Continuing Education Activity
The biceps tendon consists of 2 heads originating from the coracoid process (short head) and the supraglenoid tubercle of the scapula (long head). The tendon attaches to the bicipital tuberosity of the radius. The biceps tendon is a strong supinator of the forearm and serves as a weak elbow flexor. Some reports also mention the long-head biceps tendon’s contribution to the stability of the glenohumeral joint. Rupture of the proximal biceps tendon can be treated conservatively, while injury to its distal attachment usually needs surgical intervention. This activity reviews the causes, presentation, and diagnosis of the biceps tendon and highlights the role of the interprofessional team in the management of these patients.
Objectives:
- Identify the etiology of biceps tendon rupture.
- Review the presentation of biceps tendon rupture.
- Outline the management options available for biceps tendon rupture.
- Explain possible interprofessional team strategies for improving care coordination and communication to advance the management of biceps tendon rupture and improve outcomes.
Introduction
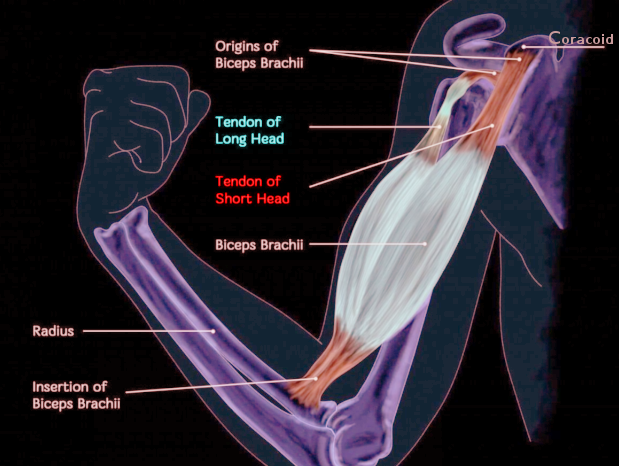
The biceps brachii muscle has two heads, one originating from the coracoid process (short head) and the other from the supraglenoid tubercle of the scapula and superior labrum (long head). The distal biceps tendon attaches to the bicipital tuberosity of the radius. The biceps tendon is a strong supinator of the forearm and serves as a weak elbow flexor. The long head (proximal biceps tendon) contributes to the stability of the glenohumeral joint. The majority of biceps rupture involves the long head.
Rupture of the proximal biceps tendon can be treated conservatively, while injury to its distal attachment usually needs surgical intervention. Patients generally recover successfully if they receive a timely diagnosis and treatment.[1][2][3]
Distal biceps tendon rupture can be complete avulsion or partial detachment from the lateral side of the radial tuberosity. Also, intersubstance muscle transaction has been reported, as in cases of a rope wrapped around the muscle (tug-of-war).
Etiology
Distal biceps rupture is from the excessive eccentric force as the arm is brought into extension from flexion. These activities include weightlifting, wrestling, and labor-intensive jobs. Proximal biceps rupture is generally not due to a unique mechanism of injury but is highly correlated with rotator cuff disease.[4]
Risk factors include age, smoking, obesity, use of corticosteroids, and overuse. Rare causes include the use of quinolones, diabetes, lupus, and chronic kidney disease.
Epidemiology
The incidence of distal biceps tendon rupture is around 2.55 per 100,000 patient-years. Most patients (more than 95%) are males, and injury events usually happen during middle age (35 years to 54 years).[5] The rupture of the distal biceps mainly involves the dominant limb. However, proximal biceps rupture is commonly seen in older patients, and its exact incidence is unknown, but it is more common than distal biceps rupture in older patients.
Pathophysiology
As mentioned above, age, overuse, smoking, and corticosteroid use contribute to tendon degeneration and, later, tendinopathy. Furthermore, there is a vascular watershed zone at the distal biceps tendon, and lack of sufficient blood supply also plays a crucial role in potentiating tendon rupture.[6]
The proximal tendon rupture, in most cases, occurs at the tendon-labral junction or the bony attachment. Distal tendon ruptures usually occur at the insertion of the radial tuberosity.
Histopathology
Histopathology studies show that the torn biceps tendon exhibit increased proteoglycan, collagen type III, matrix metallopeptidase-1, and matrix metallopeptidase-3, disorganized fiber arrangements, which were compatible with the finding of tendinopathy.
