Continuing Education Activity
Physical and chemical lesions of the oral cavity are oftentimes discovered during routine examination and are a common finding as the oral cavity is continually exposed to trauma and chemical agents. These can range from traumatic occlusion, sharp occlusal anatomy, acidic and alkaline products or drugs, and food or drink at varying temperatures. This activity reviews the evaluation and management of physical and chemical lesions of the oral mucosa and highlights the role of the interprofessional team in evaluating and treating patients with these conditions.
Objectives:
- Describe common physical and chemical lesions of the oral mucosa.
- Identify the etiology of discovered physical and chemical lesions of the oral mucosa.
- Outline appropriate patient education to aid in the prevention of physical and chemical lesions of the oral mucosa.
- Review how interprofessional team collaboration and communication can improve patient outcomes for physical and chemical lesions of the oral mucosa.
Introduction
Physical and chemical lesions of the oral cavity are oftentimes discovered during routine examination and are a common finding as the oral cavity is continually exposed to trauma and chemical agents. These can range from traumatic occlusion, sharp occlusal anatomy, acidic and alkaline products or drugs, and food or drink at varying temperatures.[1] The following lesions will be discussed in this activity: traumatic fibroma, traumatic ulcerative granuloma with stromal eosinophilia, inflammatory papillary hyperplasia, thermal injury, and chemical burns, i.e., aspirin-induced oral lesions.
Etiology
Traumatic fibromas develop as a response to local trauma or irritation. Typically, they present on the buccal mucosa and tongue. These areas are repetitively subjected to trauma, specifically occlusal trauma.[2] They are also commonly found on the gingiva (reactive hyperplastic lesions of the oral cavity).[3]
Traumatic ulcerative granulomas with stromal eosinophilia (TUGSE) are longstanding ulcerative lesions that arise from mucosal trauma. [4]
Inflammatory papillary hyperplasia is generally classified as a type of denture stomatitis resulting from poor oral hygiene beneath an existing denture, ill-fitting dentures, or patients who continuously leave their dentures in place throughout the day and night.[5][6]
Foods or liquids can cause thermal injury with extreme temperatures.
Aspirin-induced oral lesions are chemical burns caused by the placement of acetylsalicylic acid (aspirin) directly on the oral mucosa in an attempt to alleviate pain.
Epidemiology
Traumatic fibromas can occur in any patient population; however, it has a predilection for middle-aged females.[7] A retrospective epidemiological analysis by Sonkodi et al. found that of 14,661 biopsies analyzed over a 54-year period, 32.4% were traumatic fibromas, which makes them the most lesions in the study.[8]
TUGSE can occur in any patient population but has a slight predilection for females between the sixth and seventh decades of life.[9] In infants, the presence of natal teeth at birth can lead to the ulceration of the tongue, which is known as Riga Fede disease, a variant of TUGSE.[10] Kanumuri discovered the incidence of neonatal teeth present at birth to be from 1 in 2,000 to 1 in 3,500 births, making the likelihood of TUGSE within infants extremely common.[11]
Inflammatory papillary hyperplasia characteristically affects patients wearing removable dental prostheses; however, some case reports states that the condition may be present in dentate individuals.[12] A study completed by Gual-Vaqués et al. in 2017 identified the prevalence of inflammatory papillary hyperplasia to be 4.4% in denture wearers, with ill-fitting dentures and a habit of smoking as the two greatest risk factors for developing this condition.[5]
Thermal injury can occur in any patient population and has no gender or age predilection. However, thermal injury to the oral mucosa is a frequent occurrence.
Aspirin-induced oral lesions can occur in any patient population who has access to aspirin. Chemical injury to the oral mucosa is common and has no gender predilection.
Pathophysiology
Traumatic fibromas arise from local irritation or injury, causing the tissue to progressively become more fibrotic.[3] As the tissue is attempting to protect itself, an inflammatory infiltrate can sometimes be noted, with localized ulceration or edema.
Traumatic ulcerative granulomas with stromal eosinophilia arise from severe chronic irritation or trauma. These ulcerations are typically deep and tend to illicit a robust eosinophilic response. The cytotoxic nature of the by-products of these cells causes mucosal degeneration resulting in the formation of the lesion.
Inflammatory papillary hyperplasia has an unclear pathogenic pathway but likely arises from poor oral hygiene resulting in a Candida infiltrate, triggering an inflammatory response beneath a denture.[5] A denture intimately contacting the tissue over extended periods exacerbates the inflammatory response.
Thermal injury is caused by extreme temperatures resulting in injury to the tissue. As a result, there is sloughing of the epithelium and exposure of the highly vascularized connective tissue, which accounts for the erythematous appearance.
