[1]
Chang LR, Anand P, Varacallo M. Anatomy, Shoulder and Upper Limb, Glenohumeral Joint. StatPearls. 2024 Jan:():
[PubMed PMID: 30725703]
[2]
Saha AK. Dynamic stability of the glenohumeral joint. Acta orthopaedica Scandinavica. 1971:42(6):491-505
[PubMed PMID: 5144199]
[3]
Clavert P. Glenoid labrum pathology. Orthopaedics & traumatology, surgery & research : OTSR. 2015 Feb:101(1 Suppl):S19-24. doi: 10.1016/j.otsr.2014.06.028. Epub 2015 Jan 14
[PubMed PMID: 25596985]
[4]
Burkhart SS,De Beer JF, Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy : the journal of arthroscopic
[PubMed PMID: 11027751]
[5]
Sofu H, Gürsu S, Koçkara N, Oner A, Issın A, Camurcu Y. Recurrent anterior shoulder instability: Review of the literature and current concepts. World journal of clinical cases. 2014 Nov 16:2(11):676-82. doi: 10.12998/wjcc.v2.i11.676. Epub
[PubMed PMID: 25405191]
Level 3 (low-level) evidence
[6]
Taylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. The American journal of sports medicine. 1997 May-Jun:25(3):306-11
[PubMed PMID: 9167808]
[7]
Aronen JG. Anterior shoulder dislocations in sports. Sports medicine (Auckland, N.Z.). 1986 May-Jun:3(3):224-34
[PubMed PMID: 3635924]
[8]
Murray IR,Ahmed I,White NJ,Robinson CM, Traumatic anterior shoulder instability in the athlete. Scandinavian journal of medicine
[PubMed PMID: 22738342]
[9]
Mizuno K, Nabeshima Y, Hirohata K. Analysis of Bankart lesion in the recurrent dislocation or subluxation of the shoulder. Clinical orthopaedics and related research. 1993 Mar:(288):158-65
[PubMed PMID: 8458129]
[10]
Su T, Chen GX, Yang L. Diagnosis and treatment of labral tear. Chinese medical journal. 2019 Jan 20:132(2):211-219. doi: 10.1097/CM9.0000000000000020. Epub
[PubMed PMID: 30614856]
[11]
Kazár B, Relovszky E. Prognosis of primary dislocation of the shoulder. Acta orthopaedica Scandinavica. 1969:40(2):216-24
[PubMed PMID: 5365161]
[12]
Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. The Journal of bone and joint surgery. American volume. 1996 Nov:78(11):1677-84
[PubMed PMID: 8934481]
[13]
Hovelius L. Incidence of shoulder dislocation in Sweden. Clinical orthopaedics and related research. 1982 Jun:(166):127-31
