Introduction
The spine is the posterior portion of the human body. It is composed of the vertebrae interconnected with the spinal discs, known as nucleus pulposus. Together, this houses the spinal cord which extends from the brain, particularly, the medulla. It has a peripheral white matter and a central gray matter. In adults, the spinal cord ends at the lumbar level of L1 while in children it ends at L2-L3. The nerves then travel as a bundle known as the cauda equina. It is a bundle of spinal nerves and spinal nerve rootlets, which includes nerves L2 through L5, S1 through S5, and the coccygeal nerve.
The spinal cord is the port through which commands from the body and brain can communicate. It converts electrical signals from the body to physical and physiological responses. Many tracts run parallel to one another in the white matter. These send messages from the brain and body to each other. There are 31 spinal nerves that pass through the vertebral sections to their respective dermatome or target location to propagate the signals. It also has a blood supply and lymphatic system for drainage. The anterior spinal artery is a major artery providing nutrient-rich blood supply to the entire spinal cord section except for the dorsal columns. This artery runs along the entire length of the spinal cord anastomosing with other arteries.
The spinal cord is an area of many pathologies that can affect a large demographic. One of the most common complaints is back pain, which several etiologies can cause or it can be idiopathic. In recent years, surgical treatment for the conditions contributing to spinal cord injury is being performed. Spinal decompression is a very common procedure performed to relieve pressure on the impinged nerve. If blood flow to the anterior spinal artery is compromised, anticoagulation therapy can reestablish blood flow.
Structure and Function
The backbone of the body is the vertebral column which houses the extension of the human brain, known as the spinal cord. These 2 components have distinctive functions.
The brain houses the cortexes, frontal, parietal, temporal, and occipital. These work to control the different functions of the body by signaling. Signaling requires an axonal cell body that produces neurotransmitters and receives these signals by their dendritic processes. There are two broad categories of neurotransmitters, excitatory and inhibitory. Glutamate is an example of one of the most common excitatory neurotransmitters while GABA and glycine are examples of inhibitory neurotransmitters. These are the primary signal transducers that mediate commands.
The vertebral column is made up of bony segments separated by the nucleus pulposus. This is a remnant of the notochord in early embryology. It comprises of a jelly-like material that consists mainly of water, a loose network of collagen fibers. Its main function is to allow the vertebral disc to withstand forces of compression, such as shock and torsion. Several muscles originate and attach to the bony framework of the vertebral columns. These help the body move in different positions, such as, leaning forward and flexing side to side. The vertebral column is the foundation upon which the body relies on to complete its proper posture and physical activities.
Within the vertebral column, lies the spinal cord. It is a complex structure comprising neuronal cell bodies and tracts which exit through the intervertebral foramina. This is analogous to a railroad system exiting through tunnel systems to their target destination. The most important function of the spinal cord is to relay messages between the brain and the body. This is the medium through which it converts electrical signals into physical commands. After exiting, each nerve travels to its respective dermatome and innervates the muscles of that region. The spinal cord also uses the same neurotransmitters as in the brain.
Embryology
The spinal cord undergoes its inception during the third week of the embryonic period. Gastrulation is the process of specializing in a multi-layered structure from a single-layered blastula. This trilaminar structure has three germ layers known as the ectoderm, mesoderm, and endoderm. The ectoderm gives rise to the epidermis, the nervous system, and the neural crest cells. The endoderm gives rise to the epithelium of the digestive system and the respiratory system while the mesoderm gives rise to muscle, bone, and connective tissues. The ectoderm is the focus of the embryological origins of the nervous system, more commonly known as the neuroectoderm. It results in the formation of the notochord that induces the formation of the neural plate. The process of neurulation begins after it forms the neural plate. The plate invaginates to form the neural tube which pinches off completely from the neuroectoderm. This takes place during the third week of development. From the neural tube, it forms the brain and differentiates into three sections, the hindbrain, the midbrain, and the forebrain. The neural crest cells also arise from the embryonic ectoderm cell layer which specializes in the pigment cells in the skin, ganglia of the autonomic nervous system, dorsal root ganglia, cells of the adrenal medulla, and parafollicular cells in the thyroid.