Chemical burns are caused by the alkaline or acidic environment from chemical products or by-products that are cytotoxic to tissue. As tissue necrosis, it sloughs, revealing connective tissue which is highly vascularized due to an increased inflammatory response to the area.
Histopathology
Traumatic fibromas histologically present as stratified squamous epithelium, which may demonstrate hyperkeratosis overlying dense fibrous connective tissue.[3]
Traumatic ulcerative granulomas with stromal eosinophilia usually present histologically with granulomatous tissue extending deep into the mucosal layers.[13] Heavy inflammatory infiltrates are noted, with numerous eosinophils noted throughout. Small lymphocytes, histocytes, and large lymphoid cells are also often noted.[4]
Inflammatory papillary hyperplasia histologically demonstrates epithelial hyperplasia with papillary projections with varying degrees of subepithelial chronic inflammation and fibrosis.[5]
Thermal injuries and chemical burns correlate with patient history and usually resolve before a biopsy is indicated.
History and Physical
Traumatic fibromas have various clinical presentations, and they are always preceded by localized irritation or trauma. Typically, fibromas present as smooth, nodular, sessile lesions measuring up to 2 cm in diameter.[14] These lesions are firm and are usually the same color as the surrounding oral mucosa with well-defined borders, potentially presenting with an associated traumatic ulcer.[15]
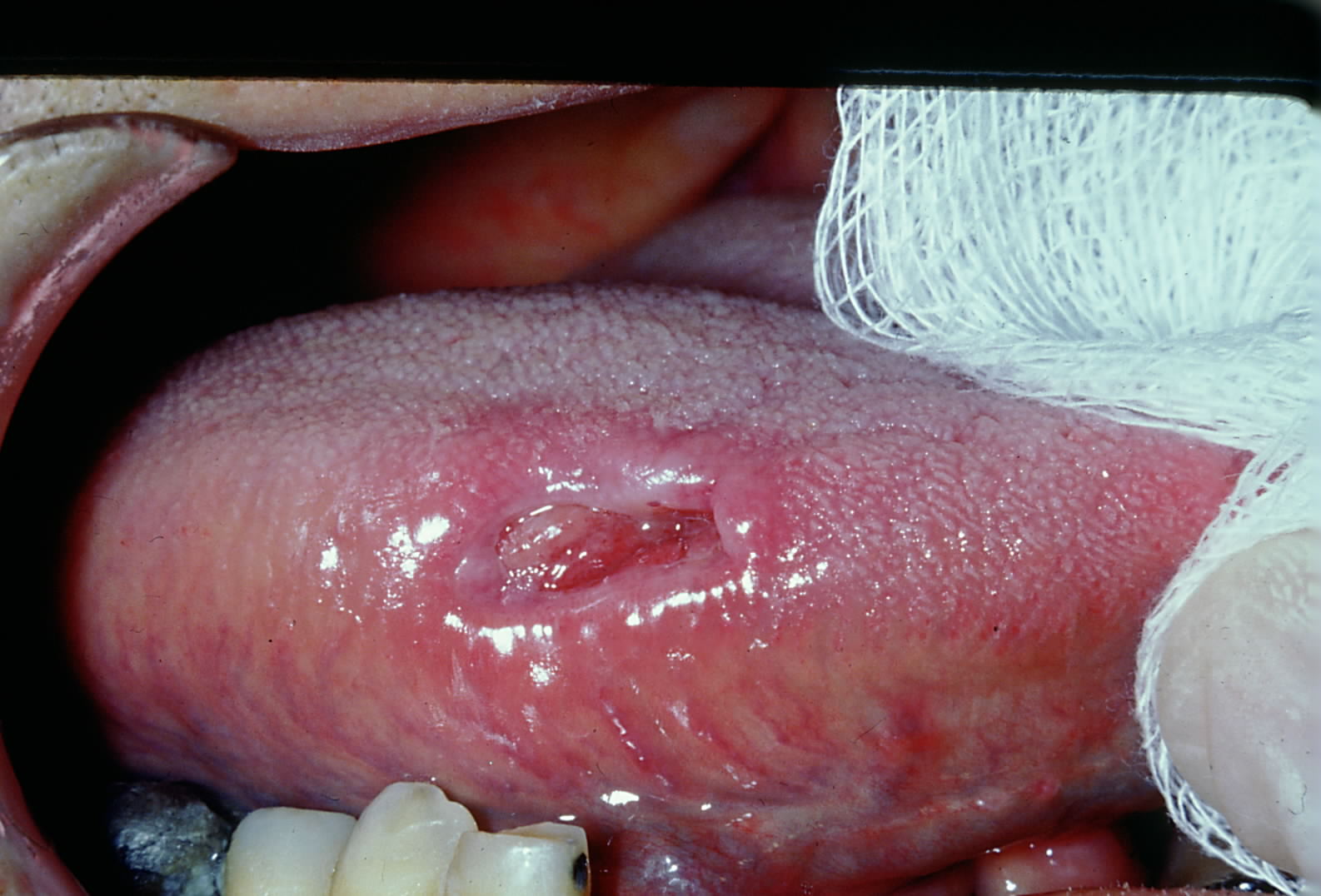
TUGSE presents clinically as self-limiting, solitary ulceration with a fibrinopurulent membrane and elevated indurated margins.[16][17] These lesions can present clinically, like squamous cell carcinoma.[18]
Inflammatory papillary hyperplasia presents as a few to innumerable small, reddened concentric papillomas on the hard palate.[6] These lesions have been described as “mulberry-like” in appearance. The appearance and number of lesions depend on the degree of inflammation.