[PubMed PMID: 7083659]
[14]
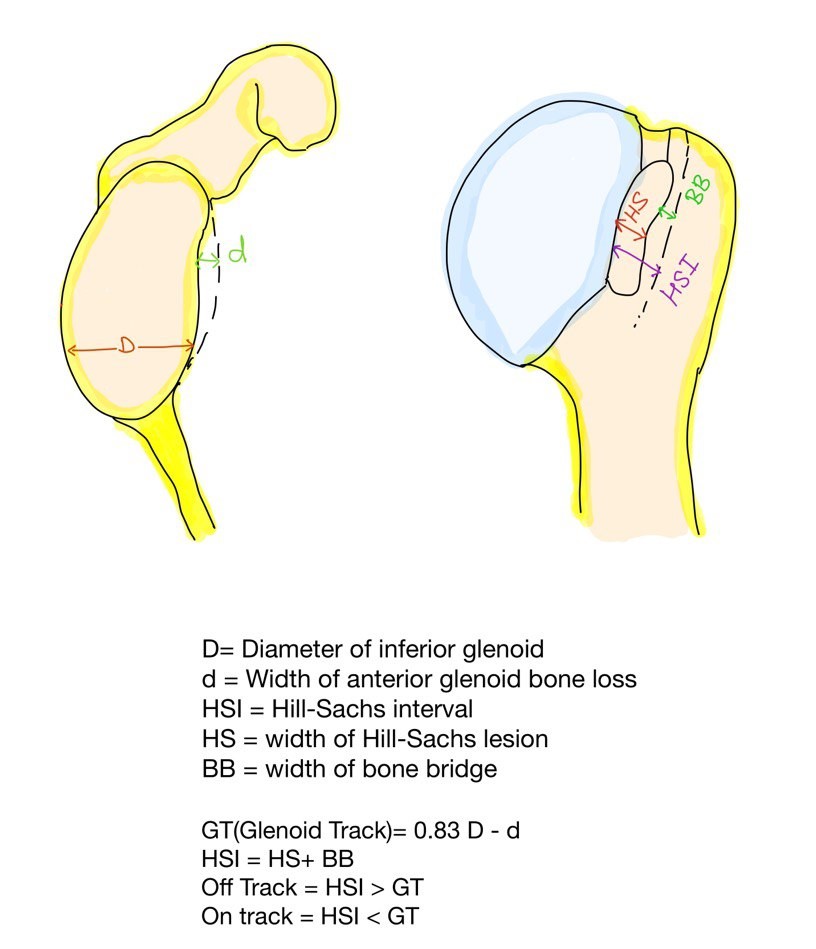
Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from "engaging/non-engaging" lesion to "on-track/off-track" lesion. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2014 Jan:30(1):90-8. doi: 10.1016/j.arthro.2013.10.004. Epub
[PubMed PMID: 24384275]
[15]
Gill TJ,Zarins B, Open repairs for the treatment of anterior shoulder instability. The American journal of sports medicine. 2003 Jan-Feb;
[PubMed PMID: 12531772]
[16]
Gill TJ, Micheli LJ, Gebhard F, Binder C. Bankart repair for anterior instability of the shoulder. Long-term outcome. The Journal of bone and joint surgery. American volume. 1997 Jun:79(6):850-7
[PubMed PMID: 9199382]
[17]
Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. The Journal of bone and joint surgery. American volume. 1978 Jan:60(1):1-16
[PubMed PMID: 624747]
[18]
Robinson CM, Shur N, Sharpe T, Ray A, Murray IR. Injuries associated with traumatic anterior glenohumeral dislocations. The Journal of bone and joint surgery. American volume. 2012 Jan 4:94(1):18-26. doi: 10.2106/JBJS.J.01795. Epub
[PubMed PMID: 22218378]
[19]
Skupiński J,Piechota MZ,Wawrzynek W,Maczuch J,Babińska A, The Bony Bankart Lesion: How to Measure the Glenoid Bone Loss. Polish journal of radiology. 2017;
[PubMed PMID: 28243338]
[20]
Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2004 Feb:20(2):169-74
[PubMed PMID: 14760350]
[21]
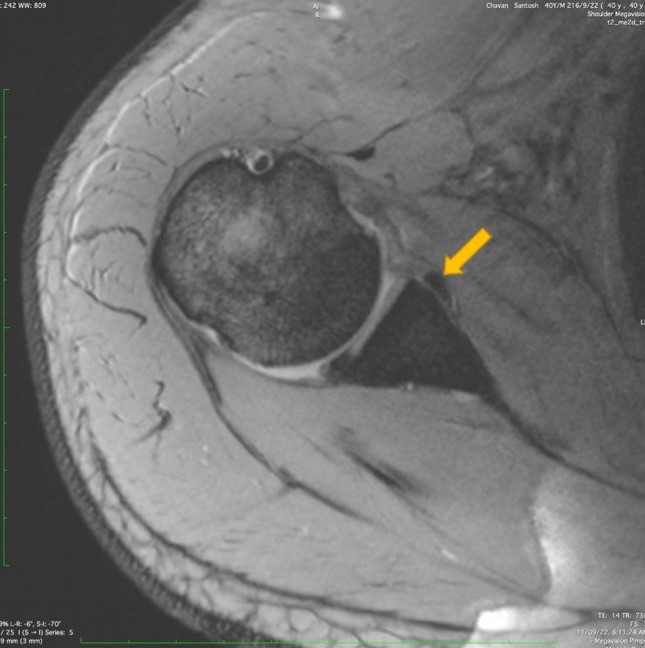
Provencher MT, Frank RM, Leclere LE, Metzger PD, Ryu JJ, Bernhardson A, Romeo AA. The Hill-Sachs lesion: diagnosis, classification, and management. The Journal of the American Academy of Orthopaedic Surgeons. 2012 Apr:20(4):242-52. doi: 10.5435/JAAOS-20-04-242. Epub
[PubMed PMID: 22474094]
[22]
Gyftopoulos S, Yemin A, Beltran L, Babb J, Bencardino J. Engaging Hill-Sachs lesion: is there an association between this lesion and findings on MRI? AJR. American journal of roentgenology. 2013 Oct:201(4):W633-8. doi: 10.2214/AJR.12.10206. Epub
[PubMed PMID: 24059403]
[23]
Itoi E. 'On-track' and 'off-track' shoulder lesions. EFORT open reviews. 2017 Aug:2(8):343-351. doi: 10.1302/2058-5241.2.170007. Epub 2017 Aug 1