There is additional signaling by the Sonic Hedgehog (SHH) ligand and the translation of the homeotic genes (HOX). These are directors in the subsequent development of the vertebral column and the segmentation of the body. Primarily, these specify the 2 major axes of the nervous system. One axis is the dorsal-ventral (D-V), and the other is anterior-posterior. In this way, the embryo forms a 3-dimensional form.
Blood Supply and Lymphatics
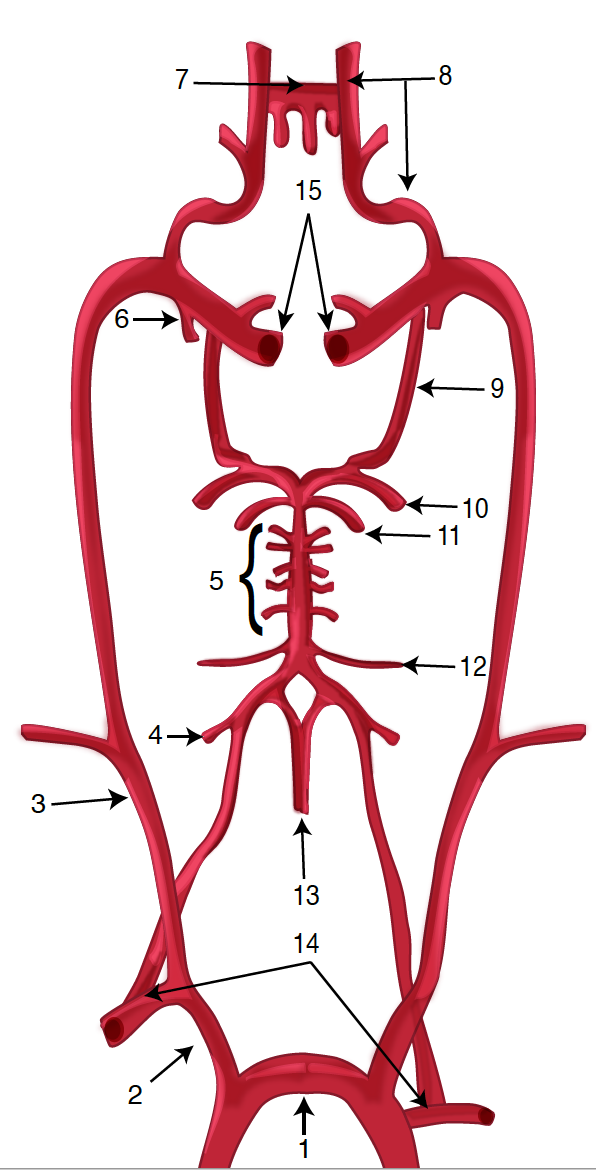
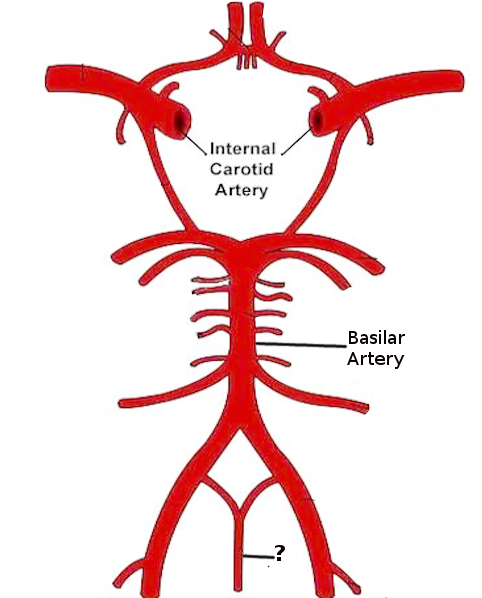
The brain and the spinal cord receive their blood supply from the carotid arteries which branch from the aortic arch and the vertebral arteries. These branch off from the central subclavian arteries. The internal carotid artery is the main supplier of nutrient-rich blood to the brain. The spinal cord, however, receives its supply from the branches of the vertebral arteries. Each artery courses along the side of the neck forming a single basilar artery in the brain superiorly while branching bilaterally inferiorly to form a single anterior spinal artery at the level of the foramen magnum. This supplies the anterior portion of the spinal cord which covers most except for the dorsal columns. These are more posterior and require tributaries to supply this part. The dorsal columns receive blood supply by the right and left posterior spinal arteries which also originate from the vertebral artery and together, these travel in the subarachnoid space.
