-speed projectile objects penetrating the cornea resulting in more serious damage.
Corneal Perforation
Corneal laceration and perforation can be accidental, however more often involve activities that cause high-speed projectiles such as saws, angle grinders, and pounding metal objects, with or without eye protection. It is important to elicit from the history the type of object i.e. wood or metal and estimated projectile speed.
Ocular Burns
Exposure-related burns of the eye can be categorized into chemical (acid and alkali burns), radiation burns from ultraviolet (UV) sources, and thermal burns. Alkali corneal injuries are more common than acid due to the prevalence of household cleaning agents containing ammonia and lye. Acidic burns are typically work-related injuries involving industrial processes, but can also be intentional assault.[6] Radiation burns result in ultraviolet keratitis from tanning beds, high-altitude environments, welding arcs, and the occasional solar eclipse. Thermal burns are distinctly uncommon but can occur with objects such as curling irons and with fire-related injuries.
Epidemiology
Eye trauma accounts for about 3% of all emergency department visits, with approximately 80% of these visits for corneal abrasions or foreign bodies.[7][8] The incidence of corneal abrasion is higher among people of working age, with automotive workers between the ages of 20 and 29 years having the highest incidence of eye injuries.[9]
Ocular chemical burns are an emergency, accounting for 11.5%–22.1% of all ocular injuries.[10] Haring et al found that young children in the U.S. were the highest-risk individual group for ocular chemical burns, with ages 1 to 2 years at greatest risk.[11] Generally, ocular chemical injuries occurred in individuals aged 18 to 64 years of age, making up the second most common cause of workplace ocular injuries after foreign bodies in the eye.[12][13] Unfortunately in recent years assault and hate crimes have contributed to an increased incidence of chemical injury, including up to 33% of severe ocular burns injuries. [14][15][6]
Pathophysiology
Corneal Injury
Fragile and easily damaged, the corneal epithelium is richly innervated, and therefore, very painful when an injury occurs. The epithelium does regenerate quickly, with most abrasions healing within 24 to 48 hours.[16] For chemical eye injuries, the extent of damage depends on the substance in question. For alcohol-related injuries, the de-epithelisation of the ocular surface will usually heal with no further sequelae. Acids will cause tissue proteins to bind to acid molecules which then neutralizes the acid, causing coagulation and tissue necrosis. Theoretically, this will act as a barrier to further acid penetration and limit the damage.[16][16] Alkali ocular injuries are more numerous and cause hydrophilic and lipophilic degeneration. The fatty acids of cellular membranes undergo saponification upon contact with alkalis, leading to rapid penetration into the cells. The tissues are more susceptible to enzymatic degradation and damage.[16]
Corneal Healing
Corneal healing is via cellular migration, proliferation, and differentiation, with extracellular matrix remodeling. The corneal epithelium regenerates via limbal stem cells and remodeling of the basement membrane. The response of healing to a corneal abrasion is dependent on the defect size and depth. Cellular proliferation and migration are necessary to heal larger abrasions. Limbal stem cells migrate and differentiate to cover the defect with a single layer of epithelial cells, which "slide" over the wound. Proliferation from the basal layer restores the normal thickness of the epithelium and the formation of normal adhesions can take up to 6 weeks.[16] Recurrent corneal erosions can occur long-term if this process is incomplete. Deeper injuries involving the corneal stroma require the transformation of keratocytes to fibroblasts and myofibroblasts, which can lead to opacification and scarring.
History and Physical
The patient is most likely to complain of pain or foreign body sensation for small corneal abrasions, and presentation can be delayed for several hours after the inciting event. For acute ocular chemical injuries symptoms are likely to be immediate. Healthcare practitioners should ask about the work environment and specifically, the use of high-speed machinery and metalworking, as these injuries are can be associated with corneal laceration and perforation of the globe. A history of eye pain that occurs after hammering metal on metal suggests a metal projectile as the cause of the ocular injury, and the possibility of globe rupture should be thoroughly investigated in this setting. For ocular burns, it is important to identify the chemical(s) the eye was exposed to, as this can impact treatment and prognosis. It is also important to ask if there was any ingestion or inhalation of chemical substances, as respiratory passage edema can lead to asphyxiation.