[PubMed PMID: 28932486]
[24]
Loh B, Lim JB, Tan AH. Is clinical evaluation alone sufficient for the diagnosis of a Bankart lesion without the use of magnetic resonance imaging? Annals of translational medicine. 2016 Nov:4(21):419
[PubMed PMID: 27942510]
[25]
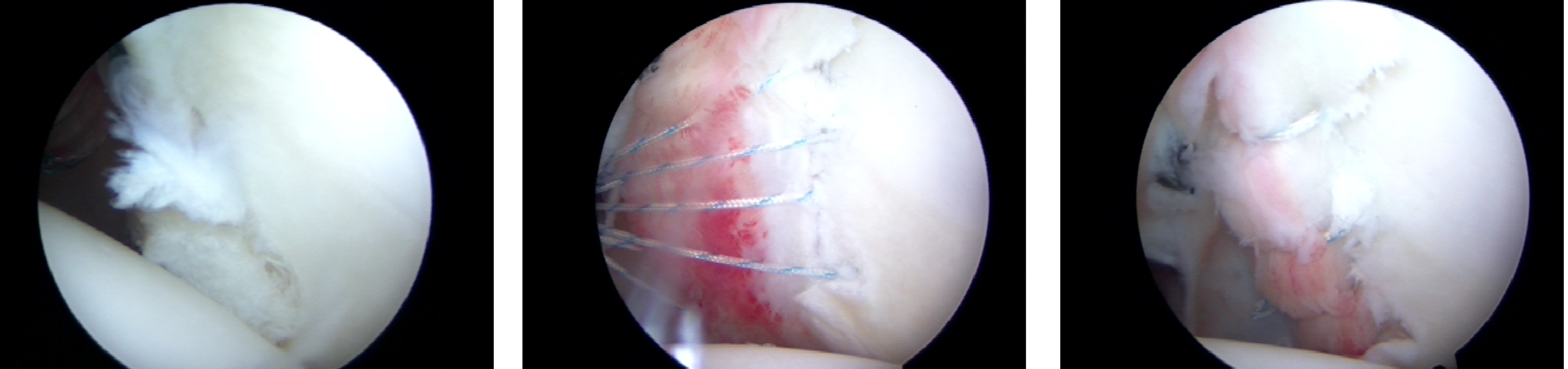
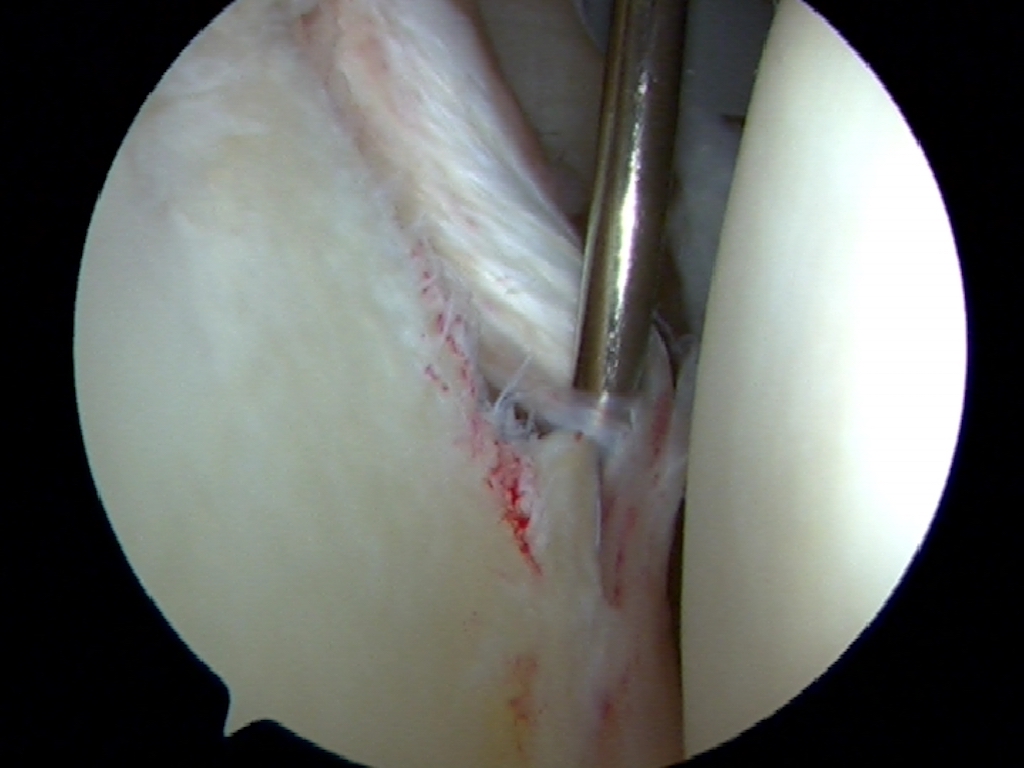
Gül O, Okutan AE, Ayas MS. Arthroscopic glenoid labral lesion repair using all-suture anchor for traumatic anterior shoulder instability: short-term results. Journal of shoulder and elbow surgery. 2019 Oct:28(10):1991-1997. doi: 10.1016/j.jse.2019.03.003. Epub 2019 May 14
[PubMed PMID: 31101476]
[26]
Farber AJ,Castillo R,Clough M,Bahk M,McFarland EG, Clinical assessment of three common tests for traumatic anterior shoulder instability. The Journal of bone and joint surgery. American volume. 2006 Jul;
[PubMed PMID: 16818971]
[27]
Bushnell BD, Creighton RA, Herring MM. The bony apprehension test for instability of the shoulder: a prospective pilot analysis. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2008 Sep:24(9):974-82. doi: 10.1016/j.arthro.2008.07.019. Epub
[PubMed PMID: 18760203]
Level 3 (low-level) evidence
[28]
Provencher MT, LeClere LE, King S, McDonald LS, Frank RM, Mologne TS, Ghodadra NS, Romeo AA. Posterior instability of the shoulder: diagnosis and management. The American journal of sports medicine. 2011 Apr:39(4):874-86. doi: 10.1177/0363546510384232. Epub 2010 Dec 4
[PubMed PMID: 21131678]
[29]
Morey VM, Singh H, Paladini P, Merolla G, Phadke V, Porcellini G. The Porcellini test: a novel test for accurate diagnosis of posterior labral tears of the shoulder: comparative analysis with the established tests. Musculoskeletal surgery. 2016 Dec:100(3):199-205
[PubMed PMID: 27591779]
Level 2 (mid-level) evidence
[30]
Kim SH,Park JS,Jeong WK,Shin SK, The Kim test: a novel test for posteroinferior labral lesion of the shoulder--a comparison to the jerk test. The American journal of sports medicine. 2005 Aug;
[PubMed PMID: 16000664]
[31]
Valencia Mora M,Ibán MÁR,Heredia JD,Gutiérrez-Gómez JC,Diaz RR,Aramberri M,Cobiella C, Physical Exam and Evaluation of the Unstable Shoulder. The open orthopaedics journal. 2017;
