[1]
Mitchell L, King M, Brillhart H, Goldstein A. Cervical Ectropion May Be a Cause of Desquamative Inflammatory Vaginitis. Sexual medicine. 2017 Sep:5(3):e212-e214. doi: 10.1016/j.esxm.2017.03.001. Epub 2017 Apr 28
[PubMed PMID: 28460993]
[2]
Chang AR. 'Erosion' of the uterine cervix; an anachronism. The Australian & New Zealand journal of obstetrics & gynaecology. 1991 Nov:31(4):358-62
[PubMed PMID: 1799353]
[3]
Goldacre MJ, Loudon N, Watt B, Grant G, Loudon JD, McPherson K, Vessey MP. Epidemiology and clinical significance of cervical erosion in women attending a family planning clinic. British medical journal. 1978 Mar 25:1(6115):748-50
[PubMed PMID: 630328]
[4]
Wright KO,Mohammed AS,Salisu-Olatunji O,Kuyinu YA, Cervical Ectropion and Intra-Uterine Contraceptive Device (IUCD): a five-year retrospective study of family planning clients of a tertiary health institution in Lagos Nigeria. BMC research notes. 2014 Dec 23;
[PubMed PMID: 25539789]
Level 2 (mid-level) evidence
[5]
Madile BM. The Cervical Epithelium From Fetal Age to Adolescence. Obstetrics and gynecology. 1976 May:47(5):536-9
[PubMed PMID: 1264400]
[6]
Jacobson DL, Peralta L, Graham NM, Zenilman J. Histologic development of cervical ectopy: relationship to reproductive hormones. Sexually transmitted diseases. 2000 May:27(5):252-8
[PubMed PMID: 10821596]
[7]
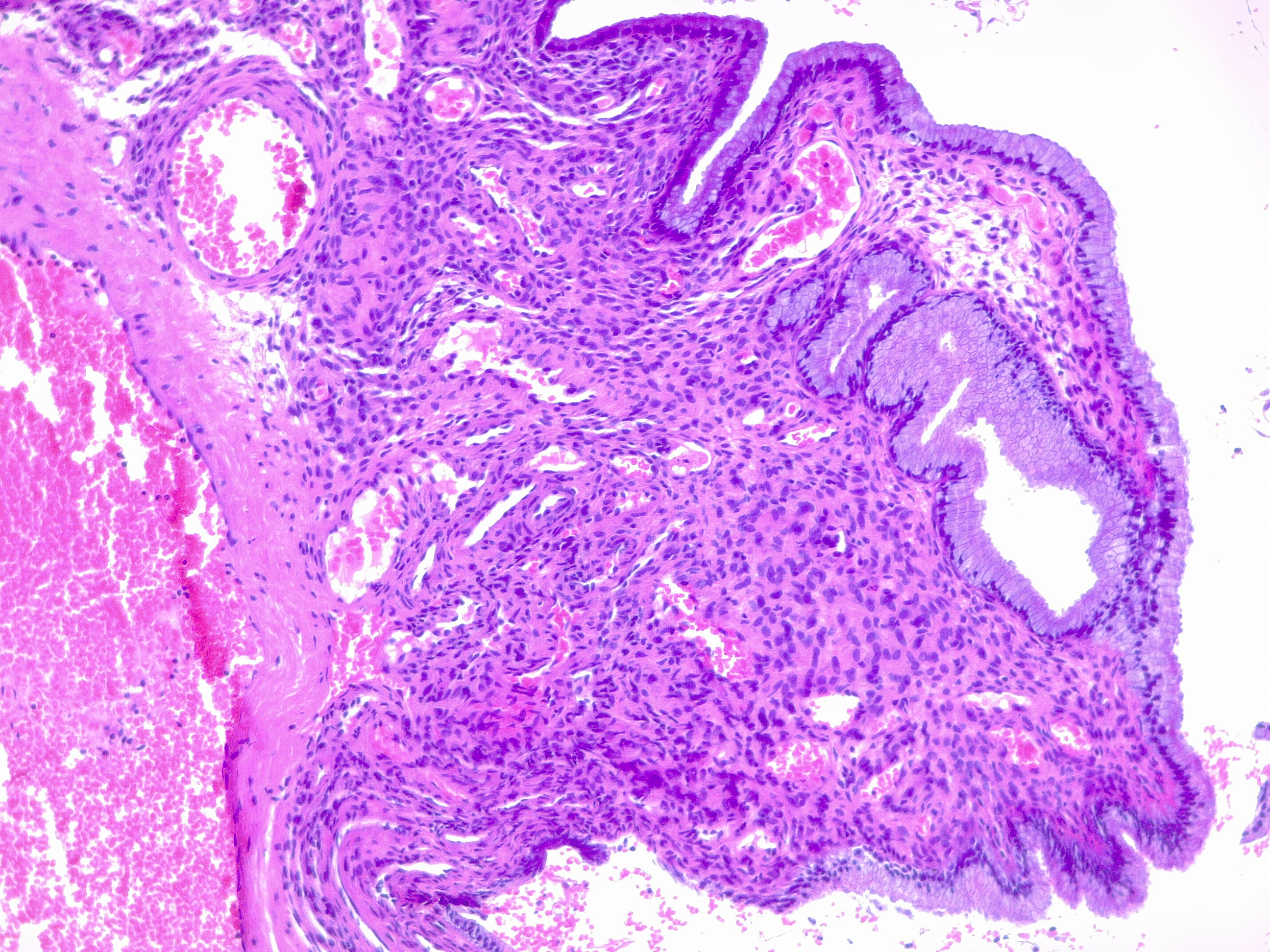
Reich O, Regauer S, McCluggage WG, Bergeron C, Redman C. Defining the Cervical Transformation Zone and Squamocolumnar Junction: Can We Reach a Common Colposcopic and Histologic Definition? International journal of gynecological pathology : official journal of the International Society of Gynecological Pathologists. 2017 Nov:36(6):517-522. doi: 10.1097/PGP.0000000000000381. Epub
[PubMed PMID: 28639968]
Level 2 (mid-level) evidence
[8]
Autier P, Coibion M, Huet F, Grivegnee AR. Transformation zone location and intraepithelial neoplasia of the cervix uteri. British journal of cancer. 1996 Aug:74(3):488-90
[PubMed PMID: 8695371]
[9]
Maqueo M, Azuela JC, Calderon JJ, Goldzieher JW. Morphology of the cervix in women treated with synthetic progestins. American journal of obstetrics and gynecology. 1966 Dec 1:96(7):994-8
[PubMed PMID: 4162849]
[10]
Ostergard DR. The effect of pregnancy on the cervical squamocolumnar junction in patients with abnormal cervical cytology. American journal of obstetrics and gynecology. 1979 Aug 1:134(7):759-60
[PubMed PMID: 463976]
[11]
Lee V, Tobin JM, Foley E. Relationship of cervical ectopy to chlamydia infection in young women. The journal of family planning and reproductive health care. 2006 Apr:32(2):104-6