History and Physical
Patients suffering from biceps tendon rupture may complain of sudden sharp pain in the elbow or shoulder, depending on the site of the rupture. Usually, there is a history of sudden eccentric force to a flexed elbow. They may feel an audible "pop" in the affected arm at the time of the injury. Pain can persist for weeks to months. Pain may diminish if the tendon is completely torn. Patients usually complain of bulbous mass in the upper arm due to excessive retraction of the biceps muscle belly, known as "Popeye deformity." In obese individuals, it is generally hard to appreciate this popeye deformity.[7]
In patients with distal biceps, rupture, ecchymosis, swelling, and tenderness may be present in the antecubital fossa. If the bicipital aponeurosis (lacertus fibrosus) is involved, the muscle will be retracted to the upper arm, and a defect of the distal tendon will be palpable. The hook test can be used to identify the absence of the biceps tendon at its distal insertion. First, the examiner positions the patient's arm at 90 degrees of flexion and then supinates it. Second, the examiner tries to hook the tendon underneath the skin. The intact distal biceps tendon permits the examiner to hook the index finger under the biceps tendon. This test has a high specificity and sensitivity in diagnosing distal biceps tears.[8]
Surprisingly, there could be very few signs and symptoms other than pain in patients with proximal biceps tendon rupture. They may have ecchymosis of the proximal arm, sometimes extending up to the elbow. Proximal biceps rupture does not result in any long-term change in the elbow or shoulder strength. It is important to check for atrophy of the shoulder girdle muscle and shoulder impingement because proximal biceps tendon disorders are usually associated with rotator cuff pathology.
Evaluation
Diagnosis is often clinically made, while imaging is helpful when the diagnosis is unclear or partial rupture is considered. Three criteria are described for diagnosis:
- History of a single traumatic event. The patient will report a sudden, painful pop while the elbow is eccentrically loaded from flexion to extension. e.g., while doing a biceps curl.
- Grossly palpable and visible signs of retraction of the biceps muscle belly( reverse popeye deformity)
- Weakness of elbow flexion and supination of the forearm in cases of distal biceps rupture.
Provocative Tests
Hook Test: The examiner uses his index finger to hook it around the lateral edge of the biceps tendon while the patient is actively flexing and supinating the elbow. If the examiner can hook his finger 1 cm underneath the tendon, the test is positive, and the tendon is intact. A false-positive test can present in a partial tear or when lacertus fibrosus or underlying brachialis tendon are misinterpreted as an intact biceps tendon.[8]
Ruland Biceps Squeeze Test: It is performed with the elbow supported in 60 to 80 degrees of flexion, and the forearm is pronated. Then the examiner squeezes the distal biceps muscle belly. The test is positive when there is no supination of the patient's forearm or wrist.[9]
Partial ruptures may present with similar but subtle symptoms, and physical presentation is usually with pain, weakness, and no palpable defect, sometimes leading to delayed diagnosis. Ultrasound is an inexpensive, noninvasive tool to reveal the absence of the tendon, but it is highly technician-dependent. Radiographs generally cannot aid in diagnosis; occasionally can show a small fleck of bone from the radial tuberosity. Radiographs can be helpful to survey for other accompanying conditions, confirm the absence of another bony pathology, or sometimes reveal radial tuberosity hypertrophy or occasional avulsion fracture of the tuberosity. MRI is rarely necessary for diagnosis, but it is helpful to distinguish between the following:
- Complete versus partial tear
- Muscle substance versus tendon tear
- Degree of retraction
Treatment / Management
Management of biceps rupture depends on the site of rupture. The initial care involves ice, supportive elastic bandages, NSAIDs after the bleeding risk has resolved, and rest.