[PubMed PMID: 29114336]
[32]
Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. The Journal of pediatrics. 2011 Jan:158(1):119-23, 123.e1-4. doi: 10.1016/j.jpeds.2010.07.021. Epub 2010 Sep 17
[PubMed PMID: 20850761]
[33]
Rozing PM, de Bakker HM, Obermann WR. Radiographic views in recurrent anterior shoulder dislocation. Comparison of six methods for identification of typical lesions. Acta orthopaedica Scandinavica. 1986 Aug:57(4):328-30
[PubMed PMID: 3788496]
[34]
Yoo JC, Lee YS, Tae SK, Park JH, Park JW, Ha HC. Magnetic resonance imaging appearance of a repaired capsulolabral complex after arthroscopic bankart repair. The American journal of sports medicine. 2008 Dec:36(12):2310-6. doi: 10.1177/0363546508322477. Epub 2008 Sep 5
[PubMed PMID: 18776021]
[35]
Chuang TY,Adams CR,Burkhart SS, Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy : the journal of arthroscopic
[PubMed PMID: 18375267]
[36]
Bottoni CR, Wilckens JH, DeBerardino TM, D'Alleyrand JC, Rooney RC, Harpstrite JK, Arciero RA. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. The American journal of sports medicine. 2002 Jul-Aug:30(4):576-80
[PubMed PMID: 12130413]
Level 1 (high-level) evidence
[37]
Resch H, Benedetto KP, Kadletz R, Oberhammer J. [Indications for the Bankart operation]. Aktuelle Traumatologie. 1985 Jun:15(3):122-6
[PubMed PMID: 2863957]
[38]
DeFroda S, Bokshan S, Stern E, Sullivan K, Owens BD. Arthroscopic Bankart Repair for the Management of Anterior Shoulder Instability: Indications and Outcomes. Current reviews in musculoskeletal medicine. 2017 Dec:10(4):442-451. doi: 10.1007/s12178-017-9435-2. Epub
[PubMed PMID: 28971317]
[39]
Davis DE,Abboud JA, Operative Management Options for Traumatic Anterior Shoulder Instability in Patients Younger Than 30 Years. Orthopedics. 2015 Sep;
[PubMed PMID: 26375529]
[40]
Ranalletta M, Rossi LA, Alonso Hidalgo I, Sirio A, Puig Dubois J, Maignon GD, Bongiovanni SL. Arthroscopic Stabilization After a First-Time Dislocation: Collision Versus Contact Athletes. Orthopaedic journal of sports medicine. 2017 Sep:5(9):2325967117729321. doi: 10.1177/2325967117729321. Epub 2017 Sep 25