[PubMed PMID: 16824301]
[12]
De Luca Brunori I, Facchini V, Filippeschi M, Battini L, Giusti G, Romani L, Scida P, Urbano M. Cell-mediated immunity in the course of cervical ectropion. Clinical and experimental obstetrics & gynecology. 1994:21(2):105-7
[PubMed PMID: 7915218]
[13]
Morrison CS, Bright P, Wong EL, Kwok C, Yacobson I, Gaydos CA, Tucker HT, Blumenthal PD. Hormonal contraceptive use, cervical ectopy, and the acquisition of cervical infections. Sexually transmitted diseases. 2004 Sep:31(9):561-7
[PubMed PMID: 15480119]
[14]
Venkatesh KK, Cu-Uvin S. Assessing the relationship between cervical ectopy and HIV susceptibility: implications for HIV prevention in women. American journal of reproductive immunology (New York, N.Y. : 1989). 2013 Feb:69 Suppl 1():68-73. doi: 10.1111/aji.12029. Epub 2012 Oct 11
[PubMed PMID: 23057756]
[15]
Monroy OL, Aguilar C, Lizano M, Cruz-Talonia F, Cruz RM, Rocha-Zavaleta L. Prevalence of human papillomavirus genotypes, and mucosal IgA anti-viral responses in women with cervical ectopy. Journal of clinical virology : the official publication of the Pan American Society for Clinical Virology. 2010 Jan:47(1):43-8. doi: 10.1016/j.jcv.2009.10.008. Epub 2009 Nov 10
[PubMed PMID: 19906557]
[16]
Kleppa E, Holmen SD, Lillebø K, Kjetland EF, Gundersen SG, Taylor M, Moodley P, Onsrud M. Cervical ectopy: associations with sexually transmitted infections and HIV. A cross-sectional study of high school students in rural South Africa. Sexually transmitted infections. 2015 Mar:91(2):124-9. doi: 10.1136/sextrans-2014-051674. Epub 2014 Oct 3
[PubMed PMID: 25281761]
Level 2 (mid-level) evidence
[17]
Junior JE, Giraldo PC, Gonçalves AK, do Amaral RL, Linhares IM. Uterine cervical ectopy during reproductive age: cytological and microbiological findings. Diagnostic cytopathology. 2014 May:42(5):401-4. doi: 10.1002/dc.23053. Epub 2013 Oct 25
[PubMed PMID: 24166971]
[18]
Casey PM, Long ME, Marnach ML. Abnormal cervical appearance: what to do, when to worry? Mayo Clinic proceedings. 2011 Feb:86(2):147-50; quiz 151. doi: 10.4065/mcp.2010.0512. Epub 2011 Jan 26
[PubMed PMID: 21270291]
Level 3 (low-level) evidence
[19]
Joshi SN, Das S, Thakar M, Sahasrabuddhe V, Kumar BK, Callahan M, Mauck C. Colposcopically observed vascular changes in the cervix in relation to the hormonal levels and menstrual cycle. Journal of lower genital tract disease. 2008 Oct:12(4):293-9. doi: 10.1097/LGT.0b013e31817efbbd. Epub
[PubMed PMID: 18820544]
[20]
