[1]
Porter J, Guirao A, Cox IG, Williams DR. Monochromatic aberrations of the human eye in a large population. Journal of the Optical Society of America. A, Optics, image science, and vision. 2001 Aug:18(8):1793-803
[PubMed PMID: 11488483]
[2]
Read SA, Collins MJ, Carney LG. A review of astigmatism and its possible genesis. Clinical & experimental optometry. 2007 Jan:90(1):5-19
[PubMed PMID: 17177660]
[3]
Saw SM, Goh PP, Cheng A, Shankar A, Tan DT, Ellwein LB. Ethnicity-specific prevalences of refractive errors vary in Asian children in neighbouring Malaysia and Singapore. The British journal of ophthalmology. 2006 Oct:90(10):1230-5
[PubMed PMID: 16809384]
[4]
Namba H, Sugano A, Murakami T, Utsunomiya H, Nishitsuka K, Ishizawa K, Kayama T, Yamashita H. Age-Related Changes in Astigmatism and Potential Causes. Cornea. 2020 Nov:39 Suppl 1():S34-S38. doi: 10.1097/ICO.0000000000002507. Epub
[PubMed PMID: 33038156]
[5]
Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. Journal of cataract and refractive surgery. 2012 Dec:38(12):2080-7. doi: 10.1016/j.jcrs.2012.08.036. Epub 2012 Oct 12
[PubMed PMID: 23069271]
[6]
Kohnen T. Posterior corneal astigmatism. Journal of cataract and refractive surgery. 2013 Dec:39(12):1795. doi: 10.1016/j.jcrs.2013.10.017. Epub
[PubMed PMID: 24286837]
[7]
Royston JM, Dunne MC, Barnes DA. Measurement of posterior corneal surface toricity. Optometry and vision science : official publication of the American Academy of Optometry. 1990 Oct:67(10):757-63
[PubMed PMID: 2247298]
[8]
Módis L Jr, Langenbucher A, Seitz B. Evaluation of normal corneas using the scanning-slit topography/pachymetry system. Cornea. 2004 Oct:23(7):689-94
[PubMed PMID: 15448494]
[9]
Amesbury EC, Miller KM. Correction of astigmatism at the time of cataract surgery. Current opinion in ophthalmology. 2009 Jan:20(1):19-24. doi: 10.1097/ICU.0b013e328319c27a. Epub
[PubMed PMID: 19077825]
Level 3 (low-level) evidence
[10]
Mohammadi M, Naderan M, Pahlevani R, Jahanrad A. Prevalence of corneal astigmatism before cataract surgery. International ophthalmology. 2016 Dec:36(6):807-817
[PubMed PMID: 26909501]
[11]