Rupture of the Proximal Biceps Tendon (Long Head)
Non-surgical treatment is usually sufficient for proximal tendon rupture, as it is more common in elderly patients. However, residual cosmetic deformity and some intermittent biceps muscle cramping may persist. Younger patients and female patients who are unwilling to accept cosmetic deformities and athletic patients with frequent cramping may opt for surgical intervention in the form of biceps tenodesis. The presence of associated rotator cuff pathology can also influence surgical management. Subpectoral tenodesis is the preferred approach for biceps tenodesis, where the tendon is attached to the bone in the bicipital groove. Sometimes this procedure is done concurrently with arthroscopic rotator cuff pathology treatment. Newer implants like interference screws and bio-absorbable suture anchors can be placed either through the open or arthroscopic approach to secure the tendon in the subpectoral space. All the approaches mentioned above are reported to achieve good clinical outcomes. However, there is limited data to show the superiority of the surgical intervention to the non-surgical approach.[10]
Rupture of the Distal Biceps Tendon
Non-operative treatment: Patients with low physical demands and multiple comorbidities are more suitable for conservative treatments. If the bicipital aponeurosis (lacertus fibrosis)is intact, the functional deficits due to biceps rupture can be minimized. Any patient who opts for conservative management of distal biceps tendon rupture needs to be counseled about the outcomes with 50% loss of sustained supination strength, 40% loss of supination strength, 30 % loss of flexion strength, and approximately 15% loss of grip strength.
Operative treatment: This is usually indicated in younger active patients who are unwilling to sacrifice their functions. Especially for the benefits of faster recovery and return to sports.[11][12][13] Most surgeons recommend operative treatment for rupture of the distal biceps tendon to regain the maximal strength of forearm supination and effectively relieve pain in the antecubital fossa. Operative management can be offered in acute, subacute, and for chronic and partial ruptures that failed conservative management. Ideally, the timing of surgical intervention should be as early as possible to avoid the need for a more extensive approach and dissection, which might be essential due to retraction and scarring of the distal biceps tendon from delayed intervention.
Surgical repair of the distal biceps tendon can be divided into 2 methods. The non-anatomic approach indicates sutures of the ruptured biceps tendon to the brachialis, which is a simple and efficient way to regain flexion strength. The anatomic approach indicates reinsertion of the ruptured tendon on the radial tuberosity, which reportedly has better results in restoring elbow flexion and forearm supination strength.
There are 2 techniques for surgical exploration and fixation of the torn distal biceps tendon.[14]
Anterior Single-Incision Technique
- The incision is over the anterior aspect of the elbow, at or just distal to the antecubital fossa. Deep dissection involves the interval between brachioradialis, which is laterally retracted, and pronator teres which is medially retracted.
- The most common complication is an injury to the lateral antebrachial cutaneous nerve exiting between the brachialis and brachioradialis at the antecubital fossa. Damage to the radial nerve or the posterior interosseous nerve is the most severe complication that would be encountered in this setting.[15] The posterior interosseous nerve can be protected by reducing lateral retraction and keeping the forearm supinated throughout the procedure.
- Less common heterotopic ossification and synostosis compared to dual incision technique.
Dual-Incision Technique
- The method is developed to avoid injury to the posterior interosseous nerve.
- It includes a smaller anterior incision over the antecubital fossa and a second posterolateral elbow incision. Deep dissection involves the interval between extensor carpi ulnaris and extensor digitorum communis. Anterior dissection is similar to the single-incision technique. Once the radial tuberosity is identified, blunt curved artery forceps are used to guide the second incision by sliding along the medial border of the tuberosity, piercing the anconeus, and tenting the skin where the second incision should be made.
- The dual-incision technique is more common in developing synostosis and heterotopic ossification than the single-incision approach.
Distal Biceps Tendon Fixation Techniques: Various options exist to fix the distal biceps tendon. Either through a bone tunnel, suture anchors, interosseous screw fixation, or suspensory cortical button.