[PubMed PMID: 28979919]
[41]
Taverna E, Garavaglia G, Ufenast H, D'Ambrosi R. Arthroscopic treatment of glenoid bone loss. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2016 Feb:24(2):546-56. doi: 10.1007/s00167-015-3893-0. Epub 2015 Dec 12
[PubMed PMID: 26658567]
[42]
Gouveia K, Abidi SK, Shamshoon S, Gohal C, Madden K, Degen RM, Leroux T, Alolabi B, Khan M. Arthroscopic Bankart Repair With Remplissage in Comparison to Bone Block Augmentation for Anterior Shoulder Instability With Bipolar Bone Loss: A Systematic Review. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2021 Feb:37(2):706-717. doi: 10.1016/j.arthro.2020.08.033. Epub 2020 Sep 7
[PubMed PMID: 32911004]
Level 1 (high-level) evidence
[43]
Haroun HK,Sobhy MH,Abdelrahman AA, Arthroscopic Bankart repair with remplissage versus Latarjet procedure for management of engaging Hill-Sachs lesions with subcritical glenoid bone loss in traumatic anterior shoulder instability: a systematic review and meta-analysis. Journal of shoulder and elbow surgery. 2020 Oct;
[PubMed PMID: 32807370]
Level 1 (high-level) evidence
[44]
Shin SJ, Kim RG, Jeon YS, Kwon TH. Critical Value of Anterior Glenoid Bone Loss That Leads to Recurrent Glenohumeral Instability After Arthroscopic Bankart Repair. The American journal of sports medicine. 2017 Jul:45(9):1975-1981. doi: 10.1177/0363546517697963. Epub 2017 Mar 23
[PubMed PMID: 28333542]
[45]
Dickens JF,Owens BD,Cameron KL,DeBerardino TM,Masini BD,Peck KY,Svoboda SJ, The Effect of Subcritical Bone Loss and Exposure on Recurrent Instability After Arthroscopic Bankart Repair in Intercollegiate American Football. The American journal of sports medicine. 2017 Jul;
[PubMed PMID: 28474965]
[46]
Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. Journal of shoulder and elbow surgery. 2011 Mar:20(2 Suppl):S61-9. doi: 10.1016/j.jse.2010.07.022. Epub 2010 Dec 9
[PubMed PMID: 21145262]
[47]
Lorenzetti A, Streit JJ, Cabezas AF, Christmas KN, LaMartina J 2nd, Simon P, Frankle MA. Bone Graft Augmentation for Severe Glenoid Bone Loss in Primary Reverse Total Shoulder Arthroplasty: Outcomes and Evaluation of Host Bone Contact by 2D-3D Image Registration. JB & JS open access. 2017 Sep 28:2(3):e0015. doi: 10.2106/JBJS.OA.17.00015. Epub 2017 Jul 28