Arriola-Villalobos P, Burgos-Blasco B, Fernández-Vigo JI, Ariño-Gutiérrez M, Burgos-Blasco P, Carmona-González D, Fernández-Pérez C. Biometry data and prevalence of corneal astigmatism in caucasian spanish candidates for cataract surgery. Journal francais d'ophtalmologie. 2021 Jan:44(1):76-83. doi: 10.1016/j.jfo.2020.03.025. Epub 2020 Nov 6
[PubMed PMID: 33162179]
[12]
Kaur M, Shaikh F, Falera R, Titiyal JS. Optimizing outcomes with toric intraocular lenses. Indian journal of ophthalmology. 2017 Dec:65(12):1301-1313. doi: 10.4103/ijo.IJO_810_17. Epub
[PubMed PMID: 29208810]
[13]
Núñez MX, Henriquez MA, Escaf LJ, Ventura BV, Srur M, Newball L, Espaillat A, Centurion VA. Consensus on the management of astigmatism in cataract surgery. Clinical ophthalmology (Auckland, N.Z.). 2019:13():311-324. doi: 10.2147/OPTH.S178277. Epub 2019 Feb 11
[PubMed PMID: 30809088]
Level 3 (low-level) evidence
[14]
Shimizu K, Misawa A, Suzuki Y. Toric intraocular lenses: correcting astigmatism while controlling axis shift. Journal of cataract and refractive surgery. 1994 Sep:20(5):523-6
[PubMed PMID: 7996408]
[15]
Statham M, Apel A, Stephensen D. Comparison of the AcrySof SA60 spherical intraocular lens and the AcrySof Toric SN60T3 intraocular lens outcomes in patients with low amounts of corneal astigmatism. Clinical & experimental ophthalmology. 2009 Nov:37(8):775-9. doi: 10.1111/j.1442-9071.2009.02154.x. Epub
[PubMed PMID: 19878222]
[16]
Nanavaty MA, Lake DB, Daya SM. Outcomes of pseudophakic toric intraocular lens implantation in Keratoconic eyes with cataract. Journal of refractive surgery (Thorofare, N.J. : 1995). 2012 Dec:28(12):884-9
[PubMed PMID: 23310966]
[17]
Gao Y, Ye Z, Chen W, Li J, Yan X, Li Z. Management of Cataract in Patients with Irregular Astigmatism with Regular Central Component by Phacoemulsification Combined with Toric Intraocular Lens Implantation. Journal of ophthalmology. 2020:2020():3520856. doi: 10.1155/2020/3520856. Epub 2020 Apr 30
[PubMed PMID: 32411427]
[18]
Srinivasan S, Ting DS, Lyall DA. Implantation of a customized toric intraocular lens for correction of post-keratoplasty astigmatism. Eye (London, England). 2013 Apr:27(4):531-7. doi: 10.1038/eye.2012.300. Epub 2013 Jan 25
[PubMed PMID: 23348728]
[19]