Thermal injuries usually present with localized or diffuse tissue damage.[19] Depending on the extent of damage, these lesions present with ulcerations or erosions on the affected tissues. They are typically pink to red in color with an ulcerated or diffuse border.
Aspirin-induced oral lesions present as an ulcerated aphthous-like white lesion caused by an immune response to the acidic components of aspirin.[20] The tissue surrounding the lesion normally will slough off, oftentimes leaving localized erythema.
Evaluation
Traumatic fibromas should be evaluated to determine a definitive diagnosis via surgical excision.[14] Histological evaluation generally reveals hyperplastic and hyperkeratotic epithelium overlying dense fibrous tissue.[15]
TUGSE can mimic several malignant processes and, therefore, should be biopsied to determine a definitive diagnosis if the lesion persists for two weeks after removing any irritant.[21] Histologically, these lesions present with ulcerated epithelium with fibrinopurulent exudate over an inflamed stroma.[22] Additionally, there is a granulomatous infiltrate rich in lymphocytes, histiocytes, and eosinophils.[13]
Inflammatory papillary hyperplasia can present as very few or multiple lesions that require evaluation. Questions should be asked of the patient to determine how long they leave their removable dental prosthesis in their mouth each day. Additionally, the prosthesis should be evaluated for proper fit.
Thermal injuries should be evaluated by interviewing the patient to determine the etiology of the lesion.
Aspirin-induced oral lesions should be evaluated by patient interview to pinpoint the etiology of the lesion, as sloughing of the oral mucosa can potentially mimic an autoimmune or malignant process.
Treatment / Management
Traumatic fibromas are generally removed via excisional biopsy and enucleation to prevent a recurrence.[14] This treatment is ideal, as it can be completed under local anesthesia. If a source of irritation is identified and removed, it will limit recurrence.[23]
TUGSE can be treated with an antibiotic to reduce the microbial load that is likely present on the lesion surface.[24] This lesion should be monitored closely, and the etiologic agent of trauma – malposed teeth, sharp cusps on teeth, local irritants – should be removed. If the lesion itself does not resolve in two weeks, a biopsy is indicated to develop a definitive diagnosis. In infants, the neonatal teeth can be smoothed or reshaped under local anesthesia if indicated.
Inflammatory papillary hyperplasia occasionally requires no treatment, whereas others may involve surgical excision of inflamed papillary tissue.[6] At times, a fabrication of a new removable dental prosthesis is indicated.
Thermal injuries are typically self-limiting and will resolve as long as the site is protected from repeated trauma or additional exposure to extreme temperatures. Palliative treatment is recommended from topical benzocaine cream or petroleum jelly to protect the ulcerated mucosa. There is no standard of care for intraoral burns; however, management of inflammation or pain is always indicated.[25]
Aspirin-induced oral lesions are chemical burns, which typically only require local palliative measures for healing, similar to chemical burns.[26] The one key point for treatment and management is patient education, as aspirin only provides analgesia if ingested, not by simply placing it on the mucosa.