The bony tunnels are made to anchor the distal bicep tendon. The smaller cortical holes on the radial side of the tuberosity are made with a 5/64-inch drill bit and connected to the larger bone tunnel. The drill holes are always positioned in precisely the same pattern, with 8 mm between the two drill holes and 7 mm between each drill hole and the bone tunnel. A locking modified Kessler stitch is placed with the No. 5 suture, and the suture's two ends are then inserted into the radial tuberosity's bone tunnel and extracted through the smaller drill holes. The sutures are tied over the bone after tensioning the tendon end.[16]
Limited exposure, the convenience of use, a lower risk of heterotopic ossification, and synostosis all favor anchor sutures. The radial tuberosity is exposed while the arm is supinated. An osteotome or burr is used for decortication, and two suture anchors are fastened to the tendon. Recent studies showed superior biomechanical results of anchor sutures over the bony tunnels.[17]
Numerous biomechanical experiments comparing all kinds of fixation have revealed that cortical buttons have the best strength. Compared to transosseous sutures, interference screws, and suture anchors, the cortical button had the highest failure load, ultimate stress distribution, and stiffness.[18] Biomechanical investigations have indicated that interference screws alone have pullout strengths that are stronger than suture anchors but weaker than the cortical button. The interference screw nearly resembles the stiffness and strength of a healthy tendon.[19]
Chronic ruptures of >4 weeks old are associated with high complication rates. Although primary anatomical tendon fixation may be feasible, biceps tendon retraction typically requires autograft or allograft augmentation with potential grafts such as fascia lata, semitendinosus, and the Achilles tendon. Hamer and Caputo promoted using the Achilles tendon autograft, claiming it offers enough graft and lowers morbidity. Additionally, they proposed a technique for employing lacertus fibrosis as their grafting substance.[20][21]
Differential Diagnosis
The diagnosis of the biceps tendon rupture sometimes is challenging. The investigator should bear in mind that proximal biceps tendon injury usually coexists with rotator cuff disorders and shoulder girdle instability.
Differential diagnosis includes:
- Rotator cuff disease
- Shoulder dislocation/instability
- Impingement syndrome
- Humeral/radial head fracture
Prognosis
Proximal biceps rupture patients generally recover with non-operative treatment and experience no long-term deficits in shoulder or elbow strength. However, distal biceps rupture can cause persistent pain and forearm supination weakness. Also, with a complete distal biceps rupture, the tendon can retract significantly, and later repair in chronic cases would be technically challenging. Hence the timely diagnosis of distal biceps rupture is critical, especially in a young active patient.[22]
Complications
- Lateral antebrachial cutaneous nerve (LABCN) injury is the most common complication.[23]
- Radial nerve or posterior interosseous nerve injury is the most severe complication.
- Superficial radial nerve injury.
- Synostosis: This is a bony bridge that develops between the radius and ulna, resulting in restriction or loss of pronation and supination. This can develop due to the proximal radius fracture from drilling a large tunnel or suture rupture when the bone tunnel technique is used. The incidence of synostosis has been reduced with the dual incision technique. Also, it can be minimized in a single incision technique by reducing dissection between the radius and ulna and reducing exposure of the ulna periosteum.
- Heterotopic ossification.
Postoperative and Rehabilitation Care
There are different rehabilitation protocols used after surgical repair of biceps tendon rupture. Patients are usually immobilized in 110 of flexion and moderate supination. Generally, initiating limited active or passive elbow flexion and supination is suggested during the early postoperative period. Strengthening exercises of the shoulder and wrist should also be incorporated into the post-operation rehabilitation protocol. [24]
Pearls and Other Issues
Chronic biceps tendon rupture is defined as a tendon tear of more than 4 weeks duration. Chronic rupture may be due to missed diagnosis or failure of conservative treatment. Partial tears or other coexisting pathology may complicate the diagnosis. MRI helps differentiate partial and complete tears of the biceps tendon.
Enhancing Healthcare Team Outcomes
Biceps tendon rupture is a relatively common disorder chiefly seen in people with repetitive lifting activities. The patient often first presents to the emergency department, urgent care clinic, or primary care provider, including a PA or nurse practitioner. The diagnosis is made by a clinical exam. An orthopedic consult is necessary if the primary clinician is unsure about management. Distal biceps tear should be promptly referred to orthopedic surgeons as a delay in treatment can cause significant proximal retraction of the tendon. Patients should be urged to undergo rehabilitation with a physical and/or occupational therapist for recovery. The interprofessional management of these injuries can include the patient's clinician or mid-level provider, orthopedist/surgeon, nursing staff, and physical therapists, all working collaboratively and communicating openly to optimize patient results. [Level 5]
The nurse should also educate the patient on injury prevention. The key to preventing this injury is educating the patient on modifying the risk factors, such as discontinuing smoking and stretching before physical activity. After the injury is diagnosed, work-specific or sports-specific training is often recommended before returning to the original activity. For most patients, full recovery is possible within 8 to 12 weeks.[22][25]