Ra H, Hwang HS, Kim HS, Kim MS, Kim EC. Toric intraocular lens implantation in cataract patients with corneal opacity. BMC ophthalmology. 2020 Mar 13:20(1):98. doi: 10.1186/s12886-020-01352-w. Epub 2020 Mar 13
[PubMed PMID: 32169054]
[20]
Stewart CM, McAlister JC. Comparison of grafted and non-grafted patients with corneal astigmatism undergoing cataract extraction with a toric intraocular lens implant. Clinical & experimental ophthalmology. 2010 Nov:38(8):747-57. doi: 10.1111/j.1442-9071.2010.02336.x. Epub
[PubMed PMID: 20497428]
[21]
Singh VM, Ramappa M, Murthy SI, Rostov AT. Toric intraocular lenses: Expanding indications and preoperative and surgical considerations to improve outcomes. Indian journal of ophthalmology. 2022 Jan:70(1):10-23. doi: 10.4103/ijo.IJO_1785_21. Epub
[PubMed PMID: 34937203]
[22]
Güçlü H, Akaray İ, Kaya S, Sattarpanah S, Çınar AC, Sakallıoğlu K, Korkmaz S, Gürlü V. Agreement of Anterior Segment Parameters Between Schiempflug Topography and Swept-Source Optic Coherence Based Optic Biometry in Keratoconus and Healthy Subjects. Eye & contact lens. 2021 Oct 1:47(10):539-545. doi: 10.1097/ICL.0000000000000787. Epub
[PubMed PMID: 33813587]
[23]
Goto S, Maeda N. Corneal Topography for Intraocular Lens Selection in Refractive Cataract Surgery. Ophthalmology. 2021 Nov:128(11):e142-e152. doi: 10.1016/j.ophtha.2020.11.016. Epub 2020 Nov 19
[PubMed PMID: 33221325]
[24]
Wang L, Koch DD. Intraocular Lens Power Calculations in Eyes with Previous Corneal Refractive Surgery: Review and Expert Opinion. Ophthalmology. 2021 Nov:128(11):e121-e131. doi: 10.1016/j.ophtha.2020.06.054. Epub 2020 Jun 29
[PubMed PMID: 32615201]
Level 3 (low-level) evidence
[25]
Montés-Micó R, Pastor-Pascual F, Ruiz-Mesa R, Tañá-Rivero P. Ocular biometry with swept-source optical coherence tomography. Journal of cataract and refractive surgery. 2021 Jun 1:47(6):802-814. doi: 10.1097/j.jcrs.0000000000000551. Epub
[PubMed PMID: 33315731]
[26]
Chung J, Bu JJ, Afshari NA. Advancements in intraocular lens power calculation formulas. Current opinion in ophthalmology. 2022 Jan 1:33(1):35-40. doi: 10.1097/ICU.0000000000000822. Epub
[PubMed PMID: 34854826]
Level 3 (low-level) evidence
[27]
