Continuing Education Activity
The velum interpositum (VI) is a membrane resulting from the superposition of two layers of the tela choroidea of the third ventricle, demarcating a potential space containing cerebrospinal fluid (CSF) located in the region between the internal cerebral veins (ICV) and the posterior medial choroidal artery. The dilatation of this space is “cavum veli interpositi” (CVI). This activity describes the anatomical characteristics of the cavum veli interpositi and highlights its role in human pathology. The part the interprofessional team plays in the care of these patients will be reviewed.
Objectives:
Identify the etiology of cavum veli interpositi and the medical conditions associated.
Interpret the evaluation of cavum veli interpositi.
Apply the management options available for the complication of cavum veli interpositi.
Communicate some interprofessional team strategies for improving care coordination and communication to advance and improve outcomes in this kind of disease associated with the presence of this anatomical variant.
Introduction
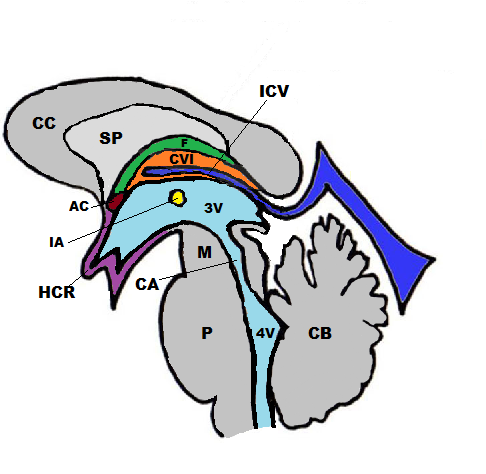
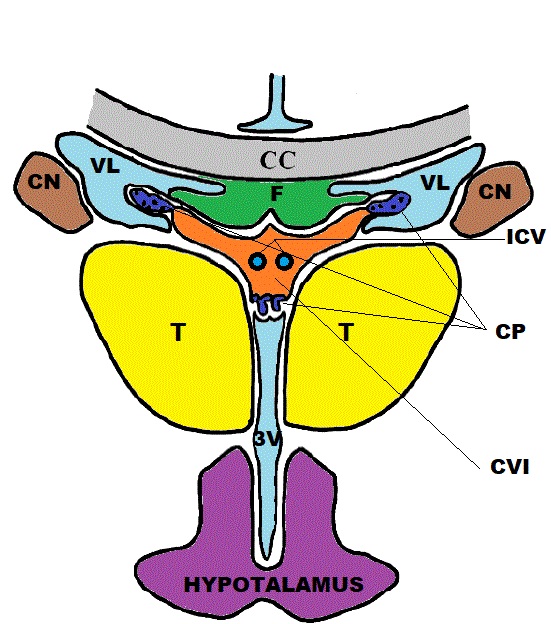
The velum interpositum (VI) is a membrane resulting from the superposition of 2 layers of the tela choroidea of the third ventricle demarcating a potential space containing cerebrospinal fluid (CSF) located in the region between the internal cerebral veins (ICV) and the posterior medial choroidal artery (see Images. Sagittal Schematic View, Cavum Veli Interpositi and Coronal Schematic View, Cavum Veli Interpositi).
Kruse, in 1930, defined the dilatation of this space as “cavum veli interpositi” (CVI). Other names frequently used to describe this structure are “ventriculi tertii, “cisterna interventricularis,” “transverse fissure,” and “sub-trigonal fissure.” CVI has a triangular shape, with a wide base dorsally and an apex pointing anteriorly. It reaches as far forward as the foramen of Monroe.
Boundaries
- Superiorly: the fornix and the hippocampal commissure,
- Inferiorly: the tela choroidea of the third ventricle and the internal cerebral veins,
- Laterally: the thalami,
- Anteriorly: the roof of the third ventricle and the interventricular foramina;
- Posteriorly: the splenium of the corpus callosum and the habenular commissure.