The anterior spinal artery is the major blood supply for the spinal cord. It descends from the level of the foramen magnum along the anterior surface of the spinal cord. As it continues to descend, the artery receives communication with other branches that enter the spinal canal through the intervertebral foramen. The artery of Adamkiewicz anastomosis with the anterior spinal artery which feeds the lower thoracic, lumbar, and sacral spinal cord.[1]
The venous drainage of the spinal cord is accomplished by the 3 anterior and 3 posterior spinal veins. These veins drain into the internal and external vertebral plexuses which empty into the systemic segmental veins.
The lymphatics of the spinal cord are indirectly connected with the general lymphatic and venous systems. They open into the subarachnoid space.
Nerves
The spinal cord is arranged anatomically with a central gray matter surrounded by peripheral white matter. The gray matter comprises of cell bodies divided into the dorsal (posterior), lateral, and ventral (anterior) “horns.” These are the primary receivers of the incoming sensory information. The white matter is composed of tracts that are ascending and descending to their respective destinations. The white matter divides into the dorsal, lateral, and ventral columns. The dorsal columns carry ascending sensory information from somatic mechanoreceptors. The lateral columns contain axons that carry motor commands from the cerebral cortex to the spinal motor neurons. These are known as the corticospinal tracts. The ventral columns carry ascending pain and temperature information and descending motor information. These are known as the spinothalamic tracts.
At each level of the spinal cord, there is a bilateral set of afferent nerves and efferent nerves. These nerves travel through the intervertebral foramina to their perspective dermatome and myotome. The afferent signals arrive at the spinal cord via the dorsal nerve roots which are made up of sensory fibers. As they near the ventral aspect of the spinal cord, they encounter a dilation known as the dorsal root ganglion (DRG). A ganglion is a set of neuronal cell bodies that are processed before continuing to their destination. The DRGs are located in the intervertebral foramina at each level of the spinal cord except for the sacral DRGs which are located in the vertebral canal and the coccygeal DRGs which are intradural.[2]
The nerve synapses onto the interneurons within the gray matter which synapses onto the efferent neurons. Most interneurons are primarily inhibitory and use the neurotransmitters GABA or glycine to achieve this response. The efferent neurons are also known as the lower motor neurons, which exit through the intervertebral foramina and synapse onto their target organ.
There are 31 pairs of spinal nerves, one on either side of the vertebral column. These are divided into the cervical, thoracic, lumbar, sacral, and coccygeal regions. The cervical region gives rise to 8 cervical nerves (C1-C8) which exit above the corresponding vertebrae. The thoracic region gives rise to 12 thoracic nerves (T1-T12), which exit that exit below the vertebral levels. The sacral region gives rise to 5 sacral nerves, and the coccygeal region gives rise to 1 nerve. The sacral and coccygeal regions are fused, and they exit the spinal cord by the cauda equina. The cauda equina is a bundle of nerves that originate from the L2 level and carries all the nerves below it in a tail-like fashion.
Muscles
The average length of the vertebral column in males is about 71 cm and in females about 61 cm. This involves a large area for many muscles to attach to the skeletal backbone. The main purpose of these muscle attachments is to support the trunk and hold the body upright. There are 3 sets of muscles:
- Extensors: The erector spinae are a group of muscles are located posterior to the spine. These include the iliocostalis and spinalis in the thoracic region and interspinales in the lumbar region. They attach from the sacrum, medial iliac crest, vertebral transverse and spinous processes to the angle of the ribs and transverse and spinous processes of the vertebrae. They function to help to stand and lift objects. Other extensors in the thoracic region include semispinalis and rotatores muscles. In the lumbar region, the longissimus lumborum and iliocostalis lumborum play a role in extension.
- Flexors: These are attached anteriorly to the spine. These muscles primarily comprise the abdominal muscles. These allow us to flex, lean forward, and arch the lower back.
- Oblique muscles: These muscles are attached laterally to the spine. They function to rotate the spine and maintain proper posture. Among these, the quadratus lumborum originates from the posterior border of the iliac crest and inserts on the inferior border of 12th rib and L1 through L4. They function to flex the vertebral column laterally. Other muscles include iliocostalis lumborum, intertransversarii lateralis, and intertransversarii medialis.