Pantanelli SM, Kansara N, Smits G. Predictability of Residual Postoperative Astigmatism After Implantation of a Toric Intraocular Lens Using Two Different Calculators. Clinical ophthalmology (Auckland, N.Z.). 2020:14():3627-3634. doi: 10.2147/OPTH.S276285. Epub 2020 Oct 29
[PubMed PMID: 33154622]
[28]
Shukhaev SV, Boiko EV, Kudlakhmedov SS. [Comparative assessment of the accuracy of toric intraocular lens calculations]. Vestnik oftalmologii. 2022:138(1):5-12. doi: 10.17116/oftalma20221380115. Epub
[PubMed PMID: 35234415]
Level 2 (mid-level) evidence
[29]
Sheen-Ophir S, Reitblat O, Levy A, Assia EI, Kleinmann G. Deviation from the planned axis of three toric intraocular lenses. Scientific reports. 2022 Aug 12:12(1):13760. doi: 10.1038/s41598-022-17811-x. Epub 2022 Aug 12
[PubMed PMID: 35962050]
[30]
Lipsky L, Barrett G. Comparison of toric intraocular lens alignment error with different toric markers. Journal of cataract and refractive surgery. 2019 Nov:45(11):1597-1601. doi: 10.1016/j.jcrs.2019.06.013. Epub
[PubMed PMID: 31706514]
[31]
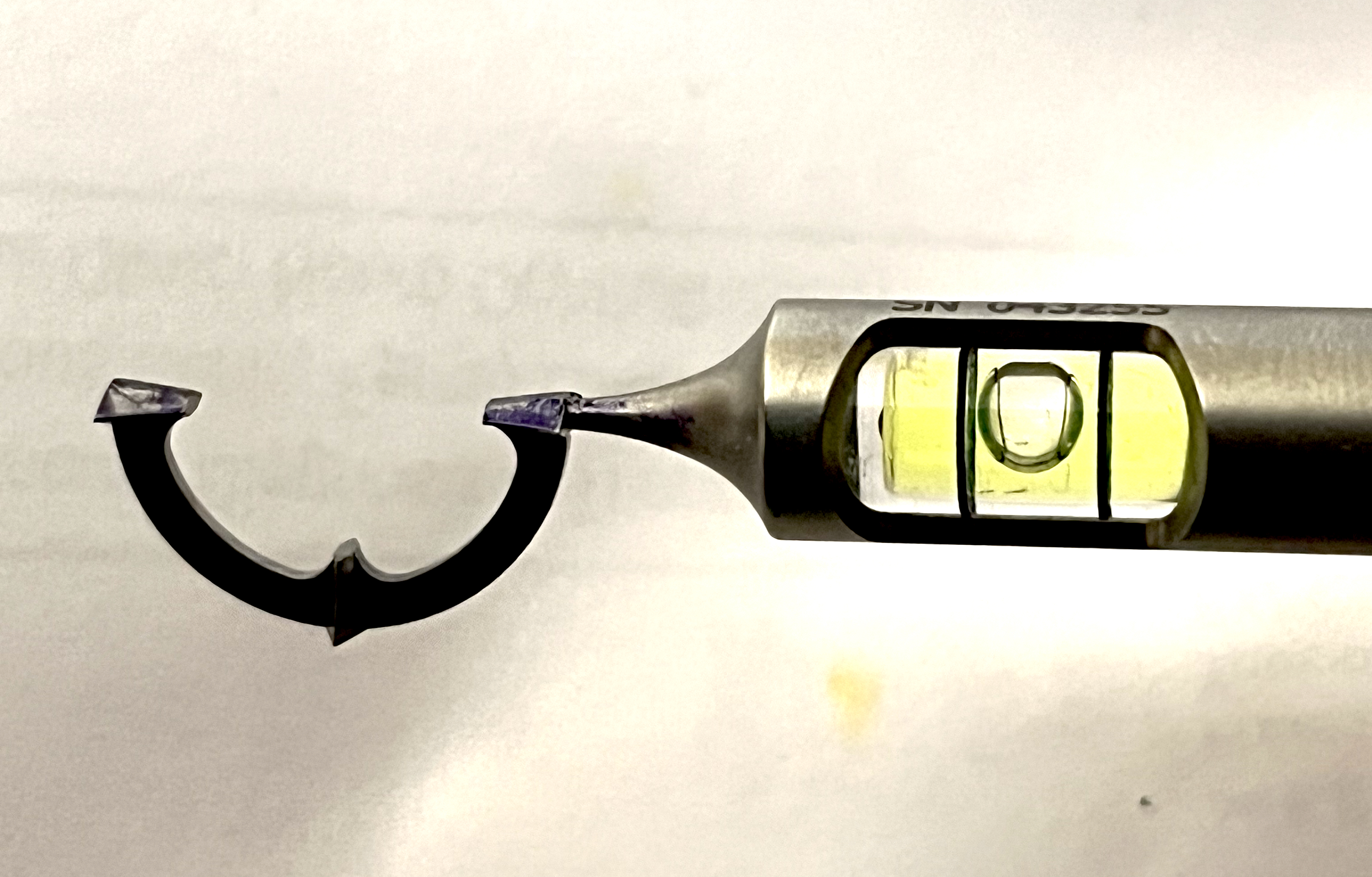
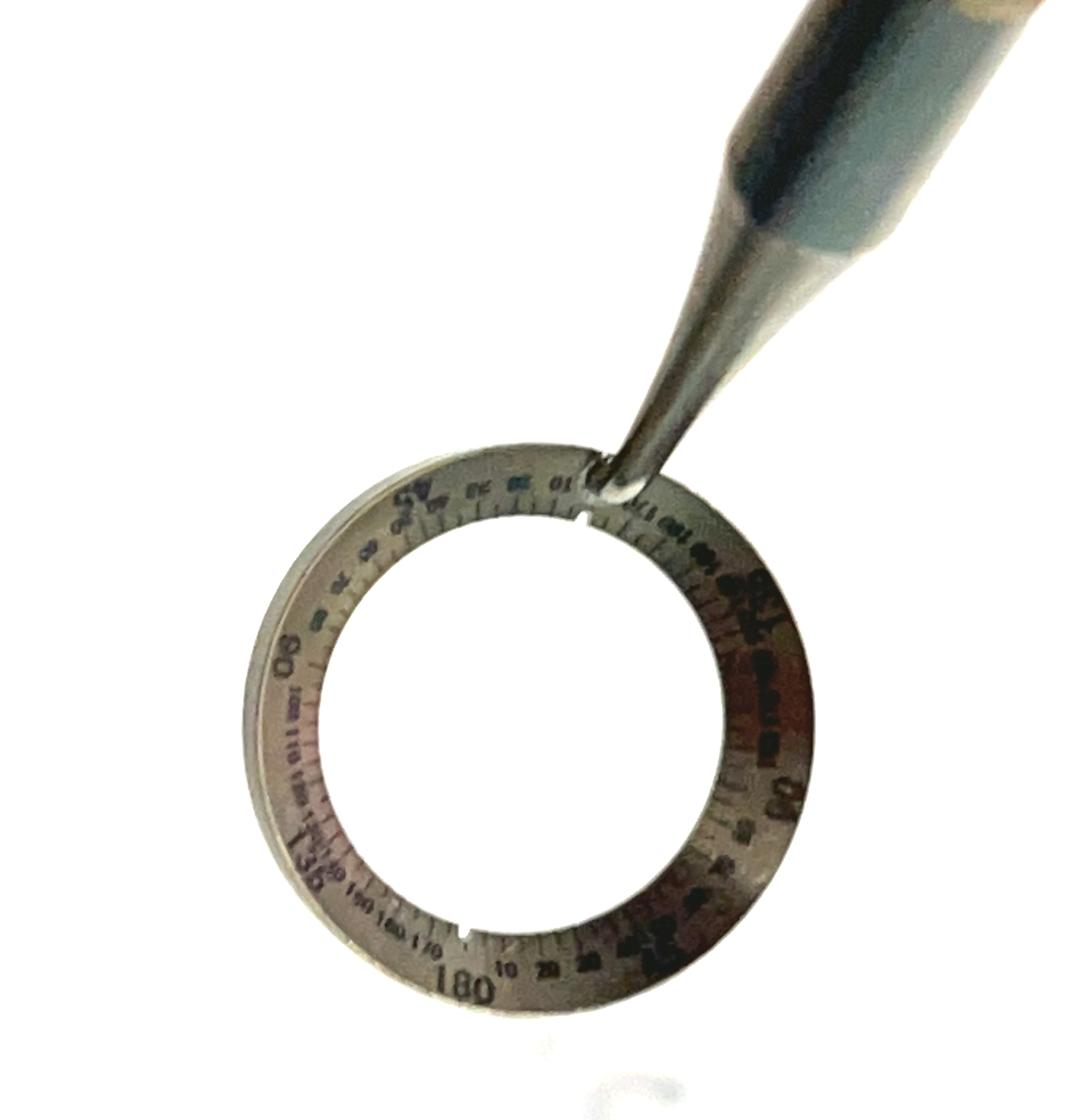
Farooqui JH, Koul A, Dutta R, Shroff NM. Comparison of two different methods of preoperative marking for toric intraocular lens implantation: bubble marker versus pendulum marker. International journal of ophthalmology. 2016:9(5):703-6. doi: 10.18240/ijo.2016.05.11. Epub 2016 May 18
[PubMed PMID: 27275425]
[32]
O'Neill BP, Diakonis VF, Tsaousis KT, Weinstock RJ. Outcomes of toric IOL implantation guided by iris-registered femtosecond laser capsulotomy markings. International ophthalmology. 2021 Dec:41(12):4009-4015. doi: 10.1007/s10792-021-01973-0. Epub 2021 Jul 27
[PubMed PMID: 34313930]
[33]
Zhou F, Jiang W, Lin Z, Li X, Li J, Lin H, Chen W, Wang Q. Comparative meta-analysis of toric intraocular lens alignment accuracy in cataract patients: Image-guided system versus manual marking. Journal of cataract and refractive surgery. 2019 Sep:45(9):1340-1345. doi: 10.1016/j.jcrs.2019.03.030. Epub
[PubMed PMID: 31470944]
Level 2 (mid-level) evidence
[34]
Raucau M, El Chehab H, Agard E, Lagenaite C, Dot C. Toric lens implantation in cataract surgery: Automated versus manual horizontal axis marking, analysis of 50 cases. Journal francais d'ophtalmologie. 2018 Jan:41(1):e1-e9. doi: 10.1016/j.jfo.2017.11.002. Epub 2018 Jan 10
