Continuing Education Activity
Registry study places the incidence of C2 fracture at 6 per 100000 people. In Sweden, of 6370 patients with C2 fractures: 51% were male, and the average age was 72 years. Those who were younger, male, and presenting with spinal cord injury were more likely to undergo surgical intervention. In the pediatric cohort, C1 to C2 injuries represented 7.7% of spine fractures presenting through a multi-institutional series following after trauma from multiple blunt mechanisms. This activity reviews the etiology, presentation, evaluation, and management of C2 vertebral fractures and reviews the interprofessional team's role in evaluating, diagnosing, and managing the condition.
Objectives:
- Describe the unique vertebral anatomy of the second cervical vertebra (axis).
- Outline the components of evaluation/assessment for a patient presenting with a potential second cervical vertebra fracture, including any indicated imaging studies.
- Summarize the management options available for second cervical vertebra fractures, based on the specific fracture type.
- Identify interprofessional team strategies for improving communication to advance medical care and improve outcomes for various types of C2 vertebral fractures.
Introduction
Registry study places the incidence of C2 fracture at 6 per 100,000 people. Of 6370 patients with C2 fractures in Sweden, 51% were male, and the average age was 72 years. Those who were younger, male, and presenting with spinal cord injury were more likely to undergo surgical intervention. In the pediatric cohort, C1 to C2 injuries represented 7.7% of spine fractures presenting through a multi-institutional series following after trauma from multiple blunt mechanisms.[1][2][3][4]
Etiology
Blunt trauma is the leading mechanism. Falls, motor vehicle accidents, assault, and other traumatic presentations usually cause blunt trauma. It is important to recognize that in the elderly cohort, low-energy cervical blunt trauma can create unstable high cervical spine fractures.[3][5][6]
Epidemiology
The incidence of C2 fractures increased 135% from 2000 to 2011 in the Medicare population. C2 fractures are associated with a 20% and 40% increased risk of mortality within 3 months and 2 years, respectively. The majority of C2 fracture types are type-II dens fractures. This is troublesome because these have a pseudoarthrosis (non-union) rate that exceeds 50%.
Pathophysiology
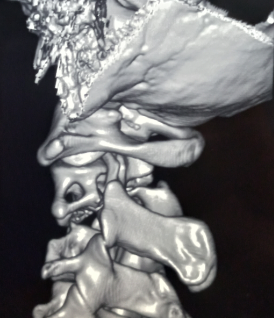
It is critical to appreciate the unique anatomy of the C2 vertebra. The dens extend superiorly to communicate with C1 via the ligamentous anatomy. Lack of intervertebral discs, unique ligamentous attachments, vertebra anatomy, and vertebral artery vasculature makes this area biomechanically unique from the subaxial cervical spine. For example, C1-C2 is generally responsible for 50% of the rotation movement.[3]
C2 fractures can be divided into 2 kinds: odontoid and hangman's.
Odontoid Fractures
Location
- Fracture through the dens, flexion, or extension injury
Nomenclature
Anderson and D’Alonzo classification is the most ubiquitous.
- Type-1 fractures: Upper portion of the odontoid peg, above the transverse portion of the cruciform ligament, these are generally stable
- Type-2 fractures: These are the most common; they fracture through the based of the odontoid below the transverse portion of the cruciform ligament, they have a high risk of non-union
- Type-3 fractures: These fracture through the odontoid peg and into the body of C2, generally well tolerated
The Roy-Camille classification of odontoid fractures is another but less frequently used nomenclature format focusing on the direction of the fracture line.
