Continuing Education Activity
Balloon valvuloplasty is a cardiac intervention to open up a stenotic or stiffed heart valves (e.g., aortic or mitral) using a catheter with a balloon on the tip. It is also known as balloon valvotomy. It is a less invasive procedure because it is done by inserting a catheter into the blood vessel from groin percutaneously rather than valve replacement with cardiothoracic surgical or other open methods. This activity reviews the indications of balloon valvuloplasty and highlights the role of the interprofessional team in the management of these patients.
Objectives:
- Identify the indications for balloon valvuloplasty.
- Describe the technique of balloon valvuloplasty.
- Recall the potential complications of balloon valvuloplasty.
- Discuss interprofessional team strategies for improving care coordination and communication to advance the technique of balloon valvuloplasty and improve outcomes.
Introduction
Balloon valvuloplasty is a cardiac intervention to open up a stenotic or stiffed heart valves (e.g., aortic or mitral) using a catheter with a balloon on the tip. It is also known as balloon valvotomy. It is a less invasive procedure because it is done by inserting a catheter into the blood vessel from groin percutaneously rather than valve replacement with cardiothoracic surgical or other open methods. Balloon valvulotomy has several types, depending upon which heart valve is involved for example:
- Percutaneous balloon tricuspid valvuloplasty
- Percutaneous balloon pulmonary valvuloplasty
- Percutaneous balloon mitral valvuloplasty
- Percutaneous balloon aortic valvuloplasty[1]
Anatomy and Physiology
The heart is a four-chamber blood-pumping organ in the chest cavity. Blood flows from one chamber to another through valves. The following are the four valve classifications:
- Tricuspid valve: present between the right atrium and ventricle
- Pulmonary valve: present between the right ventricle and pulmonary article
- Mitral valve: a bicuspid valve present between the left atrium and ventricle
- Aortic valve: present between the left ventricle and ascending aorta
With the ongoing age, any inflammation or infection of the valve or a congenital heart defect causes the leaflets of valves to become stiff and calcified hence causing hindrance in the flow of blood from one chamber to another.[2]
Indications
The balloon valvuloplasty can be used for treating stenosis of tricuspid, pulmonary, mitral, and aortic valves, but in some cases, its potential risks outweigh its potential benefits. The following are the indications of balloon valvuloplasty in different valvular stenosis.
Tricuspid Valve Stenosis
The treatment of tricuspid stenosis is a combination of medical and valvular interventions. For patients with severe tricuspid valve stenosis, valve replacement surgery is preferred over balloon valvulotomy as most cases are associated with tricuspid regurgitation, and balloon valvuloplasty can worsen regurgitation. To choose balloon valvuloplasty over tricuspid valve replacement surgery in an isolated, symptomatic, severe tricuspid stenosis with mild to less tricuspid regurgitation, the surgical risk of a patient must be too high and outweigh disadvantages of over benefits of balloon valvuloplasty.
Pulmonary Valve Stenosis
Percutaneous balloon pulmonary valvulotomy (BPV) is preferred in moderate (gradient 40 to 60 mmHg) to severe (greater than 60 mmHg) pulmonary stenosis and it is the first-line treatment of typical dome-shaped valvular pulmonary stenosis in severe stenosis (gradient greater than 60 mmHg). BPV is also the preferred treatment in neonates with critical pulmonary stenosis.
Mitral Valve Stenosis
The percutaneous mitral balloon valvuloplasty is the treatment of choice in patients with mitral valve stenosis who have following features:
- Severe mitral stenosis
- Pliable, noncalcified mitral valves
- Symptomatic
- The absence of left atrial thrombus
- The absence of moderate to severe mitral regurgitation
- Older patients or who are at high risk for surgery
It is primarily performed in patients with rheumatic mitral stenosis. There is a little experience with percutaneous balloon mitral valvuloplasty in congenital mitral stenosis.