[PubMed PMID: 29331293]
Level 3 (low-level) evidence
[35]
Miyake T, Kamiya K, Amano R, Iida Y, Tsunehiro S, Shimizu K. Long-term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. Journal of cataract and refractive surgery. 2014 Oct:40(10):1654-60. doi: 10.1016/j.jcrs.2014.01.044. Epub 2014 Aug 20
[PubMed PMID: 25149554]
Level 2 (mid-level) evidence
[36]
Prinz A, Neumayer T, Buehl W, Vock L, Menapace R, Findl O, Georgopoulos M. Rotational stability and posterior capsule opacification of a plate-haptic and an open-loop-haptic intraocular lens. Journal of cataract and refractive surgery. 2011 Feb:37(2):251-7. doi: 10.1016/j.jcrs.2010.08.049. Epub
[PubMed PMID: 21241906]
[37]
Shah GD, Praveen MR, Vasavada AR, Vasavada VA, Rampal G, Shastry LR. Rotational stability of a toric intraocular lens: influence of axial length and alignment in the capsular bag. Journal of cataract and refractive surgery. 2012 Jan:38(1):54-9. doi: 10.1016/j.jcrs.2011.08.028. Epub 2011 Nov 4
[PubMed PMID: 22055077]
[38]
Jung NY, Lim DH, Hwang SS, Hyun J, Chung TY. Comparison of clinical outcomes of toric intraocular lens, Precizon vs Tecnis: a single center randomized controlled trial. BMC ophthalmology. 2018 Nov 9:18(1):292. doi: 10.1186/s12886-018-0955-3. Epub 2018 Nov 9
[PubMed PMID: 30413154]
Level 2 (mid-level) evidence
[39]
Epitropoulos AT. Visual and Refractive Outcomes of a Toric Presbyopia-Correcting Intraocular Lens. Journal of ophthalmology. 2016:2016():7458210. doi: 10.1155/2016/7458210. Epub 2016 Jan 13
[PubMed PMID: 26885382]
[40]
Ribeiro FJ, Ferreira TB. Comparison of visual and refractive outcomes of 2 trifocal intraocular lenses. Journal of cataract and refractive surgery. 2020 May:46(5):694-699. doi: 10.1097/j.jcrs.0000000000000118. Epub
[PubMed PMID: 32358262]
[41]
Piovella M, Colonval S, Kapp A, Reiter J, Van Cauwenberge F, Alfonso J. Patient outcomes following implantation with a trifocal toric IOL: twelve-month prospective multicentre study. Eye (London, England). 2019 Jan:33(1):144-153. doi: 10.1038/s41433-018-0076-5. Epub 2018 Sep 6
[PubMed PMID: 30190549]
[42]
Koch DD, Jenkins RB, Weikert MP, Yeu E, Wang L. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. Journal of cataract and refractive surgery. 2013 Dec:39(12):1803-9. doi: 10.1016/j.jcrs.2013.06.027. Epub 2013 Oct 26