Etiology
CVI is part of the group of "cystic persistent primitive structures" of brain midline as the absence of septum pellucidum(ASP), the cavum septi pellucidi (CSP), and the cavum vergae (CV). See Image. Cavum Septum Pellucidum. These cystic structures are present during the brain's developmental process in the embryonic period, and they regress between the seventh month of intrauterine life and the second year of postnatal life. They are normal findings during fetal life but persist in a certain proportion of adults.[1]
These cerebral cavities do not have ependymal coverage, and they do not have a lining of choroid plexus cells. They are in direct communication with the subarachnoid space, and the ventricular system separates them, so they cannot be considered part of the ventricular system.[2] CVI is an anatomic variation originating from a protrusion of the pia mater into the primitive neural tube during the third fetal month.[3]
Epidemiology
CVI is considered a structure normally present in the fetal brain. It decreases in size after full-term birth and is an uncommon variant in adults.
The persistence in children between the ages of 1 and 10 is around 30%. Cheng found an incidence of CVI of about 21% at the ultrasonography of children born preterm, while a CT study based on the analysis of 442 adults showed an incidence of 7.24% for CVI.[2][4]
CVI was present in 5.54% of a population of 505 neurosurgical patients between 2 months and 79 years old. No statistically significant difference existed in the frequency of CVI between the genders and age groups. CVI is considered to be twice as frequent as the cavum vergae.[5]
Pathophysiology
Cavum veli interpositi does not usually cause symptoms, and it is a common incidental finding in brain MRI. Symptoms occur rarely, and they primarily relate to the ball-valve mechanism between the cisterna CVI and the cisterna venae magnae Galeni with transient increased intracranial pressure.
Histopathology
CVI is a potential space containing cerebrospinal fluid formed between the 2 layers of the tela choroidea of the third ventricle. The tela choroidea comprises a dual-layer loose connective tissue of the pia mater surmounted by the ependyma. A very rich arterial and venous vascularization characterizes the tela choroidea.
History and Physical
Although several pieces of evidence have accumulated, the role of cavum veli interpositi in brain pathology is still uncertain. The existence of a syndrome characterized by moderate ventricular dilation without intracranial hypertension and progressive increase in head size has been hypothesized in association with the presence of CVI.[6] Some studies supposed a relationship between the presence of dilated CVI in children and the presence of hydrocephalus, seizures, and mental retardation.[6][7]
Tubbs and colleagues (J Pediatr Neurol. 2004; 2: 107-110) studied a couple of identical twins with midline cerebral cysts, increased head size, and mild ventricular enlargement. They suggested that the midline cysts can lead to microcephaly and mild ventricular enlargement through recurrent episodes of raised intracranial pressure. A ball-valve mechanism between the cisterna CVI and the cisterna venae magnae Galeni explained the intermittency of symptoms.
Evaluation
CVI is generally an occasional common finding during routine MRI or CT scans performed for other conditions. It is also usually visible during newborn transcranial ultrasound.
Treatment / Management
The treatment of the small cysts of cavum veli interpositi is mainly based on their collapse. Shunting or endoscopic ventricular fenestration are valid alternatives for treating the large cysts of CVI when they become symptomatic because it creates a communication between the midline cavity filled with CSF and the νentricular system. The ventriculoperitoneal shunting creates communication between the cystic cavity and the ventricular system.[8]
Differential Diagnosis
The cyst of cavum veli interpositi must be distinguished mainly from other midline intracranial cysts. The key to the differential diagnosis is an accurate anatomical evaluation of these structures:
- Cavum septi pellucidi (CSP): cavum with the same triangular shape but with posterior apex pointing. CSP is anterior to the foramen of Monro, between the frontal horns of the lateral ventricles.
- Cavum vergae: cavum with a rectangular shape in cross-section. It is superior to the columns of the fornices, which are displaced inferiorly.
- Pineal cyst: a common, usually asymptomatic, and incidental finding for CVI. The pineal cyst is located below the internal cerebral veins abutting the colliculi.
- Arachnoid cyst: an arachnoid cyst of the region of the quadrigeminal cistern can mimic a CVI. It is usually eccentric, located below the cerebral veins, and not triangular in cross-section.