[PubMed PMID: 30229222]
[48]
Neviaser TJ, The anterior labroligamentous periosteal sleeve avulsion lesion: a cause of anterior instability of the shoulder. Arthroscopy : the journal of arthroscopic
[PubMed PMID: 8442824]
[49]
Wischer TK, Bredella MA, Genant HK, Stoller DW, Bost FW, Tirman PF. Perthes lesion (a variant of the Bankart lesion): MR imaging and MR arthrographic findings with surgical correlation. AJR. American journal of roentgenology. 2002 Jan:178(1):233-7
[PubMed PMID: 11756126]
[50]
Kelley TD, Clegg S, Rodenhouse P, Hinz J, Busconi BD. Functional Rehabilitation and Return to Play After Arthroscopic Surgical Stabilization for Anterior Shoulder Instability. Sports health. 2022 Sep-Oct:14(5):733-739. doi: 10.1177/19417381211062852. Epub 2021 Dec 17
[PubMed PMID: 34918564]
[51]
Green MR, Christensen KP. Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 1993:9(4):371-4
[PubMed PMID: 8216566]
[52]
Sommaire C,Penz C,Clavert P,Klouche S,Hardy P,Kempf JF, Recurrence after arthroscopic Bankart repair: Is quantitative radiological analysis of bone loss of any predictive value? Orthopaedics
[PubMed PMID: 22884854]
[53]
Matsuki K, Sugaya H. Complications after arthroscopic labral repair for shoulder instability. Current reviews in musculoskeletal medicine. 2015 Mar:8(1):53-58. doi: 10.1007/s12178-014-9248-5. Epub
[PubMed PMID: 25532917]
[54]
Lützner J, Krummenauer F, Lübke J, Kirschner S, Günther KP, Bottesi M. Fuctional outcome after open and arthroscopic bankart repair for traumatic shoulder instability. European journal of medical research. 2009 Jan 28:14(1):18-24
[PubMed PMID: 19258206]
[55]
DeFroda SF, Mehta N, Owens BD. Physical Therapy Protocols for Arthroscopic Bankart Repair. Sports health. 2018 May/Jun:10(3):250-258. doi: 10.1177/1941738117750553. Epub 2018 Jan 3
[PubMed PMID: 29298132]
[56]
Fedorka CJ, Mulcahey MK. Recurrent anterior shoulder instability: a review of the Latarjet procedure and its postoperative rehabilitation. The Physician and sportsmedicine. 2015 Feb:43(1):73-9. doi: 10.1080/00913847.2015.1005543. Epub 2015 Jan 19
[PubMed PMID: 25598036]