Selo-Ojeme DO, Dayoub N, Patel A, Metha M. A clinico-pathological study of postcoital bleeding. Archives of gynecology and obstetrics. 2004 Jul:270(1):34-6
[PubMed PMID: 15224216]
[21]
Critchlow CW, Wölner-Hanssen P, Eschenbach DA, Kiviat NB, Koutsky LA, Stevens CE, Holmes KK. Determinants of cervical ectopia and of cervicitis: age, oral contraception, specific cervical infection, smoking, and douching. American journal of obstetrics and gynecology. 1995 Aug:173(2):534-43
[PubMed PMID: 7645632]
[22]
Stillo A, Bianco V, Lorenzin MG, Franzosi N. [Colposcopic evaluation of cervical epithelium during oral contraception. A controlled clinical study]. Annali di ostetricia, ginecologia, medicina perinatale. 1989 Nov-Dec:110(6):296-304
[PubMed PMID: 2700878]
[23]
Slimani O, Ben Temim R, Makhlouf T, Mathlouthi N, Attia L. Cyto-colpo-histologic correlation: about an analytical study of 120 colposcopies. La Tunisie medicale. 2016 Oct:94(10):616-620
[PubMed PMID: 28972254]
[24]
Gay C, Riehl C, Ramanah R, Desmoulin G, Violaine B. [Cryotherapy in the management of symptomatic cervical ectopy]. Gynecologie, obstetrique & fertilite. 2006 Mar:34(3):214-23
[PubMed PMID: 16530444]
[25]
Çekmez Y, Şanlıkan F, Göçmen A, Vural A, Türkmen SB. Is Cryotherapy Friend or Foe for Symptomatic Cervical Ectopy? Medical principles and practice : international journal of the Kuwait University, Health Science Centre. 2016:25(1):8-11. doi: 10.1159/000441433. Epub 2015 Oct 27
[PubMed PMID: 26436550]
[26]
Baram A, Paz GF, Peyser MR, Schachter A, Homonnai ZT. Treatment of cervical ectropion by cryosurgery: effect on cervical mucus characteristics. Fertility and sterility. 1985 Jan:43(1):86-9
[PubMed PMID: 3838091]
[27]
Agah J,Sharifzadeh M,Hosseinzadeh A, Cryotherapy as a Method for Relieving Symptoms of Cervical Ectopy: A Randomized Clinical Trial. Oman medical journal. 2019 Jul;
[PubMed PMID: 31360321]
Level 1 (high-level) evidence
[28]
Yang K, Li J, Liu Y, Ma B, Roberts H, Tan J, Tian J, Wu T, Zhang P. Microwave therapy for cervical ectropion. The Cochrane database of systematic reviews. 2007 Oct 17:2007(4):CD006227
[PubMed PMID: 17943899]
Level 1 (high-level) evidence
[29]
De Luca Brunori I, Urbano M, Romani L, Tarani A, Felipetto R, Battini L, Amato A, Andreoni P. [Clinico-morphological changes in ectropion after treatment with polydeoxyribonucleotide (PDRN)]. Annali di ostetricia, ginecologia, medicina perinatale. 1990 Nov-Dec:111(6):379-87
[PubMed PMID: 2102065]
[30]