Evaluation
Corneal Abrasion and Laceration/Perforation
Conjunctival erythema, lid swelling, tearing, and blepharospasm can be seen upon eye inspection. The corneal defect can often be visualised under magnification even without the use of fluorescein. With severe pain, treatment with a topical anesthetic may be needed to obtain a complete physical exam. Relief of pain with the application of a topical anaesthetic such as proparacaine strongly suggests a superficial (corneal) etiology of ocular pain. Visual acuity should be considered the vital sign of the eye and be determined in every patient with an ocular complaint. Acuity should be assessed while the patient is wearing any corrective lenses should they have them and is typically normal in the setting of corneal abrasions unless there is associated iritis or corneal defect in the central visual axis. Instillation of fluorescein and examination with a cobalt blue light will demonstrate the corneal abrasion as a bright green, superficial defect of the cornea.[17][18][19][20]
Corneal Foreign Bodies
Similar to corneal abrasions, patients usually complain of pain with foreign body sensation, tearing, and blepharospasm. Application of a topical anesthetic improves physical examination and diagnosis may be aided by the use of a slit lamp. Ocular foreign bodies may lodge under the upper eyelid and cause repeated abrasions to the cornea whenever the patient blinks. The resulting corneal injury can have the appearance of numerous linear or curvilinear abrasions of the cornea. The upper eyelid should, therefore, be everted and examined for foreign bodies when a corneal or conjunctival foreign body is suspected. In the setting of a metallic foreign body, a rust ring will generally form in the surrounding cornea within several hours.
Corneal Laceration/Perforation
Signs that suggest a full-thickness corneal laceration or perforation include a misshapen iris, hyphema, microhyphema, decreased visual acuity, and a shallow anterior chamber. Aqueous humor leaking from the anterior chamber during fluorescein examination suggests a corneal perforation (Seidel’s test). Although, for small lacerations, it is possible for the Seidel test to be negative with grossly normal-appearing ocular anatomy. The entire thickness of the cornea should be evaluated with a slit lamp. A high index of suspicion for globe penetration should be maintained and a CT of the orbit should be obtained when the history or physical examination suggests the possibility of such an injury. While fairly accurate, CT is an imperfect diagnostic test; ophthalmology consultation is recommended for situations where there is a very high index of suspicion even when the orbital CT is unremarkable.
Ocular Burns
Chemical burns to the eye are an ocular emergency with scarring and permanent loss of vision and the eye being a possibility. Irrigation of the eyes and removal of any chemical substances must be done immediately, before any evaluation or examination, including testing of vision. Once completed, the visual acuity and intraocular pressure measurement should be documented. It is also important to ascertain whether the patient has inhaled or ingested any chemical substance, in order to assess for any respiratory compromise. Patients with radiation burns and photokeratitis are typically in severe pain and discomfort. In addition to decreased visual acuity, tearing, and chemosis of the conjunctiva, instillation of fluorescein reveals a characteristic superficial punctate staining of the cornea. Grading systems can be used to assess ocular ischemic damage and visual prognosis.[21]
Treatment / Management
Corneal Abrasions
The majority of corneal abrasions heal spontaneously, so treatment consists primarily of pain control and preventing infection. For abrasions greater than 2 mm, or for those that are very painful, a cycloplegic agent such as cyclopentolate 1% or homatropine 5% can help control discomfort by relaxing the ciliary body and relieving pain from spasm. The cycloplegia of both these agents lasts approximately 24 hours, so a single administration at the time of care should be adequate given the rapidity of corneal healing. Topical anesthetics should never be prescribed for home use as they can inhibit corneal healing, impair the protective blinking reflex, and prolong identification of the progression of the ocular pathology or development of complications.