[PubMed PMID: 24169231]
[43]
Kodavoor SK, Divya J, Dandapani R, Ramamurthy C, Ramamurthy S, Sachdev G. Randomized trial comparing visual outcomes of toric intraocular lens implantation using manual and digital marker. Indian journal of ophthalmology. 2020 Dec:68(12):3020-3024. doi: 10.4103/ijo.IJO_465_20. Epub
[PubMed PMID: 33229690]
Level 1 (high-level) evidence
[44]
Uckmann MS, Stattin M, Zehetner C, Neururer S, Speicher L. [Comparison of two optical biometric devices for intraocular lens calculation]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2019 Mar:116(3):253-260. doi: 10.1007/s00347-018-0655-7. Epub
[PubMed PMID: 29372303]
[45]
Ortiz A, Galvis V, Tello A, Viaña V, Corrales MI, Ochoa M, Rodriguez CJ. Comparison of three optical biometers: IOLMaster 500, Lenstar LS 900 and Aladdin. International ophthalmology. 2019 Aug:39(8):1809-1818. doi: 10.1007/s10792-018-1006-z. Epub 2018 Aug 22
[PubMed PMID: 30136018]
[46]
Melles RB, Holladay JT, Chang WJ. Accuracy of Intraocular Lens Calculation Formulas. Ophthalmology. 2018 Feb:125(2):169-178. doi: 10.1016/j.ophtha.2017.08.027. Epub 2017 Sep 23
[PubMed PMID: 28951074]
[47]
Bayramlar H, Dag Y, Karadag R, Cakici O. An easy and practical method for toric intraocular lens implantation: marking corneal astigmatic axis at slit-lamp. International ophthalmology. 2017 Feb:37(1):179-184. doi: 10.1007/s10792-016-0250-3. Epub 2016 May 12
[PubMed PMID: 27169419]
[48]
Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4 corneal astigmatic marking methods. Journal of cataract and refractive surgery. 2012 Dec:38(12):2094-9. doi: 10.1016/j.jcrs.2012.07.039. Epub 2012 Oct 23
[PubMed PMID: 23098629]
[49]
Cha D, Kang SY, Kim SH, Song JS, Kim HM. New axis-marking method for a toric intraocular lens: mapping method. Journal of refractive surgery (Thorofare, N.J. : 1995). 2011 May:27(5):375-9. doi: 10.3928/1081597X-20101005-01. Epub 2010 Oct 15
[PubMed PMID: 20954592]
[50]
Hura AS, Osher RH. Comparing the Zeiss Callisto Eye and the Alcon Verion Image Guided System Toric Lens Alignment Technologies. Journal of refractive surgery (Thorofare, N.J. : 1995). 2017 Jul 1:33(7):482-487. doi: 10.3928/1081597X-20170504-02. Epub