de Luca Brunori I, Battini L, Filippeschi M, Romani L, Tarani A, Urbano M. [Topical therapy with placental polydeoxyribonucleotide in cervical ectopy and ectropion]. Annali di ostetricia, ginecologia, medicina perinatale. 1989 Jan-Feb:110(1):35-41
[PubMed PMID: 2757327]
[31]
Hua X, Zeng Y, Zhang R, Wang H, Diao J, Zhang P. Using platelet-rich plasma for the treatment of symptomatic cervical ectopy. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2012 Oct:119(1):26-9. doi: 10.1016/j.ijgo.2012.05.029. Epub 2012 Jul 24
[PubMed PMID: 22835570]
[32]
Dawood AS, Salem HA. Current clinical applications of platelet-rich plasma in various gynecological disorders: An appraisal of theory and practice. Clinical and experimental reproductive medicine. 2018 Jun:45(2):67-74. doi: 10.5653/cerm.2018.45.2.67. Epub 2018 Jun 29
[PubMed PMID: 29984206]
Level 2 (mid-level) evidence
[33]
Chen J, Zhou D, Liu Y, Peng J, Li C, Chen W, Wang Z. A comparison between ultrasound therapy and laser therapy for symptomatic cervical ectopy. Ultrasound in medicine & biology. 2008 Nov:34(11):1770-4. doi: 10.1016/j.ultrasmedbio.2008.03.013. Epub 2008 May 9
[PubMed PMID: 18471953]
[34]
Li C, Xiong X, Li Y, Li J, Peng B, Wang Z, Chen W. Therapeutic effects of focused ultrasound in 4014 patients with symptomatic cervical ectopy. Ultrasound in medicine & biology. 2013 Apr:39(4):604-10. doi: 10.1016/j.ultrasmedbio.2012.11.012. Epub
[PubMed PMID: 23497842]
[35]
Cotarcea S,Stefanescu C,Adam G,Voicu C,Cara M,Comanescu A,Cernea N,Pană R, The Importance of Ultrasound Monitoring of the Normal and Lesional Cervical Ectropion Treatment. Current health sciences journal. 2016 Apr-Jun;
[PubMed PMID: 30568831]
[36]
Mitchell H. Vaginal discharge--causes, diagnosis, and treatment. BMJ (Clinical research ed.). 2004 May 29:328(7451):1306-8
[PubMed PMID: 15166070]
[37]
Mattson SK, Polk JP, Nyirjesy P. Chronic Cervicitis: Presenting Features and Response to Therapy. Journal of lower genital tract disease. 2016 Jul:20(3):e30-3. doi: 10.1097/LGT.0000000000000225. Epub
[PubMed PMID: 27243142]
[38]
Machado Junior LC, Dalmaso AS, Carvalho HB. Evidence for benefits from treating cervical ectopy: literature review. Sao Paulo medical journal = Revista paulista de medicina. 2008 Mar 6:126(2):132-9
[PubMed PMID: 18553039]
[39]
Hwang LY, Ma Y, Shiboski SC, Farhat S, Jonte J, Moscicki AB. Active squamous metaplasia of the cervical epithelium is associated with subsequent acquisition of human papillomavirus 16 infection among healthy young women. The Journal of infectious diseases. 2012 Aug 15:206(4):504-11. doi: 10.1093/infdis/jis398. Epub 2012 Jun 13
[PubMed PMID: 22696500]