Prognosis
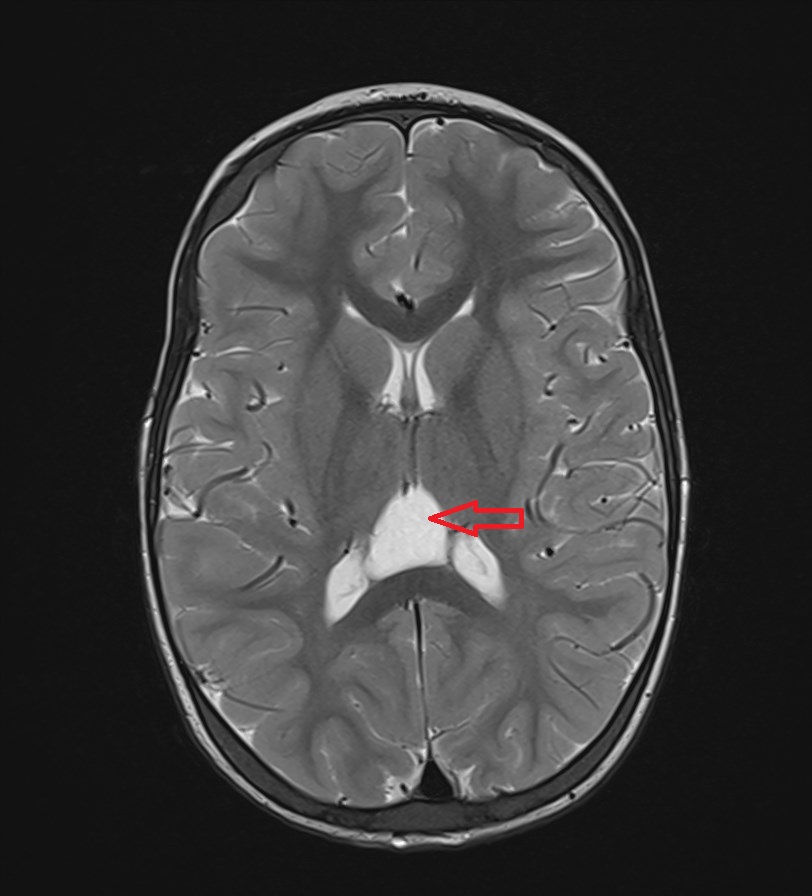
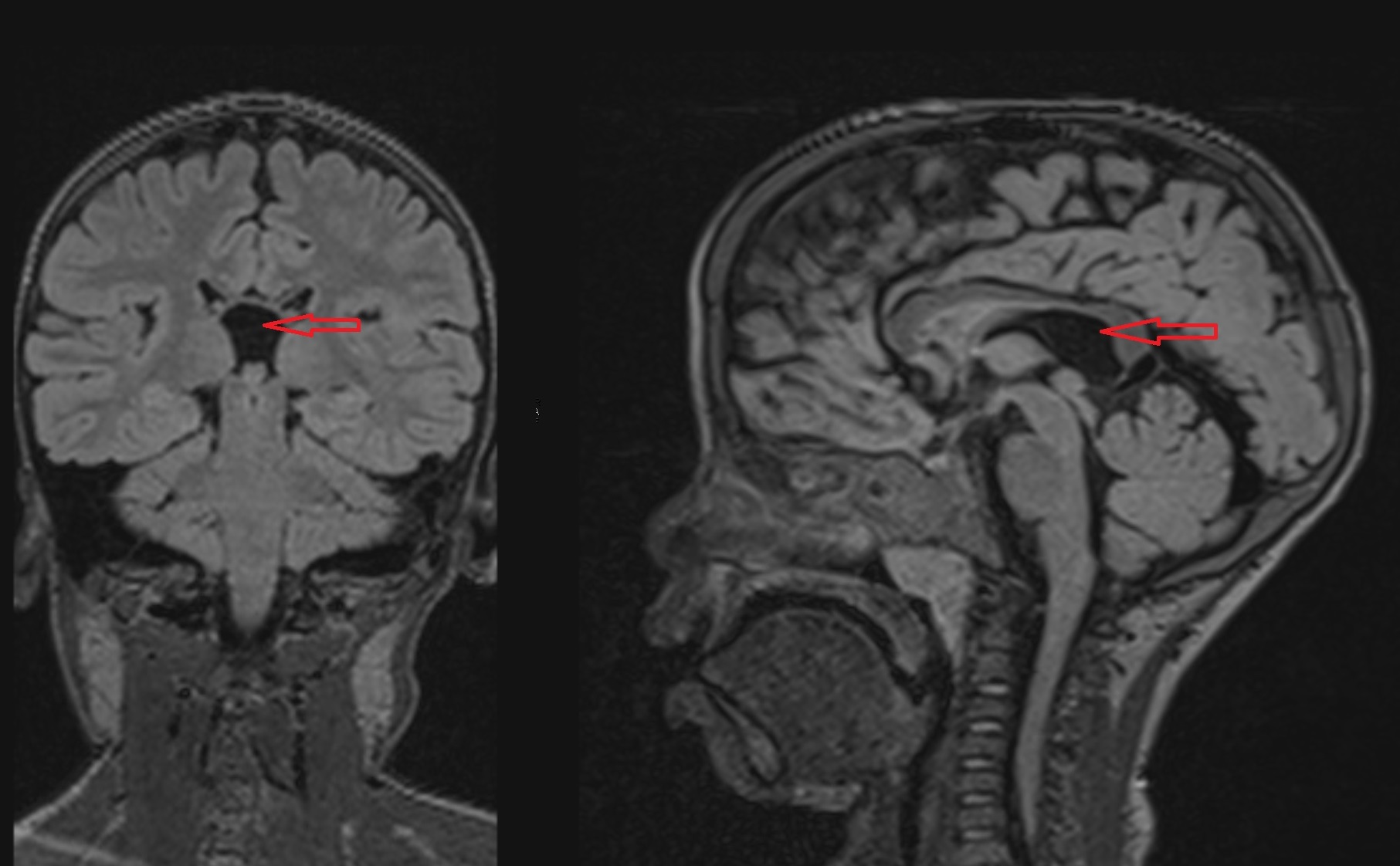
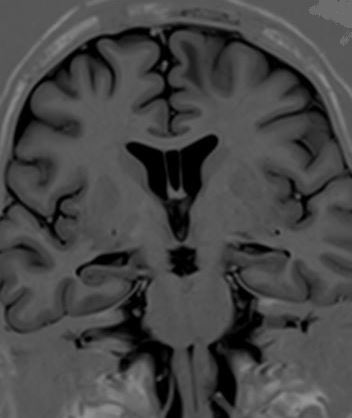
Cavum veli interpositi is usually an incidental finding at an MRI or CT scan and is mostly asymptomatic (see Images. Axial T2: Cavum Veli Interpositi and Coronal and Sagittal FLAIR: Cavum Veli Interpositi). The rare symptomatic cases treated with the collapse of the cavity, the shunting, or the endoscopic ventricular fenestration have always shown a good prognosis.[9][10]
Complications
The presence of the cavum veli interpositi in children has correlations with the development of psychosis spectrum disorders. Other studies supposed a relationship between CVI and the development of hydrocephalus, mental retardation, and seizures in children.[6][7] However, all studies about this matter concluded that further evaluation is needed to find whether there is any clinical complication related to the presence of CVI.
Deterrence and Patient Education
Patients need reassurance that the cavum veli interpositi is a normal anatomical variation, and it does not require surgical intervention except in very rare cases.
Pearls and Other Issues
The cavum veli interpositi is generally an occasional common finding during routine MRI or CT scans performed for other conditions. The role of CVI in human pathology is still uncertain, and further studies are needed.
Enhancing Healthcare Team Outcomes
The role of CVI in human pathology is still uncertain. For this reason, evaluating the rare symptomatic cases that require surgical treatment must receive an accurate interprofessional analysis. A rigorous clinical assessment and radiological examinations are necessary before any treatment. The interprofessional collaboration between neuroradiologists, neurologists, and neuropsychiatrists is essential.