[1]
Pacheco JM, Yilmaz M, Rice L. How low is too low: Statin induced hemolysis. American journal of hematology. 2016 Feb:91(2):267. doi: 10.1002/ajh.24105. Epub 2015 Oct 16
[PubMed PMID: 26147873]
[2]
Privitera G, Meli G. An unusual cause of anemia in cirrhosis: spur cell anemia, a case report with review of literature. Gastroenterology and hepatology from bed to bench. 2016 Fall:9(4):335-339
[PubMed PMID: 27895861]
Level 3 (low-level) evidence
[3]
Anoop P, Parker-Williams J. Morphological diagnosis of abetalipoproteinemia and the importance of a freshly prepared peripheral smear. European journal of haematology. 2009 Dec 1:83(6):606. doi: 10.1111/j.1600-0609.2009.01302.x. Epub 2009 Jun 22
[PubMed PMID: 19552676]
[4]
El Nabouch M, Rakotoharinandrasana I, Ndayikeza A, Picard V, Kayemba-Kay's S. Infantile pyknocytosis, a rare cause of hemolytic anemia in newborns: report of two cases in twin girls and literature overview. Clinical case reports. 2015 Jul:3(7):535-8. doi: 10.1002/ccr3.288. Epub 2015 May 8
[PubMed PMID: 26273436]
Level 3 (low-level) evidence
[5]
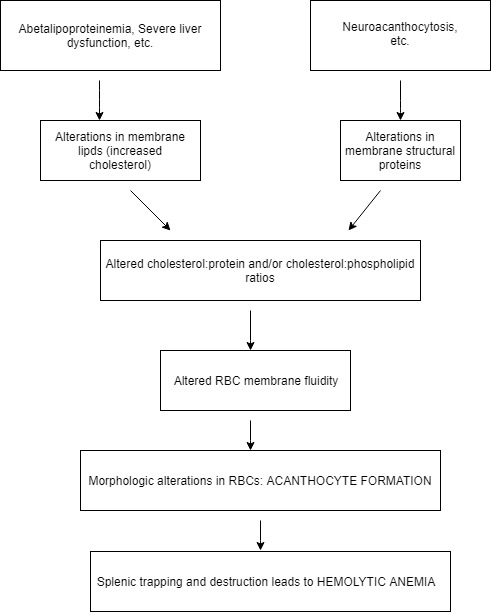
Wong P. A basis of the acanthocytosis in inherited and acquired disorders. Medical hypotheses. 2004:62(6):966-9
[PubMed PMID: 15142658]
[6]
Malik P, Bogetti D, Sileri P, Testa G, Blumenthal SA, Wiley TE, Layden TJ, Benedetti E. Spur cell anemia in alcoholic cirrhosis: cure by orthotopic liver transplantation and recurrence after liver graft failure. International surgery. 2002 Oct-Dec:87(4):201-4
[PubMed PMID: 12575799]
[7]
Miki K, Maruki T, Imashuku S. Plasmapheresis for Spur Cell Anemia in a Patient with Alcoholic Liver Cirrhosis. Case reports in hematology. 2018:2018():9513946. doi: 10.1155/2018/9513946. Epub 2018 Jun 21
[PubMed PMID: 30034891]
Level 3 (low-level) evidence
[8]
Chitale AA, Sterling RK, Post AB, Silver BJ, Mulligan DC, Schulak JA. Resolution of spur cell anemia with liver transplantation: a case report and review of the literature. Transplantation. 1998 Apr 15:65(7):993-5
[PubMed PMID: 9565106]
Level 3 (low-level) evidence
[9]
Adam MP, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, Burnett JR, Hooper AJ, Hegele RA. Abetalipoproteinemia. GeneReviews(®). 1993:():
[PubMed PMID: 30358967]
[10]
Di Filippo M, Créhalet H, Samson-Bouma ME, Bonnet V, Aggerbeck LP, Rabès JP, Gottrand F, Luc G, Bozon D, Sassolas A. Molecular and functional analysis of two new MTTP gene mutations in an atypical case of abetalipoproteinemia. Journal of lipid research. 2012 Mar:53(3):548-555. doi: 10.1194/jlr.M020024. Epub 2012 Jan 11
[PubMed PMID: 22236406]
Level 3 (low-level) evidence
[11]
Jung HH, Danek A, Walker RH. Neuroacanthocytosis syndromes. Orphanet journal of rare diseases. 2011 Oct 25:6():68. doi: 10.1186/1750-1172-6-68. Epub 2011 Oct 25
[PubMed PMID: 22027213]
[12]
Hermann A, Walker RH. Diagnosis and treatment of chorea syndromes. Current neurology and neuroscience reports. 2015:15(2):514. doi: 10.1007/s11910-014-0514-0. Epub
[PubMed PMID: 25620691]
[13]
Walker RH. Management of Neuroacanthocytosis Syndromes. Tremor and other hyperkinetic movements (New York, N.Y.). 2015:5():346. doi: 10.7916/D8W66K48. Epub 2015 Oct 19
[PubMed PMID: 26504667]
[14]
Asano K, Osawa Y, Yanagisawa N, Takahashi Y, Oshima M. Erythrocyte membrane abnormalities in patients with amyotrophic chorea with acanthocythosis. Part 2. Abnormal degradation of membrane proteins. Journal of the neurological sciences. 1985 May:68(2-3):161-73
[PubMed PMID: 3159851]
[15]
Olivieri O, De Franceschi L, Bordin L, Manfredi M, Miraglia del Giudice E, Perrotta S, De Vivo M, Guarini P, Corrocher R. Increased membrane protein phosphorylation and anion transport activity in chorea-acanthocytosis. Haematologica. 1997 Nov-Dec:82(6):648-53
[PubMed PMID: 9499662]
[16]
Clark MR, Aminoff MJ, Chiu DT, Kuypers FA, Friend DS. Red cell deformability and lipid composition in two forms of acanthocytosis: enrichment of acanthocytic populations by density gradient centrifugation. The Journal of laboratory and clinical medicine. 1989 Apr:113(4):469-81
[PubMed PMID: 2703759]
[17]
Perillie PE, Tembrevilla C. Letter: Red-cell changes in hypothyroidism. Lancet (London, England). 1975 Dec 6:2(7945):1151-2
[PubMed PMID: 53639]
Level 3 (low-level) evidence
[18]
Doll DC, List AF, Dayhoff DA, Loy TS, Ringenberg QS, Yarbro JW. Acanthocytosis associated with myelodysplasia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1989 Oct:7(10):1569-72
[PubMed PMID: 2778485]
[19]
Filippini A, Villa G, Corrocher R, De Franceschi L. Acute hemolytic anemia with acanthocytosis associated with high-dose misoprostol for medical abortion. Annals of emergency medicine. 2007 Sep:50(3):289-91
[PubMed PMID: 17084939]