Aortic Valve Stenosis
- Use in calcified aortic stenosis: Use of balloon aortic valvotomy (BAV) is limited in calcified aortic stenosis. The use is generally limited to two settings:
- Percutaneous BAV is used as a bridge to surgical aortic valve replacement or transcatheter aortic valve replacement (TAVR) in a severely symptomatic aortic stenosis
- For patients with a severely symptomatic aortic stenosis who require an urgent non-cardiac surgery
- Use in congenital aortic stenosis: Balloon aortic valvotomy (or valvuloplasty, BAV) is a first-line treatment option for children and younger adults with aortic stenosis with the congenital disease without significant valve calcification.[3]
Contraindications
The percutaneous balloon valvuloplasty is contraindicated if in the presence of moderate to severe valvular regurgitation, infective endocarditis, vegetation, tumor, or irreversible noncardiac disease that is severely limiting life. [4]
Preparation
Admit the patient to the hospital a day before the procedure for preparation. A detailed history should be taken especially for cardiac and pulmonary diseases. Questions regarding age, weight, height, previous medical history, and medications including anticoagulants; heart, vascular, liver, kidney, and musculoskeletal disease and any current symptoms; any allergies in the past; complications during previous surgeries or complications of anesthesia in any family member; and social and sexual history should be documented. The patient is not allowed to eat or drink after midnight and should remain nill per oral (NPO) until after the procedure. [4]
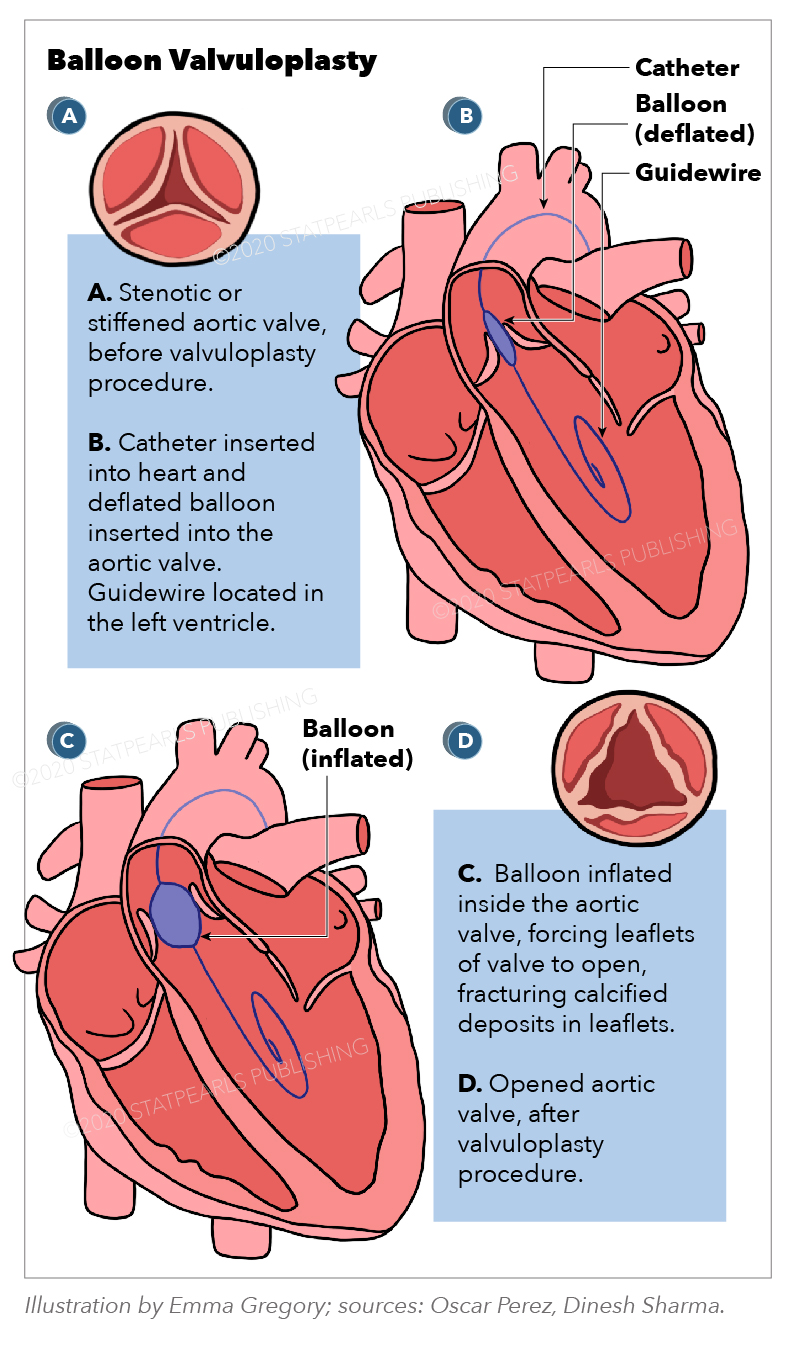
Technique or Treatment
The procedure started with a local anesthetic injection at the site of catheter insertion. Some IV sedative medicines are also given to help the patient relax before the procedure. After identifying the site of insertion just above the vessel in the groin, the doctor inserts an introducer into the vessel which helps with the later introduction of the catheter through the vessel into the heart. Following catheterization, the practitioner begins injecting contrast dye from the IV line to check the exact place of catheter and valve. As he or she approaches the required position, the balloon is inflated, forcing the calcified valve leaflets open. By fracturing the calcified deposits within the leaflets, the inflated balloon relieves the stenosis. After that, the practitioner deflates the balloon and removes the catheter. [5]
Complications
A variety of complications are associated with balloon valvuloplasty. The following are some of the main complications:
- Bleeding or hematoma formation at the catheter site insertion
- Infection at the catheter site
- Vessel damage due to multiple puncturing attempts
- Contrast dye allergy
- Arrhythmia
- Stroke
- Valve rupture requiring open heart surgery
- Ventricular rupture
- Valve regurgitation[6]