Differential Diagnosis
Traumatic Fibroma
- Any benign mesenchymal tumor (lipoma, neuroma, neurilemmoma)
- Pyogenic granuloma
- Peripheral ossifying fibroma, if on the gingiva
Traumatic Ulcer
- Recurrent aphthous ulcer
- Herpetic ulceration
- Traumatic eosinophilic granuloma
- Squamous cell carcinoma
- Ulcerative mucosal disease, e.g., lichen planus
Inflammatory Papillary Hyperplasia
- Secondary pseudomembranous candidiasis
- HPV-associated papillary lesions
- Erythema migrans
Thermal Injury
- Recurrent aphthous ulcer
- Herpes simplex virus
- Behçet’s disease
Aspirin-induced Oral Lesions
- TUGSE
- Traumatic ulceration
- Recurrent aphthous ulcer
Prognosis
Traumatic fibromas have an excellent prognosis, as they are a reactive overgrowth of normal tissues. With appropriate surgical excision and removal of any source of local irritation, their recurrence rate is low.[27]
TUGSE has a good prognosis, as the lesion itself is self-limiting and aggressive treatment typically is not indicated.[28] That said, if the offending agent is not removed, a traumatic ulcer, if not TUGSE, will be expected to recur.
Inflammatory papillary hyperplasia has a good prognosis. Discontinuing the use of ill-fitting dentures and allowing the tissue an appropriate time to heal has shown to resolve the condition.[29] Patient education is key to ensuring the patient reduces their risk of recurrence; the emphasis should be placed on removing their dentures daily to allow cleansing and rest of the oral tissues.
Thermal injuries have a great prognosis, as the oral mucosa is resilient and will heal on its own, granted no additional thermal challenge is introduced.
Aspirin-induced oral lesions have a great prognosis, as the oral mucosa will heal with removing the aspirin from the tissue. However, recurrence is dependent on the patient discontinuing this habit.
Complications
Traumatic fibromas typically arise from parafunctional habits, such as chewing of the cheeks or tongue or from a local irritant or trauma.[30] Without the resolution of these habits or sources of trauma, traumatic fibromas are likely to recur. Additionally, since they are generally removed by surgical excision. Encouraging the patient to continue optimal oral hygiene is paramount to promote healing.
TUGSE can present as a painful lesion that shares many features of squamous cell carcinoma.[28] Due to this, lesions that do not resolve in 2 weeks with the removal of the etiologic agent should be biopsied for a definitive diagnosis. In infants presenting with Riga Fede disease, patient management may be difficult and should be referred to a pediatric dentist.
Inflammatory papillary hyperplasia does not have any malignant potential but can be mistaken as a potentially malignant process.[31] Patients with this condition should be encouraged to allow proper healing time for their oral tissues. Treatment is very patient-dependent, as meticulous oral hygiene is required for the resolution of this condition.
Thermal injuries are typically painful and will likely become irritated by the patient’s tongue or other oral tissues. Patients should be encouraged to minimize additional trauma to the area.
Aspirin-induced oral lesions are painful and can become exacerbated without cessation of the habit. Therefore, patients should be encouraged to minimize additional trauma to the area as much as possible.
Deterrence and Patient Education
Traumatic fibromas should be brought to the patient’s attention once identified and biopsied for a definitive diagnosis. Patients should be made aware of the potential sources for these lesions.
TUGSE is a self-limiting disease that requires immediate attention, as it is a reactive and inflammatory process that can mimic malignant processes. Patients should be counseled on parafunctional habits or potential local irritants that could increase recurrence.
Inflammatory papillary hyperplasia was found to occur at its highest incidence in patients who left their dentures in place for the entire night.[6] Patients should be instructed to remove their removable dental prosthesis between six and eight hours each day to properly clean the oral tissues and relieve oral tissues of any possible pressure the prosthesis could induce.
Thermal injuries can be avoided by patient education and patient compliance. Patients should be encouraged to ensure foods or liquids are at an appropriate temperature for consumption to avoid potential harm to the tissues.
Aspirin-induced oral lesions are self-resolving once the patient eliminates the use. Patients should be educated on the lack of efficacy in placing aspirin directly on the oral mucosa, as it does not provide any analgesia but rather induces damage and pain.[26]
Pearls and Other Issues
Though this list is non-exhaustive, it provides the practitioner with a baseline understanding of the possible etiologies and tools for differentiating between common physical and chemical lesions of the oral mucosa. If any lesion is thought to be suspicious, or if an etiology cannot be determined, referral for biopsy is indicated for definitive diagnosis.
Enhancing Healthcare Team Outcomes
Physical and chemical lesions of the oral mucosa are common conditions that any interprofessional healthcare team can manage. Identifying the etiology of such lesions is important in determining the appropriate treatment modalities to improve patient care. If the etiology of the lesion cannot be identified, or if the lesion persists beyond two weeks, appropriate referral to a healthcare specialist is warranted for subsequent diagnostic procedures. All interprofessional team members are integral in identifying these lesions and initiating treatment, referral, and/or education in a timely manner to ensure optimal patient care. This interprofessional approach will drive better patient outcomes. [Level 5]