Hangman’s Fractures
Location
- Fracture is generally through the bilateral pars, usually from hyperextension and axial loading
- Stable 90% heal with immobilization alone
Nomenclature
Levine and Edwards Classification
- Type 1: Less than 3 mm subluxation of C2 on C3, due to axial loading, stable, rigid cervical collar treatment
- Type 2: disruption of the C2 to C3 disc, posterior longitudinal ligament, greater than 4 mm subluxation, greater than 11 degrees angulation, less than 5 mm requires a reduction in axial traction and halo fixation for 6 to 12 weeks while those with greater than 5 mm can require surgery
- Type 2a: Less displacement more angular deformity, flexion injury, unstable, not suitable for axial traction; treatment in halo
- Type 3: C2 to C3 facet capsule disrupted, anterior longitudinal ligament disruption, unstable, may have a deficit; surgical candidates
History and Physical
It is important to recognize that low-energy, blunt trauma can induce significant unstable injury, especially in the elderly population. History should also entertain fracture risk factors such as osteoporosis, metastatic burden, or vitamin D deficiencies. Physical exam findings include pain with palpation in the posterior portion of the neck, radiculopathy, myelopathy, and possible posterior fossa findings secondary to vertebral artery injury. A strict neurologic exam including cranial nerves, sensory, motor, and rectal tone is mandatory.
Evaluation
Laboratory tests should be ordered as an adjunct in overall medical status. Normalized hemoglobin, hematocrit, coagulation profile with prothrombin time (PT), partial thromboplastin time (PTT), and platelet counts will be needed for operative intervention.
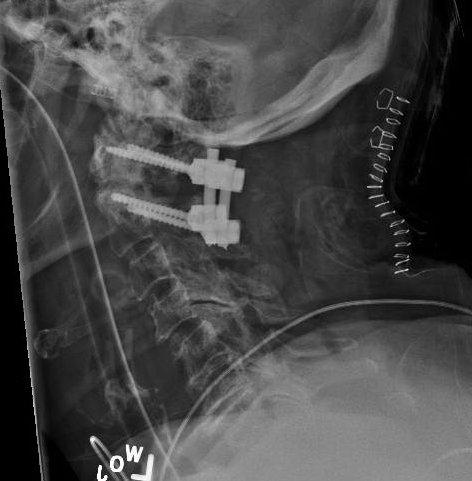
X-ray
Evaluation of x-rays will provide limited but important information. Care must be taken to ensure proper radiographic imaging creates a picture from the occiput to the C7 through T1 disc space. This is essential in reviewing cervical spine trauma. Lateral, anteroposterior (AP), and open mouth odontoid views are necessary. Approximately 93% of cervical spine injuries are apparent with combined, lateral, AP, and odontoid view radiographs. X-rays are an excellent modality for determining alignment during the immediate injury, post-operative period, as well as long-term follow-up.
Computed Tomogram (CT) Scan
CT scan is the most important modality for determining fracture etiology and ruling out an injury regarding a C2 fracture. Even if plain films are negative and clinical suspicion is high, a CT scan is warranted. CT scan does not directly evaluate the spinal cord, soft tissue, or ligamentous construct. It is important to recognize the importance that complete imaging will require dedicated thin-cut CT reconstructions. Non-contrast CT scan is adequate for evaluation of the bony anatomy for fracture. This can be coupled with a CT angiogram (see below) for evaluation of the vascular anatomy.
Magnetic Resonance imaging (MRI) Scan
Evaluation with MRI is important for analyzing the ligamentous construct, disc space, spinal cord, nerve roots, and other soft tissue injuries. MRI is also useful for determining the acute nature of the fracture when this is otherwise unknown. This is done via non-contrasted imaging. T2 signal hyperintensities and STIR changes within the dens, ligaments, or soft tissue can illustrate an acute component. MRI is less dangerous than flexion-extension cervical injury. Furthermore, MRI evaluation is mandatory in evaluating the transverse ligament for the surgical decision matrix of non-displaced type II odontoid fractures. An intact transverse ligament is needed for the anterior placement of an odontoid screw.
Vascular Imaging
Vascular imaging may be indicated. The vertebral artery’s second segment (V2) runs through the transverse foramen of C2 to C6, while V3 runs extradurally, exiting the C2 foramen across the sulcus arteriosus. This can place it at risk for injury. Indeed, in one series, 15% of patients with C1 to C2 fractures had a vertebral artery injury. Of which, type-III odontoid fractures posed the greatest risk. It is important to note that an untreated vertebral artery injury has a 24% stroke rate. CT angiography can be coupled to CT imaging upon fracture evaluation with consideration of kidney function. Level-III evidence suggests that patients with C1 to C3 fractures can be screened with multi-slice multi-detector CT angiography. At this time, MR angiography cannot be listed as the sole imaging modality for the evaluation of vertebral artery injury. The first-line investigation with percutaneous angiography is overly aggressive.