Physiologic Variants
The spinal cord is also the distinction between the central nervous system and the peripheral nervous system. Its main function is to mediate homeostasis. This involves the use of the neurotransmitters are the primary signals to aid in propagating nerve impulses. In addition, the spinal cord plays the role of an integrator of information. The tracts in the white matter carry impulses to and from the brain while the gray matter of the cord contains cell bodies.
The spinal cord is the location where electrical signals are converted to physical voluntary and involuntary responses. They propagate these through the major neurotransmitters, glutamate, GABA, and glycine.
Surgical Considerations
Nerve impingement is a problem faced by many because it has many etiologies ranging from accidental to spinal stenosis. The procedure to relieve the nerve from being irritated is spinal decompression. This can be performed at any point in the length of the spinal cord whether it may be cervical or lumbar.
A minimally invasive lumbar procedure can be performed to treat the lumbar spinal stenosis.[3] There are several common techniques for decompression. These include discectomy which involves removing a portion of an intervertebral disc to relieve pressure on the nearby roots. This procedure is most commonly used for a herniated disc in the lumbar region. Laminectomy or laminotomy is a procedure in which a small part of the bony arches of the spinal canal is removed. A laminectomy procedure removes the entire lamina while the laminotomy removes just a section of the lamina. The foraminectomy or foraminotomy procedure expands the area for the nerve roots to exit the spinal cord. A portion of the bone or tissue is removed. Osteophyte removal involves the removal of the bony growths known as osteophytes or bone spurs. A corpectomy is a procedure that removes the body of a vertebra and the discs. This requires the additional step to fuse the vertebrae to stabilize the spine. All these procedures are meant to increase space for the nerves to pass freely without irritation.
As with every surgical procedure, there are risks. These include infection, bleeding, blood clots, spinal leaks, nerve or tissue damage, and allergic reaction to anesthesia. It is important to take into consideration the age of the patient as elderly patients may take a longer time to heal and their history. Associated conditions, such as diabetes mellitus, can delay wound healing and are considered an added risk. Most patients stay in the hospital for an average of 4 to 5 days, and they may require rehabilitation services.
Clinical Significance
The spinal cord has a significant amount of length in the body. It holds the body upright and a medium through which nerves can enter and exit to their target locations.
In ages younger than 15, it is very rare to encounter a spinal cord injury. Usually, it is the motor vehicle accidents that have been shown to be the major contributor. Data showed, 68% of the patients had an injury to the level of C1 to C4, 25% had the injury to the levels of C5 to C7, and 7% of the pediatric population had the injury to both locations.[4]
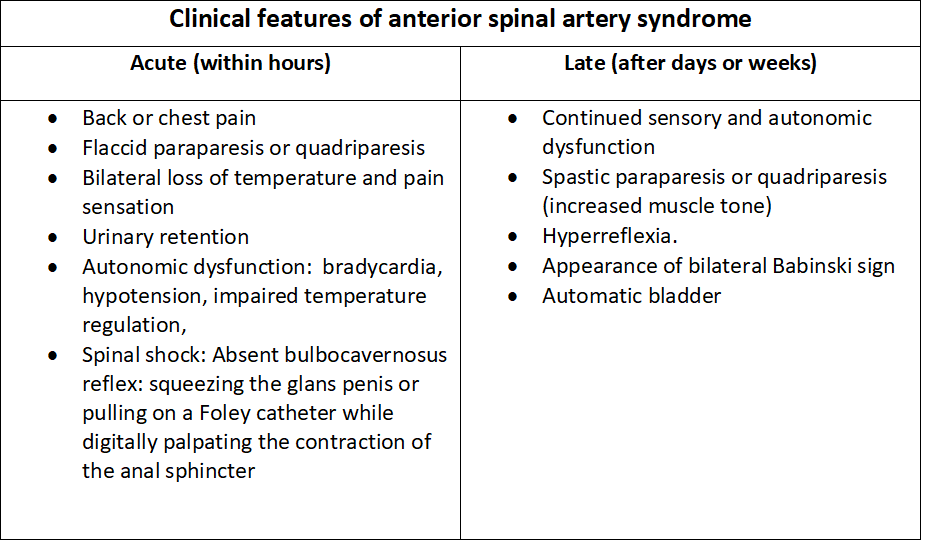
Vascular etiology can cause spinal cord injury, such as a stroke. A stroke of the anterior spinal artery results in loss of blood supply to a major portion of the spinal cord. This is known as anterior spinal artery syndrome, which is characterized by loss of motor function below the level of injury, loss of sensations carried by the anterior columns of the spinal cord (pain and temperature) while not affecting proprioception carried by the dorsal columns. The blood supply does not affect this dorsal portion of the spinal cord.