In cases not related to contact lens wear, erythromycin ophthalmic ointment is a suitable antibiotic, but for contact lens wearers antipseudomonal coverage is needed. A fluoroquinolone such as ciprofloxacin or ofloxacin will provide adequate antibiotic prophylaxis. Tetanus prophylaxis should be administered if necessary. Patients should be counseled to not wear contacts until the abrasion has healed completely. Patients with corneal abrasions should be reevaluated within 24 to 48 hours to assure complete resolution of the injury.
Corneal Foreign Bodies
Corneal foreign bodies should be removed at the time of diagnosis, preferably under slit lamp magnification, after anesthesia has been achieved with a topical agent such as proparacaine 0.5%. A cotton applicator may occasionally be effective in removing a foreign body but a sterile needle or eye spud may be necessary.[22] Residual rust ring removal can be performed similarly or be deferred for removal by an ophthalmologist the following day. Scarring can occur with rust removal so care should be exercised with rust in the central visual axis and consideration given to referral to an ophthalmologist for removal. If there is any possibility that the foreign body penetrated the entire length of the cornea, the injury should be treated as a globe perforation as described above. Following removal of the foreign body, the treatment of the remaining corneal defect should be as described above in the discussion of corneal abrasion management.
Corneal Laceration/Perforation
Unrecognized corneal perforations can quickly result in endophthalmitis or traumatic cataract. These should be treated similarly to scleral (globe) rupture with the placement of a protective eye shield to prevent accidental pressure on the globe and broad-spectrum intravenous antibiotics to cover common organisms that cause post-traumatic endophthalmitis. A third-generation cephalosporin, gentamycin, and vancomycin would be appropriate.
Ocular Burns
Treatment of radiation burns (ultraviolet keratitis) is supportive of pain control and topical antibiotics, although there is minimal evidence for the latter. Oral opioids are typically needed. Generally a self-limiting condition, ophthalmology follow up in 24 hours is needed if symptoms have not resolved. Patients should be counseled on the adverse effects of ultraviolet radiation including cataract formation, pterygium, and skin cancer.
Treatment of ocular chemical burns should begin at the scene of the injury with copious irrigation with water for at least thirty minutes and continue upon arrival to the hospital. The use of irrigation devices, such as a Morgan Lens, is helpful in delivering continuous irrigation to the affected eye. The conjunctival fornices should be checked for any particulate matter, and irrigation should continue until the pH of the conjunctivae is 7 in both eyes. If available, buffered eyewash solutions may be better for the irrigation of caustic exposures than standard normal saline. After irrigation of one to two liters, the pH should be tested with fresh litmus paper. Irrigation should be continued until the pH remains neutral for at least 30 minutes after the last irrigation. Ophthalmology consultation should be obtained for all but minor burns. Any patient with corneal clouding or an epithelial defect should be promptly referred to an ophthalmologist. The principles of acute management include removal of inciting chemical agents, promotion of ocular surface epithelial healing (ascorbate, citrate), inflammation control (topical steroids, citrate, and acetylcysteine), and infection prevention (topical antibiotics), pain control (cycloplegia, systemic oral analgesia). A prompt and frequent review is necessary to assess clinical progress and detect complications e.g. raised intraocular pressure.
Differential Diagnosis
- Acute angle-closure glaucoma
- Acute conjunctivitis (pink eye)
- Epidemic Keratoconjunctivitis
- Map-dot fingerprint dystrophy
Treatment Planning
After the initial acute management of corneal injury, more intermediate and long-term care is necessary for severe cases such as chemical burns. Management of these cases focuses on 3 areas: encouraging re-epithelisation, treating symptomatic limbal stem cell deficiency, and diagnosing and managing secondary glaucoma.