Treatment / Management
Treatment options include conservative management, cervical orthosis, halo-vest orthosis, and surgical procedures.[7][8][9][10]
External Fixation
A rigid cervical collar represents the immediate first treatment. For type-I and type-III odontoid fractures, this is generally adequate. This is also true for 90% of hangman’s fractures. Halo-vest orthosis can be used as well for external fixation in certain cases of type-II odontoid fractures or angulated/displaced Hangman’s fractures but is not very well tolerated in the elderly population.
Internal Fixation
Internal fixation can be achieved via anterior fixation or by a variety of posterior constructs.
Anterior
An odontoid screw can be placed for type-II odontoid fractures in good alignment with an intact transverse ligament in the acute setting. There is concern about the placement of the odontoid screw in the elderly population and instances of delayed non-union.
Posterior
- C1 to C2 transarticular screws
- C1 lateral mass and C2 pedicle screws
- C1 lateral mass and C2 pars interarticularis screws
- C1 to C2 wiring (also as an adjunct technique)
Posterior fixation technique selection requires significant review by a neurosurgeon or orthopedic spine surgeon. It takes into consideration a variety of factors, including surgeon experience, fracture location, vertebral artery location, biomechanical suitability, and anatomical variations. Vascular imaging is mandatory to illustrate the location of the vertebral artery in the V2 and V3 segments. The patient’s overall functional status, medical optimization, and bone health must be evaluated in the operative decision-making. This includes consideration for type-II odontoid fractures.
Differential Diagnosis
- Os odontoideum
- Mach effect
- Persistent ossiculum terminale
- Pseudosubluxation (generally C2 to C3)
Prognosis
Generally, C2 fracture treatment is quite successful. A retrospective study comparing posterior cervical fusion with either C2 pedicle or C2 translaminar screws found that breach of pedicle screws occurred more frequently. The same study determined that the 1-year durability of translaminar screws is inferior to pedicle screws for subaxial fusions but equally effective for axial fusions.[11] Early management of cervical spine injuries is recommended to improve clinical outcomes.[12]
Complications
Complications of a C2 fracture treatment include nonunion, malunion, and pseudoarthrosis formation. This risk is higher in those treated with the conservative approach. In patients treated with conservative therapy after initial therapy who present with nonunion, surgical correction is warranted.
Other complications of this disease are inherent with any surgical procedure, such as infection, especially osteomyelitis. Other complications include hardware failure and neurovascular injury.
In patients undergoing an anterior surgical approach, there is a risk of airway compromise that may lead to prolonged endotracheal intubation.
Deterrence and Patient Education
Patient education on compliance with therapy, especially those planned for conservative treatment, is essential. Patients also need to be educated on the importance of clinical and radiologic follow-up to ensure adverse outcomes do not occur.
Pearls and Other Issues
- A rigid cervical collar should be immediately placed in the emergency room setting.
- It is important to recognize that high cervical spine fractures requiring surgical instrumentation can be complex operative interventions.
- Complete and proper imaging is a must.
Enhancing Healthcare Team Outcomes
Upper cervical spine fractures are not uncommon and are usually associated with other injuries as well. These fractures are best managed by an interprofessional team that includes a trauma surgeon, orthopedic surgeon, neurosurgeon, emergency department physician, radiologist, and a neurologist. The treatment options include conservative management, cervical orthosis, halo-vest orthosis, and surgical procedures. Neurosurgery nurses usually monitor the patients in an ICU setting. Rehabilitation may include physical therapy. The outlook depends on the presence of a neurological deficit on presentation, patient age, other associated injuries, and head trauma. Isolated high cervical spine injuries that are not displaced have a good prognosis.[13][14]