In adolescents, adults, and the elderly, the criteria for spinal cord injury is more broadened. There is a further distinction between the 2 genders. Adolescents experience spinal cord injury primarily through accidental means. Many of these patients experience back pain. One cause is the slipped disk or herniated disk. The result of wear and tear may cause this. As people age, the spinal discs lose their elasticity. They can lose their gel-like fluid and become brittle and cracked. In adults, it is due to lifting a heavy object or accident. These discs, also known as the nucleus pulposus, are between 2 vertebrae. Once slipped, the disc impinges on the nearby nerve irritating it. The symptoms experienced by these patients can be sudden or severe shooting pain.
Women experience a weakening of the bones, especially after menopause. The hormone estrogen is protective as it acts as an inhibitor for the resorption of bone. After menopause, the levels of estrogen decrease, and bone resorption occurs at a greater rate than bone formation. Women require hormone replacement and vitamin D supplements to prevent bone fracture. The pathology is known as osteoporosis, and this can take place in the vertebrae leading to vertebral compression fractures.
The elderly can experience spinal stenosis, a serious arthritic spine problem. Stenosis is a narrowing or constriction of a neural structure such as the spinal cord or a nerve. Once this happens, the stenotic portion impinges on the nerve causing chronic pain. There are 2 types of stenosis in the vertebral column; Cervical stenosis and lumbar stenosis. Cervical stenosis refers to the narrowing of the spinal canal in the neck. Unlike the lumbar spine, the true spinal cord is located in the cervical spine and not just the nerves. Damage to the spinal cord at this level can cause total body paralysis and even quadriplegia. Symptoms rarely include neck pain, but rather numbness and clumsiness of the hands. They also have difficulty in walking due to balance problems. The other stenosis is lumbar, which refers to the narrowing of the low back area. This the region where the spinal cord ends and the nerves travel in a bundle known as the cauda equina. The major complaint is numbness in legs, and it is relieved by leaning on a cane or taking frequent breaks. This is a chronic condition and patients complain for years to a point where they can longer walk for more than a few minutes. The problem becomes severe when sacral functions are affected, such as urinary and fecal incontinence. This requires a surgical approach to attempt to resolve the problem. A study was conducted to identify the causes and the rehabilitation outcome of traumatic spinal cord injury in patients older than 60 years at the time of injury. The results showed that 34 patients (77%) were injured after falling from a height, 24 with cervical lesions. Thirty-five patients (80%) had incomplete lesions, and they had the best outcome regarding functionality. They concluded a high proportion of the patients had cervical spinal stenosis and incomplete spinal cord injury; most of them regained good function.[5]
An additional problem of the spine is the physical distortion of the spine itself. The terms are known as kyphosis, scoliosis, and lordosis. Kyphosis is the abnormal convex curvature of the spine mostly involving the thoracic region. The most obvious symptom is a rounded back, general fatigue, weakness, and pain in the muscles. Scoliosis is an unnatural sideways curvature of the spine. The curvature can be mild or it can increase. Symptoms include periodic pain in the lower back and unevenly aligned arms and hips. Lordosis is the abnormal concave curvature of the spine. It can either be lumbar lordosis or cervical lordosis. Symptoms of these conditions include lower back pain, inward curve of the spine, a limited range of motion, and weakness in the lumbar muscles.
Other Issues
The disorders of the spine are major health and social problems. Whether etiological or idiopathic, back pain is a major problem for many patients. According to the Global Burden of Disease 2010, low back pain is the single leading cause of disability worldwide. It is also one of the most common reasons for missed work. The Lancet, in 2010 musculoskeletal disorders caused nearly 166 million years lived with a disability (YLDs), with neck and low back pain accounting for 69.9% of the total. In Poland, in 2014, the low back pain was self-reported by 28.4% of women and 21.2% of men aged 15 and older.[6]
As part of the aging process, the spine undergoes continuous changes as a response to physiologic axial load. These result in pathological degenerative changes that may be asymptomatic in adults and the elderly. The degeneration involves the bony structures and the intervertebral disk.[7]