Clinical Significance
Balloon valvuloplasty is a less invasive than open-heart valve replacement, but it is not an alternative to valve replacements.
Studies comparing ballon tricuspid valvuloplasty to surgical tricuspid valve replacement are not available, so in most of the cases, tricuspid valve surgery is preferred. However, in high-risk surgical cases or with moderate to severe valvular regurgitation associated with tricuspid stenosis, balloon tricuspid valvuloplasty can be performed.
Pulmonary stenosis is a common congenital heart disease characterized by the right ventricular outflow obstruction. The clinical significance in treating pulmonary stenosis in children mainly depends on the severity of obstruction. Mild pulmonary stenosis (gradient <greater than 0 mmHg) does not require intervention. In moderate pulmonary stenosis (gradient 40 to 60 mmHg) and severe pulmonary stenosis (gradient greater than 60 mmHg), balloon pulmonary valvuloplasty is preferred.
The outcome of clinical trials on the clinical significance of percutaneous balloon mitral valvuloplasty compared to open and closed surgical commissurotomy was that percutaneous mitral balloon valvuloplasty was good or better than surgery in patients who were candidates for valvotomy.
Percutaneous balloon aortic valvuloplasty has a limited role in the treatment of calcific aortic stenosis. BAV is first-line therapy in children and younger adults with aortic stenosis due to congenital disease (generally due to bicuspid commissural fusion) without significant valve calcification.[3]
Enhancing Healthcare Team Outcomes
Balloon valvoplasty is a cardiac intervention technique that is widely used today to manage stenotic lesions. However, the preoperative work is usually done by an interprofessional team. The patients need to meet the indications for valvuloplasty to derive the most benefits. The nurse practitioner, physician assistant, anesthesiologist, and cardiologist should ensure patient fitness for the procedure. Usually, the nurse practitioner or physician assistant does the initial screening and reports back to the clinical team leader if there are concerns. The cardiologist should ensure and confirm with the nurse practitioner or physician assistant that the patient has the right indications for valvuloplasty. A nurse in the cardiac catheterization lab is dedicated to the monitoring of the patient during the procedure and should report to the cardiologist if any abnormal changes in vital signs develop. After the procedure, the recovery room nurses need to monitor the patient's vital signs and the site of puncture for hematoma formation and distal leg pulses. If there is an elevation in heart rate or drop in blood pressure, the physician should be contacted immediately. Only through an interprofessional team approach can the morbidity of this procedure be decreased and the outcomes improved. [Level V]