[PubMed PMID: 28681908]
[51]
Ma JJ, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. Journal of cataract and refractive surgery. 2008 Oct:34(10):1631-6. doi: 10.1016/j.jcrs.2008.04.041. Epub
[PubMed PMID: 18812110]
[52]
Till JS, Yoder PR Jr, Wilcox TK, Spielman JL. Toric intraocular lens implantation: 100 consecutive cases. Journal of cataract and refractive surgery. 2002 Feb:28(2):295-301
[PubMed PMID: 11821213]
Level 3 (low-level) evidence
[53]
Ruhswurm I, Scholz U, Zehetmayer M, Hanselmayer G, Vass C, Skorpik C. Astigmatism correction with a foldable toric intraocular lens in cataract patients. Journal of cataract and refractive surgery. 2000 Jul:26(7):1022-7
[PubMed PMID: 10946194]
[54]
Chang DF. Repositioning technique and rate for toric intraocular lenses. Journal of cataract and refractive surgery. 2009 Jul:35(7):1315-6. doi: 10.1016/j.jcrs.2009.02.035. Epub
[PubMed PMID: 19545827]
[55]
Thomas BC, Khoramnia R, Auffarth GU, Holzer MP. Clinical outcomes after implantation of a toric intraocular lens with a transitional conic toric surface. The British journal of ophthalmology. 2018 Mar:102(3):313-316. doi: 10.1136/bjophthalmol-2017-310386. Epub 2017 Aug 3
[PubMed PMID: 28774937]
Level 2 (mid-level) evidence
[56]
Vale C, Menezes C, Firmino-Machado J, Rodrigues P, Lume M, Tenedório P, Menéres P, Brochado Mdo C. Astigmatism management in cataract surgery with Precizon(®) toric intraocular lens: a prospective study. Clinical ophthalmology (Auckland, N.Z.). 2016:10():151-9. doi: 10.2147/OPTH.S91298. Epub 2016 Jan 19
[PubMed PMID: 26855559]
[57]
Xiao XW, Hao J, Zhang H, Tian F. Optical quality of toric intraocular lens implantation in cataract surgery. International journal of ophthalmology. 2015:8(1):66-71. doi: 10.3980/j.issn.2222-3959.2015.01.12. Epub 2015 Feb 18
[PubMed PMID: 25709910]
Level 2 (mid-level) evidence
[58]
Espaillat A, Pérez O, Potvin R. Clinical outcomes using standard phacoemulsification and femtosecond laser-assisted surgery with toric intraocular lenses. Clinical ophthalmology (Auckland, N.Z.). 2016:10():555-63. doi: 10.2147/OPTH.S102083. Epub 2016 Mar 30
[PubMed PMID: 27099462]
Level 2 (mid-level) evidence