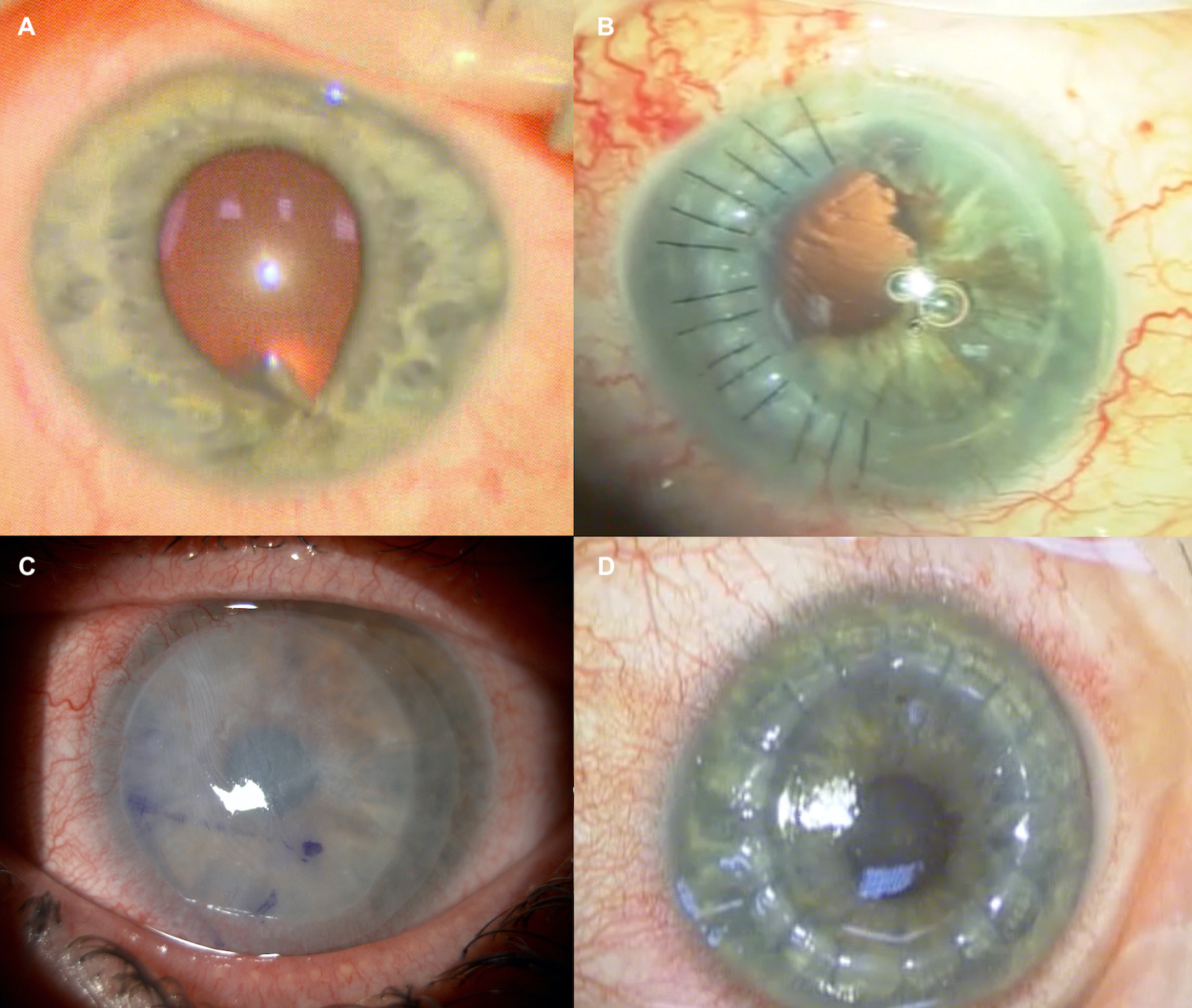
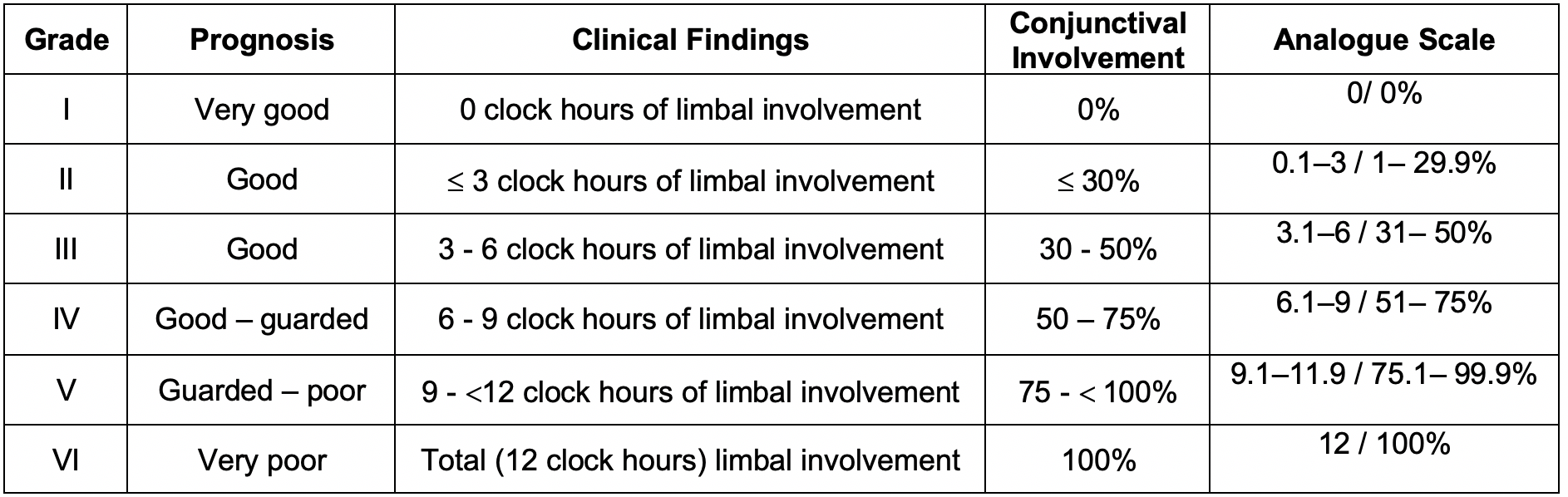
Staging
Staging of ocular surface burns is helpful for clinical assessment and visual prognosis. The Dua classification is commonly used (see attached image).[21] The analogue scale refers to the limbal involvement in clock hours of limbus and percentage of conjunctivae affected conjunctivae. Bulbar conjunctivae including the fornices are included in the percentage score.
Prognosis
Superficial cornea abrasions or foreign body injuries have a very good prognosis, especially if the visual axis is not involved. For anterior stromal scarring affecting the visual axis, excimer laser correction, or partial corneal transplantation are options for long-term visual rehabilitation. Greater than 50% conjunctival or >6 clocks hours of limbal involvement result in poor visual prognosis in ocular chemical burns.
Complications
Complications of corneal injury include scarring affecting the visual axis, recurrent corneal erosion due to weak adhesions between the healed corneal epithelium and underlying corneal layers, reduced limbal stem cell function and failure, secondary glaucoma due to trabecular meshwork damage, traumatic cataract, retinal detachment, and loss of vision or the eye.[23][24]
Deterrence and Patient Education
Significant numbers of corneal injuries are related to activities at home or work, by a body part, sports equipment, or work tools. Eye protection can be easily obtained but is commonly omitted. A proportion of severe ocular chemical burns are assault-related. Delayed presentations and poor compliance with treatment and follow-up reviews can adversely affect final visual outcomes. Targeted patient education and public health awareness can potentially aid in improving treatment outcomes in this group of patients.
Enhancing Healthcare Team Outcomes
The management of corneal injuries is with an interprofessional team that includes an ophthalmic nurse, emergency department physician, an ophthalmologist.[25] As soon as a corneal injury is suspected in the emergency room, an ophthalmology consult should be made. These patients need to be managed ASAP to preserve vision. The outcomes depend on the type and severity of the corneal injury. Most small abrasions heal without sequelae. Tiny corneal foreign bodies also have a good outcome. However, the prognosis after ocular burns and corneal perforations is guarded. Many of these patients may require prolonged care and some may even have a visual loss after adequate treatment.[26][27] (Level V)